4.14: Shoulder Pain
- Page ID
- 59141
The rotator cuff is a group of tendons that holds the shoulder joint in place allowing people to lift their arm and reach overhead. Rotator cuff related shoulder pain is a term that encompasses a spectrum of conditions including subacromial pain syndrome, rotator cuff tendinopathy, and symptomatic partial and full thickness rotator cuff tears (Lewis, 2016).
Pathophysiology
Rotator Cuff Related Shoulder Pain
In some cases of rotator cuff disorders pathoanatomical explanations do not account for why pain persists, which is why it is important to take into account patient-specific assessment findings and psychosocial factors (Wylie et al., 2016; Wong et al., 2020). In other cases, pathological changes (e.g., fibrosis, interstitial collagen deposition, and inflammatory cells) may be associated with sensorimotor declines, and symptomatic rotator cuff disorders (Fouda et al., 2017).
Frozen Shoulder
Frozen shoulder also known as “Adhesive Capsulitis” is classified as idiopathic (primary) or following shoulder surgery or trauma (secondary). Traditionally it has been taught that regardless of therapeutic intervention the affected shoulder will eventually improve or “thaw out”. This long held idea of complete resolution without treatment for frozen shoulder is unfounded. In most cases an understanding of the pathophysiology of frozen shoulder will lead to improved treatment outcomes, reduced pain and suffering associated with the condition (Wong et al., 2017).
The progression of the frozen shoulder is a complicated process, involving a cascade of molecular and cellular events. Connective tissue fibrosis and storage of leukocytes and chronic inflammatory cells is thought to play a fundamental role. Ongoing inflammation feeds into a cycle and upregulation of pro-inflammatory cytokine production, namely transforming growth factor beta (TGF-β). This may be further perpetuated by sympathetic dominance of autonomic balance, and neuro-immune activation (Pietrzak, 2016).
Clinical Examination
A thorough health history intake can be done to gather information about patients’ limitations, course of pain, and prognostic factors for delayed recovery (e.g., low self-efficacy, fear of movement, ineffective coping strategies, fear-avoidance, pain catastrophizing) and answers to health-related questions. Screen patients to identify those with a higher likelihood of serious pathology/red flag conditions. Then undertake a physical examination: neurological screening test, assess mobility and/or muscle strength.
Outcome Measurements
Incorporate one or more of the following outcome measurements when assessing and monitoring patient progress:
- Self-Rated Recovery Question
- Patient-specific Functional Scale
- DASH Outcome Measure
- Upper Extremity Functional Index
- Western Ontario Rotator Cuff (WORC) Index
Neurovascular Assessment
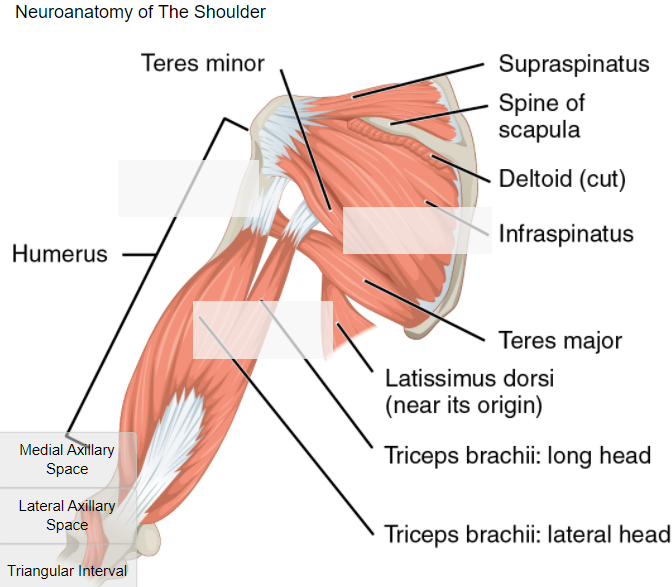
Medial axillary space – The Axillary space is bounded by teres major muscle, teres minor muscle and humerus. The long head of triceps brachii splits this area into medial and lateral groups. Scapular circumflex artery and scapular circumflex vein pass through it.
Lateral axillary space – The axillary nerve and posterior circumflex humeral artery can be irritated by soft tissue structures. Symptoms include axillary nerve related weakness of the deltoid muscle, resulting in a reduction in shoulder abduction. The pain from axillary neuropathy is usually dull and aching rather than sharp and increases with increasing range of motion. Many people notice only mild pain but considerable weakness when they try to use the affected shoulder.
Triangular interval – The radial nerve and profunda brachii artery pass through the triangular interval, on route to the posterior compartment of the arm. The triceps brachii has potential to irritate the radial nerve in the triangular interval.
Drag and Drop: Anatomy Review
Physical Examination
Incorporate one or more of the following physical examination tools and interpret examination results in the context of all clinical exam findings.
- Apprehension Test (Crank Test)
- Hawkins Kennedy Impingement Test
- Acromioclavicular Shear Test
- Speed’s Test
- Yergason’s Test
- Supraspinatus Test (Empty Can Test)
- Drop Arm Test (Codman’s Test)
- Apley’s Scratch Test
- Sulcus Sign Test
- Neer’s Test
- Roo’s Test (EAST)
- Slap Lesion Cluster
- Load & Shift – Anterior
- Scapular Retraction
- AC Crossbody Adduction Test (Acromioclavicular Crossover)
- Posterior Capsule Tightness
- Serratus Anterior Strength Test (Punch Out)
- Jerk Test (Posteroinferior Labral Tear)
- Scapular Load Test
- O’Brien Test (Active Compression Test)
- Lift-off Sign
- Belly Press Test
- Painful Arc Test
Jeremy Lewis: Rotator Cuff Shoulder Pain – Exercise is as effective as surgery
Treatment
Education
Provide reassurance and patient education on condition and management options and encourage the use of active approaches (lifestyle, physical activity) to help manage symptoms.
Manual Therapy
A massage therapy treatment plan should be implemented based on patient-specific assessment findings and patient tolerance. Structures to keep in mind while assessing and treating patients suffering from shoulder pain may include neurovascular structures and investing fascia of:
- Rotator Cuff (subscapularis, infraspinatus, teres minor, supraspinatus)
- Pectoral Region (pectoralis major, pectoralis minor, serratus anterior and subclavius)
- The Upper Arm (biceps brachii, brachialis, coracobrachialis, triceps brachii)
- Deltoid Muscle Group (anterior, middle, posterior)
- Erector Spinae (iliocostalis, longissimus, spinalis) & Multifidus
- External Obliques, Internal Obliques, and Transverse Abdominal
- Thoracolumbar Fascia, Latissimus Dorsi and Teres Major
- Quadratus Lumborum
Self-Management Strategies
Massage therapists not only provide hands-on treatment they can also develop self-management programs to help patients manage symptoms. Simple home-care recommendations such as stretching and strengthening exercises may be useful for people with shoulder pain.
Prognosis
Prognosis is favorable when therapists use a multidisciplinary approach to treatments. Exercise is the mainstay of treatment; a strong recommendation may be made regarding the effectiveness of manual therapy when combined with exercise for subacromial shoulder pain (Pieters et al., 2020). Several systematic reviews support the use of exercise and manual therapy for the treatment of shoulder pain (Hawk et al., 2017; Steuri et al., 2017).
Massage Therapeutics: How to treat frozen shoulder: Massage video with Maria Natera
Contemporary multimodal massage therapists are uniquely suited to incorporate a number of rehabilitation strategies for acute and chronic shoulder pain based on patient-specific assessment findings including, but not limited to:
- Manual Therapy (soft tissue massage, neural mobilization, joint mobilization)
- Education that is Person-Centered (e.g., biopsychosocial model of health and disease, self-efficacy beliefs, active coping strategies)
- Stretching & Loading Programs (e.g., concentric, eccentric, isometric exercises)
- Hydrotherapy (hot & cold)
- Self-Management Strategies (e.g., engaging in physical activity and exercise, social activities, and healthy sleep habits)
References and Sources
Alsubheen, S. A., Nazari, G., Bobos, P., MacDermid, J. C., Overend, T. J., & Faber, K. (2019). Effectiveness of Nonsurgical Interventions for Managing Adhesive Capsulitis in Patients With Diabetes: A Systematic Review. Archives of physical medicine and rehabilitation, 100(2), 350–365. doi:10.1016/j.apmr.2018.08.181
Bailey, L. B., Thigpen, C. A., Hawkins, R. J., Beattie, P. F., & Shanley, E. (2017). Effectiveness of Manual Therapy and Stretching for Baseball Players With Shoulder Range of Motion Deficits. Sports health, 9(3), 230–237. doi:10.1177/1941738117702835
Beard, D. J., Rees, J. L., Cook, J. A., Rombach, I., Cooper, C., Merritt, N., … CSAW Study Group (2018). Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet (London, England), 391(10118), 329–338. doi:10.1016/S0140-6736(17)32457-1
Cools, A. M., Maenhout, A. G., Vanderstukken, F., Declève, P., Johansson, F. R., & Borms, D. (2020). The challenge of the sporting shoulder: from injury prevention through sport-specific rehabilitation toward return to play. Annals of physical and rehabilitation medicine, S1877-0657(20)30082-8. Advance online publication. https://doi.org/10.1016/j.rehab.2020.03.009
Dueñas, L., Balasch-Bernat, M., Aguilar-Rodríguez, M., Struyf, F., Meeus, M., & Lluch, E. (2019). A Manual Therapy and Home Stretching Program in Patients With Primary Frozen Shoulder Contracture Syndrome: A Case Series. The Journal of orthopaedic and sports physical therapy, 49(3), 192–201. doi:10.2519/jospt.2019.8194
Fouda, M. B., Thankam, F. G., Dilisio, M. F., & Agrawal, D. K. (2017). Alterations in tendon microenvironment in response to mechanical load: potential molecular targets for treatment strategies. American journal of translational research, 9(10), 4341–4360.
Funk, L. (2018). Shoulder Rehabilitation: A Comprehensive Guide To Shoulder Exercise Therapy (4th ed). Shoulderdoc.co.uk.
Gismervik, S. Ø., Drogset, J. O., Granviken, F., Rø, M., & Leivseth, G. (2017). Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC musculoskeletal disorders, 18(1), 41. doi:10.1186/s12891-017-1400-0
Greening, J., Anantharaman, K., Young, R., & Dilley, A. (2018). Evidence for Increased Magnetic Resonance Imaging Signal Intensity and Morphological Changes in the Brachial Plexus and Median Nerves of Patients With Chronic Arm and Neck Pain Following Whiplash Injury. The Journal of orthopaedic and sports physical therapy, 48(7), 523–532. doi:10.2519/jospt.2018.7875
Hawk, C., Minkalis, A. L., Khorsan, R., Daniels, C. J., Homack, D., Gliedt, J. A., … Bhalerao, S. (2017). Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions. Journal of manipulative and physiological therapeutics, 40(5), 293–319. doi:10.1016/j.jmpt.2017.04.001
Hegedus, E. J., Goode, A. P., Cook, C. E., Michener, L., Myer, C. A., Myer, D. M., & Wright, A. A. (2012). Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. British journal of sports medicine, 46(14), 964–978. doi:10.1136/bjsports-2012-091066
Hegedus, E. J., Michener, L. A., & Seitz, A. L. (2020). Three Key Findings When Diagnosing Shoulder Multidirectional Instability: Patient Report of Instability, Hypermobility, and Specific Shoulder Tests. The Journal of orthopaedic and sports physical therapy, 50(2), 52–54. doi:10.2519/jospt.2020.0602
Karjalainen, T. V., Jain, N. B., Heikkinen, J., Johnston, R. V., Page, C. M., & Buchbinder, R. (2019). Surgery for rotator cuff tears. The Cochrane database of systematic reviews, 12, CD013502.doi:10.1002/14651858.CD013502
Lähdeoja, T., Karjalainen, T., Jokihaara, J., Salamh, P., Kavaja, L., Agarwal, A., Winters, M., Buchbinder, R., Guyatt, G., Vandvik, P. O., & Ardern, C. L. (2020). Subacromial decompression surgery for adults with shoulder pain: a systematic review with meta-analysis. British journal of sports medicine, 54(11), 665–673. https://doi.org/10.1136/bjsports-2018-100486
Le, H. V., Lee, S. J., Nazarian, A., & Rodriguez, E. K. (2017). Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder & elbow, 9(2), 75–84. doi:10.1177/1758573216676786
Lewis, J. (2016). Rotator cuff related shoulder pain: Assessment, management and uncertainties. Manual therapy, 23, 57–68. doi:10.1016/j.math.2016.03.009
Meehan, K., Wassinger, C., Roy, J. S., & Sole, G. (2020). Seven Key Themes in Physical Therapy Advice for Patients Living With Subacromial Shoulder Pain: A Scoping Review. The Journal of orthopaedic and sports physical therapy, 50(6), 285–a12. https://doi.org/10.2519/jospt.2020.9152
Park, S. W., Chen, Y. T., Thompson, L., Kjoenoe, A., Juul-Kristensen, B., Cavalheri, V., & McKenna, L. (2020). No relationship between the acromiohumeral distance and pain in adults with subacromial pain syndrome: a systematic review and meta-analysis. Scientific reports, 10(1), 20611. https://doi.org/10.1038/s41598-020-76704-z
Paavola, M., Kanto, K., Ranstam, J., Malmivaara, A., Inkinen, J., Kalske, J., Savolainen, V., Sinisaari, I., Taimela, S., Järvinen, T. L., & Finnish Shoulder Impingement Arthroscopy Controlled Trial (FIMPACT) Investigators (2020). Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: a 5-year follow-up of a randomised, placebo surgery controlled clinical trial. British journal of sports medicine, bjsports-2020-102216. Advance online publication. https://doi.org/10.1136/bjsports-2020-102216
Pieters, L., Lewis, J., Kuppens, K., Jochems, J., Bruijstens, T., Joossens, L., & Struyf, F. (2020). An Update of Systematic Reviews Examining the Effectiveness of Conservative Physical Therapy Interventions for Subacromial Shoulder Pain. The Journal of orthopaedic and sports physical therapy, 50(3), 131–141. https://doi.org/10.2519/jospt.2020.8498
Pietrzak, M. (2016). Adhesive capsulitis: An age related symptom of metabolic syndrome and chronic low-grade inflammation?. Medical hypotheses, 88, 12–17. doi:10.1016/j.mehy.2016.01.002
Richardson, E., Lewis, J. S., Gibson, J., Morgan, C., Halaki, M., Ginn, K., & Yeowell, G. (2020). Role of the kinetic chain in shoulder rehabilitation: does incorporating the trunk and lower limb into shoulder exercise regimes influence shoulder muscle recruitment patterns? Systematic review of electromyography studies. BMJ open sport & exercise medicine, 6(1), e000683. https://doi.org/10.1136/bmjsem-2019-000683
Salamh, P., & Lewis, J. (2020). It Is Time to Put Special Tests for Rotator Cuff-Related Shoulder Pain out to Pasture. The Journal of orthopaedic and sports physical therapy, 50(5), 222–225. https://doi.org/10.2519/jospt.2020.0606
Strauss, E. J., Kingery, M. T., Klein, D., & Manjunath, A. K. (2020). The Evaluation and Management of Suprascapular Neuropathy. The Journal of the American Academy of Orthopaedic Surgeons, 28(15), 617–627. https://doi.org/10.5435/JAAOS-D-19-00526
Steuri, R., Sattelmayer, M., Elsig, S., Kolly, C., Tal, A., Taeymans, J., & Hilfiker, R. (2017). Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. British journal of sports medicine, 51(18), 1340–1347. doi:10.1136/bjsports-2016-096515
Struyf, F., Tate, A., Kuppens, K., Feijen, S., & Michener, L. A. (2017). Musculoskeletal dysfunctions associated with swimmers’ shoulder. British journal of sports medicine, 51(10), 775–780. doi:10.1136/bjsports-2016-096847
Weber, S., & Chahal, J. (2020). Management of Rotator Cuff Injuries. The Journal of the American Academy of Orthopaedic Surgeons, 28(5), e193–e201. https://doi.org/10.5435/JAAOS-D-19-00463
Weiss, L. J., Wang, D., Hendel, M., Buzzerio, P., & Rodeo, S. A. (2018). Management of Rotator Cuff Injuries in the Elite Athlete. Current reviews in musculoskeletal medicine, 11(1), 102–112. doi:10.1007/s12178-018-9464-5
Wong, C. K., Levine, W. N., Deo, K., Kesting, R. S., Mercer, E. A., Schram, G. A., & Strang, B. L. (2017). Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy, 103(1), 40–47. doi:10.1016/j.physio.2016.05.009
Wong, W. K., Li, M. Y., Yung, P. S., & Leong, H. T. (2020). The effect of psychological factors on pain, function and quality of life in patients with rotator cuff tendinopathy: A systematic review. Musculoskeletal science & practice, 47, 102173. https://doi.org/10.1016/j.msksp.2020.102173
Wylie, J. D., Suter, T., Potter, M. Q., Granger, E. K., & Tashjian, R. Z. (2016). Mental Health Has a Stronger Association with Patient-Reported Shoulder Pain and Function Than Tear Size in Patients with Full-Thickness Rotator Cuff Tears. The Journal of bone and joint surgery. American volume, 98(4), 251–256. doi:10.2106/JBJS.O.00444


