5.4: Approach to Bone and Joint x-rays
- Page ID
- 14809
Image Acquisition:
Optimal image exposure should allow you to see the cortex of the bone distinctly and differentiate between cortex and medulla without difficulty.
The standard views are AP (anterior-posterior) and lateral. These two views are taken at right angles (orthogonal) to each other. If these images are not helpful, ancillary views such as oblique views, or special views such as, an axillary or carpal tunnel view, may be required based upon the clinical scenario.
Stress views i.e. a force is applied to a bone or joint to determine if an injury is present, such as, a subtle avulsion or a suspected tendon or ligament tear causing joint instability. These are acquired as special requests and should be performed in a manner that minimizes patient pain and discomfort.
At least one joint space should be visible in relation to the suspected bone injury. Additional x-ray views and views of another adjacent joint space may be required in some circumstances.
Comparison views to the contralateral, normal bone, or joint, may be required, this is especially true if a subtle growth plate injury is suspected in a child. Comparison views should not be ordered routinely, but should be used if clinically necessary.
It is important to remember that some bone and ligament injuries occur as a common pattern of multiple injuries i.e. the Colle fracture of the distal radius is often associated with an avulsion fracture of the ulnar styloid. Ankle ligament injuries and fractures often occur in a sequence i.e. medial malleolar avulsion fracture (or medial ligament tear), interosseous ligament tear between the tibia and fibula, and a subsequent oblique fracture of the proximal fibula (Maisonneuve fracture complex). Keep this in mind as you encounter various patients and you will develop knowledge and experience of these associated bone and soft tissue injuries.
Fractures usually present as a lucent line on x-rays involving the cortex and medulla of the bone that can be followed from one cortex to the opposite cortex with varying degrees of displacement and malalignment of the involved bone.
There are some fractures that may be associated with bone ischemia and avascular necrosis i.e. capital femoral fractures and scaphoid fractures. Be aware of this and learn the importance of aggressive and pre-emptive management for these patients.
Anatomic Locations in Bone
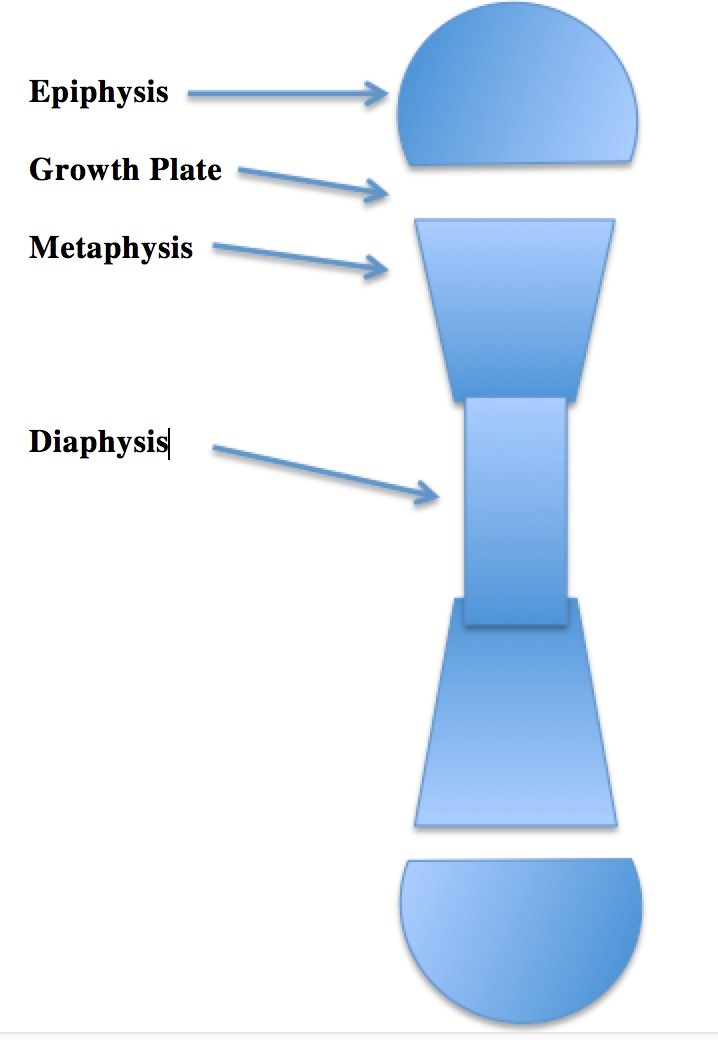
| Diaphysis | Middle of the bone |
| Metaphysis | Flared region of the bone, between the epiphysis and the diaphysis |
| Epiphysis | The end of the bone, usually this area is associated with actively growing bone at the epiphyseal plate in children |
| Intra-articular | The joint space |
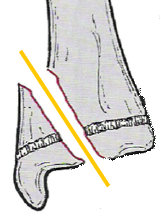
Complete Fracture:
Fracture line completely traverses the bone effecting the cortex and medulla.
| Transverse | Across the long axis of the bone
i.e. 90 degrees to the long axis of the bone |
| Oblique | Passes across the bone with an angle of less than 90 degrees |
| Spiral | Passes around the bone in a cork screw path |
| Longitudinal | Fracture is oriented parallel to the long axis of the bone |
| T-Shaped | There are two fractures, a longitudinal portion and a transverse or oblique portion |
| Comminuted | More than two bone fragments |
Table 5.2 Types of complete bone fractures
Incomplete Fracture:
The fracture does not complete traverse the bone.
| Bowing | The bone is bent but not fractured |
| Buckle | One cortex is bucked outward, the buckle is like a fold
The opposite cortex may be fractured or may be intact |
| Greenstick | One cortex is compressed into denser bone while the contralateral cortex is fractured |
| Salter-Harris | This classification describes the various epiphyseal and metaphyseal findings to describe the degree of damage to the actively developing growth plate |
Table 5.3 Types of Incomplete Bone Fractures
Salter-Harris
Some fractures in children involve the growth plate and the adjacent metaphysis of the bone. These fractures have been categorized using the Salter-Harris classification.
| Type | Description | Image |
| I | The fracture plane extends completely through the growth plate. This type of fracture can be minimally displaced, making detection challenging. Repeated x-rays in 7 days will demonstrate periosteal new bone if a subtle fracture is suspected.
5 – 7% frequency. Good prognosis. |
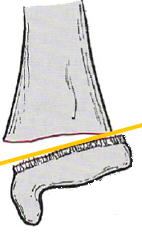 |
| II | The fracture plane leaves a small, triangular or quadrangular portion of the metaphysis in contact with the growth plate. This is the most common type of Salter-Harris injury.
75% frequency. Good prognosis. |
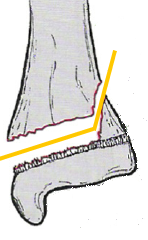 |
| III | A quadrangular fragment of the epiphysis is isolated from the adjacent bone.
7 – 10% frequency. Poorer prognosis. |
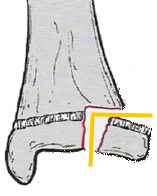 |
| IV | A triangular fragment of epiphysis, growth plate, and metaphysis is separated from the adjacent bone.
10% frequency. Poorer prognosis. |
 |
| V | This injury is focal and results in delayed abnormal bone growth in a focal region of the bone due crushing type of damage to the growing bone.
1% frequency. Worst prognosis |
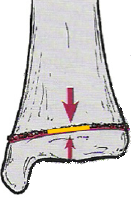 |
Table 5.4 Classification of Salter-Harris Fractures
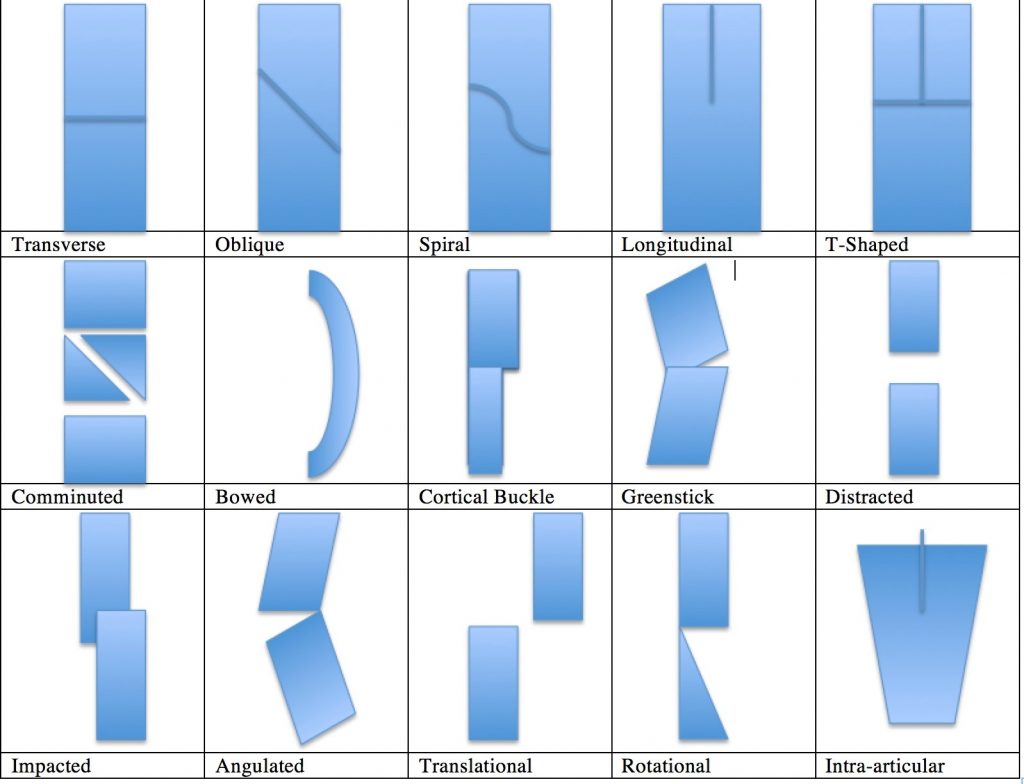
Displacement
Describe based upon the location and orientation of the distal bone fragment.
| Distracted | The bone ends are quite displaced away from each other |
| Impacted | The bone ends are collapsed into each other |
| Angulated | There is an angle that can be described. The angle can be measured and describe based upon the apex of the angle seen. Some also describe the angle based upon the normal angulation of the bone in the region and whether this has been altered i.e. the bone is varus or valgus in comparison to the normal |
| Translational | The distal fragment is shifted away from normal |
| Rotational | The distal fragment is spun out of normal alignment |
| Pathologic | The bone at the fracture site is abnormal due to infection, congenital bone abnormality, a metabolic bone abnormality, or malignancy. Fractures that are the result of these conditions are pathologic |
| Avulsion | A small fragment of bone (triangular, quadrangular) is pulled off of the parent bone by a ligament or tendon. The ligament is usually intact as the bone was the greatest point of weakness that gave way |
| Stress Fractures | Repetitive, low-grade injury to a bone can lead to stress fracture. Frequent sites are the ventral tibial cortex and the metatarsals but they can occur elsewhere. These are most often seen in young active patients who complain of chronic, focal, bone pain |
Table 5.5 Types of bone displacements
Descriptors of Displacement
Additional Descriptors
| Subluxation | Joint alignment is disrupted but the cartilaginous ends of the bones at the joint space are still in contact with each other |
| Dislocation | The bones have been displaced and the cartilaginous ends of the bones no longer are in proximity to each other |
| Open Fracture | There is a discontinuity of the skin and underlying soft tissues that allows air to be in contact with the bone and/or the joint space. This type of injury increases the risk for infections such as, septic arthritis and osteomyelitis. There may be an underlying fracture or dislocation, but this is not always the case |
Intra-articular, Salter-Harris, and open fractures require enhanced treatment and close clinical follow-up to minimize the possibility of undetected abnormal healing, or infection, that can lead to heightened morbidity or mortality.
Joint, Arthritic Conditions
The two most common arthritic conditions encountered are degenerative (osteoarthritis) and inflammatory (rheumatoid) arthritis. The radiographic appearance of these arthridites will vary based upon severity and distribution. The longer the condition has been present the worse the imaging changes will usually be unless treatment has been instituted. There are a variety of arthritic conditions that can be encountered. Using laboratory assessment, clinical parameters, and imaging features often one can shorten the differential diagnostic possibilities. Osteoarthritis is usually quite distinct from erosive arthritides, i.e. rheumatoid, gout, calcium pyrophosphate, psoriatic, etc. It is beyond the scope of this work to discuss the imaging features of all of the various possible arthritides. The two most common arthritides encountered will be compared using the ABCDS method detailed below.
ABCDS method is one way to approach bone and joint arthritis.
A- Alignment of bones
B- Bones – bone mineralization, new bone formation, erosions, osteophytes, fractures
C- Cartilage – joint space alignment and narrowing, joint calcifications, effusions
D- Distribution of disease – Some distribution of bone involvement is characteristic for certain diseases i.e. hip and knee osteoarthritis, first metatarsal-phalangeal gout, interphalangeal joint rheumatoid arthritis, etc.
S- Soft tissues – swelling and calcifications
Osteoarthritis
Bone alignment is usually normal until the degenerative changes become severe. The bone density is usually within normal limits unless the patient becomes sedentary due to severe joint pain. Erosions of the bone are uncommon in osteoarthritis for the most part, but subchondral cysts can be seen in the joint space. They are not true erosions. The hallmarks of osteoarthritis are joint space narrowing, sub-chondral bone sclerosis, and osteophyte formation. The arthritic changes are asymmetric in the joint and with the contralateral body part. The soft tissues are not usually effected unless the patient develops a joint effusion. Joint crepitations may be felt with range of motion but the joints are not usually red or warm.
Erosive Arthritis (Rheumatoid)
Bone malalignment can be minimal to severe based upon severity of the arthritis. Some deformities of joints i.e. swan neck and hitch hiker thumb deformities are characteristic of rheumatoid arthritis. Often the visible joint deformity is quite noticeable with rheumatoid arthritis as the disease progresses. The bone density is usually diminished with rheumatoid arthritis, this is most noticeable in the peri-articular bone which is preferentially reduced in density. Rheumatoid arthritis is characteristically very symmetrical in distribution. There is joint space narrowing and peri-articular erosions with the arthritis. Often, the erosions are subtle and small. The hands are often involved early and erosions can be seen in the PIP and MCP joints. Rheumatoid arthritis often effects a wide variety of joints that are not weight bearing and it can involve almost any joint in the body including the acromio-clavicular, gleno-humeral, elbow, and upper cervical spine joints. The soft tissues are often swollen, red, and may feel warm to touch. Effusions may also be palpable.
Attributions
Figure 5.15 Anatomic Locations in Bone by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 5.16 Illustrations of Displacement by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.


