1.5: Histology of Gglands, Lymphatics and Sinuses
- Page ID
- 41541
- Basic anatomy
- Salivary glands
- Components of saliva
- Dental pellicle
- Histology of salivary glands
- Anatomy of salivary glands
- Clinical applications of gland histology
- Lymphatic system
- Lymph nodes
- Tonsils
- Clinical application of lymphatic histology
- Sinuses
- Para-nasal sinus anatomy
- Clinical application of para-nasal sinus histology

Basic anatomy of exocrine glands and lymphatic organs
The average exocrine gland is composed of simple cuboidal epithelial cells that form grape-shaped structures called acini (although other glands have tube-shaped ends). These grape-shaped structures are where secretions are produced. The liquids produced by these cells enter a duct, which can be made of simple cuboidal or simple columnar epithelial cells. It is possible for larger glands to have regions of stratified cuboidal epithelial cells. The outside of the gland is surrounded by a dense connective tissue capsule (not quite thick enough for us to worry about whether the collagen fibers are regular or irregular). The connective tissue extends inwards forming trabeculae (or septa, not to be confused with the trabeculae of spongy bone tissue), which divide the organ into lobes.
The average lymphatic organ shares patterns with exocrine glands. A lymphatic organ is surrounded by a dense connective tissue capsule, and that connective tissue extends inwards forming trabeculae. Inside a lymphatic organ, clusters of white blood cells suspended within reticular connective tissue form germinal centers (or nodules) where white blood cells filter cellular debris and scan body fluids for pathogens. If they detect a pathogen, they multiply, release inflammatory signals, and migrate through the body’s connective tissues looking for more pathogens.
Salivary glands

Components of saliva
The major function of salivary glands is to produce saliva, which helps maintain the health of the oral mucosa and teeth, as well as assist in mastication. Acinar epithelial cells transcribe and translate long mucous proteins on the rough endoplasmic reticulum, modify them in the Golgi apparatus to form large glycoproteins, and secrete them. These cells also pump electrolytes from their cytoplasm into the lumen of the acinus, which, along with the glycoproteins, attract water by osmosis. These components make saliva moist and sticky enough to adhere to all surfaces of the oral cavity, rather than sink to the floor of the mouth.
Other molecules are secreted to become a part of saliva. Buffers within saliva help to maintain a stable pH, despite the acidity or alkalinity of different foods, or the acidity of certain oral bacterial secretions. Buffers and electrolytes also help disrupt the formation of bacterial biofilms, which bacteria use to adhere to teeth. The watery nature of saliva helps to moisten food and the oral mucosa, assisting in mastication, speech and swallowing. Watery saliva helps to limit the population of oral bacteria. People swallow saliva even when they are not eating, flushing a percentage of oral microorganisms down to the stomach, where certain death awaits in the form of Hydrochloric Acid and the protein-destroying enzyme pepsin. The enzymes salivary amylase and lysozyme are produced by acinar cells to serve a similar purpose, breaking covalent bonds within the cell walls of viruses and bacteria, or their surface glycoproteins used to adhere to tooth surfaces. Without hours of mechanical digestion by the teeth and stomach, there is very little surface area for salivary amylase to digest carbohydrate molecules for nutritional purposes. Chemical digestion of carbohydrates for nutrition is carried out in the small intestines by the much more abundant pancreatic amylase. Bacteria, however, do not form a bolus (a large solid mass), their cell walls and surface glycoproteins are open to attack by enzymes without prior mechanical processing. A second function of salivary amylase is to cleave a small amount of small sugars from starch, allowing taste buds to detect them, so Salivary amylase and other carbohydrases in saliva function in the sense of gustation as well as in limiting bacterial populations.
Dental pellicle
The dental pellicle is a coating of glycoproteins from saliva on the surface of teeth. It normally prevents excess deposits of Ca2+PO43-. It also prevents demineralization of enamel. Both depositing bumps or eroding crevices allows bacteria to adhere to teeth and avoid being washed into the stomach. Saliva also contains the minerals that produce calculus, so its role is complex.
Histology of salivary glands

Serous acini produce more watery secretions. These are composed of simple cuboidal epithelium. Serous acini tend to stain more faintly using a traditional H&E stain, because they make fewer proteins.
Mucous acini secrete more glycoproteins, making their secretion thicker and stickier (more mucous). Mucous acini are made of a simple columnar epithelium. Mucous acini tend to stain a little darker using a traditional H&E stain, because they make more proteins.
Muco-serousacini produce secretions halfway in-between the first two in consistency. These look like mucous acini under the microscope, with an additional bonnet (a hat) of myo-epithelial cells. These cells contract like smooth muscle cells. For most epithelial cells, the actin and myosin genes are not highly expressed, except by epithelial stem cells, which may need to migrate to a different area to help repair a wound. Myo-epithelial cells, on the other hand, use some of the DNA instructions for making larger amounts of actin and myosin and organizing them into filaments more similar to muscle tissue than generic cytoskeleton. This makes these myo-epithelial cells appear more similar to smooth muscle than an epithelium. However, these cells have an epithelial lineage– they differentiated from an epithelial stem cell, not from a Mesenchymal Stem Cell or myoblast.
All three secretions mix in the oral cavity to produce saliva. These secretions reach the oral cavity by way of different ducts, which can be identified under the microscope by their different types of epithelial cells. We know of no clinical significance to the types of ducts or their cells.

Anatomy of exocrine glands
There are three major and numerous minor salivary glands. The three major salivary glands are listed in Table 5.1.
| Major salivary gland | Details |
|---|---|
| Parotid salivary glands | Largest |
| Serous (mostly) | |
| 25% saliva by volume | |
| Sub-mandibular salivary glands | 2nd largest |
| Muco-serous | |
| 65% saliva by volume | |
| Sub-lingual salivary gland | Mucous |
| 10% saliva by volume |
Table 5.1: Summary of the three major salivary glands.

The parotid glands drain into the oral cavity by way of the parotid duct (or Stensen duct). The ducts travel through the masseter muscle and enters the oral cavity at a papilla usually located lateral to the 2nd maxillary molar.

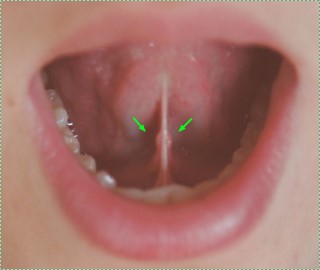
The sub-lingual glands and sub-mandibular glands have ducts that share an entrance on the floor of the mouth at the sub-lingual caruncle. The sub-lingual gland also has numerous smaller ducts that open onto the floor of the mouth.

Numerous minor salivary glands are located throughout the oral cavity. They are normally not visible, unless the oral mucosa is hyper-keratinized. Luckily, no one has bothered to name these glands or their ducts, except for the von Ebner salivary glands, which are minor salivary glands associated with the circumvallate lingual papillae. The minor salivary glands are predominantly mucous, with exceptions, which helps their secretions to stick to the roof and sides of the oral cavity.
Clinical application of salivary gland histology
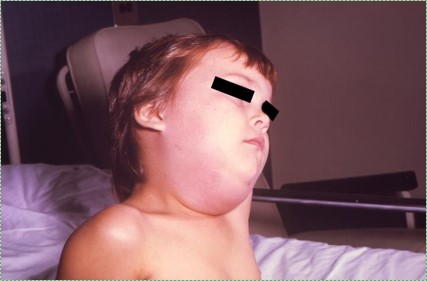
Mumps is a viral infection that causes swelling of the Parotid glands. Vaccination has reduced the number of mumps cases in the US by over 99%. Unfortunately, mumps outbreaks still occur, often in high-density living areas (such as college dormitories), aided by fraud, misinformation campaigns, and conspiracy theories targeting vaccines (the MMR vaccine in particular, at least in the U.S.). Unfortunately, it is difficult to counter these or other beliefs in pseudoscience, although some strategies work better than others.

Hypo-salivation
Hypo-salivation, or decreased saliva production, can be caused by certain diseases, medications, cancer treatments, and aging. It may result in xerostomia, or dry mouth. Reduced saliva can decrease the healing ability of the oral mucosa, leading to sores. Reduced saliva also reduces limits to growth placed on the oral microbiome, leading to infections and caries. Reduced taste can also be a consequence, which patients might compensate for by flavoring their food with excessive levels of salt (NaCl). Using Monosodium Glutamate (MSG, or NaC5H8NO4) to enhance both flavor and saliva production is a significantly safer option, despite fears of the non-existent (not to mention racist) Chinese Restaurant Syndrome.

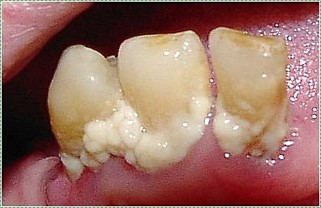
Mineralized saliva (sialoliths)
Electrolytes in saliva can precipitate and form salivary gland stones, or sialoliths. Large sialoliths may block the duct of one of the salivary glands, which stops the flow– but not the production– of saliva. As a result, saliva builds up in the gland, causing swelling and possibly inflammation. Blockage of a minor salivary gland produces a swelling within the oral mucosa known as a mucocoele (Fig. 5.14), while blockage of a major salivary gland produces a ranula (Fig. 5.115). These are fairly common disorders. Inflammation of the parotid gland must be clearly distinguished from mumps before any treatment is given.


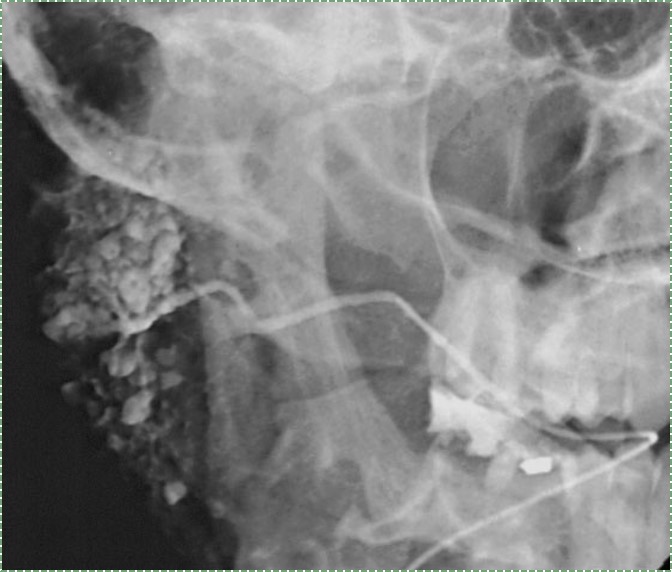
Sialography
Sialoliths may be felt by technicians. Alternately, an image of the blockage known as a sialograph can be taken by injecting a radiopaque dye as far into the salivary gland duct as it can go (until further flow is blocked by the sialolith). Usually, sialoliths are removed with minimal discomfort. Sialography should not be done in cases of acute infection, as the dye may push infectious exudate, spreading the infection.
Lymphatic system

Very basic overview of the lymphatic system
| Lymphatic organ | Major function |
|---|---|
| Lymphatic vessels | Drain ECF off organs, including teeth |
| Lymph nodes | Filter debris and identify pathogens |
| Tonsillar tissue | Identify pathogens |
| Other lymphatic organs | Located below the neck |
Table 5.2: Functions of the major lymphatic organs

Lymphatic drainage of the teeth
Fluid travels to the teeth via capillaries. As plasma exudes from the capillaries, it becomes ECF. Veins collect most of this fluid, the rest is collected by lymphatic vessels. ECF absorbed into a lymphatic vessel is called lymph, and it is returned to the circulatory system. Lymphatic vessels are more permeable than capillaries, having mini-valves on their outer edges. Mini-valves allow solids to enter the lymphatic vessels, including cellular debris, microorganisms, and cancer cells. The lymphatic vessels are connected to a number of lymph nodes, which clean up debris and mount an immune response against the microorganisms and cancer cells. Knowing the anatomical connections of the lymphatic vessels helps locate periodontal disease by the inflammation triggered in down-stream lymph nodes.
Lymph nodes
Lymph nodes are found throughout the body. A large cluster of lymph nodes can be found in the neck, called the cervical lymph nodes, in addition to other locations. Lymph nodes are composed primarily of reticular connective tissue, which provides support for resident clusters of white blood cells. Afferent lymphatic vessels bring lymph to the node, while efferent vessels drain lymph towards the circulatory system.
Lymph nodes serve two major functions. One is to clear cellular debris before lymph reaches the circulatory system, becoming blood plasma again. Two is to identify pathogens and begin an inflammatory response when necessary. If this occurs, white blood cells multiply within the node and secrete inflammatory molecules.

Tonsillar tissue
Tonsillar tissue is similar to lymph nodes, except there are no lymphatic vessels, and one end of the tonsil is un-encapsulated (an broad opening). Clusters of white blood cells can be found in germinal centers, suspended within reticular connective tissue.
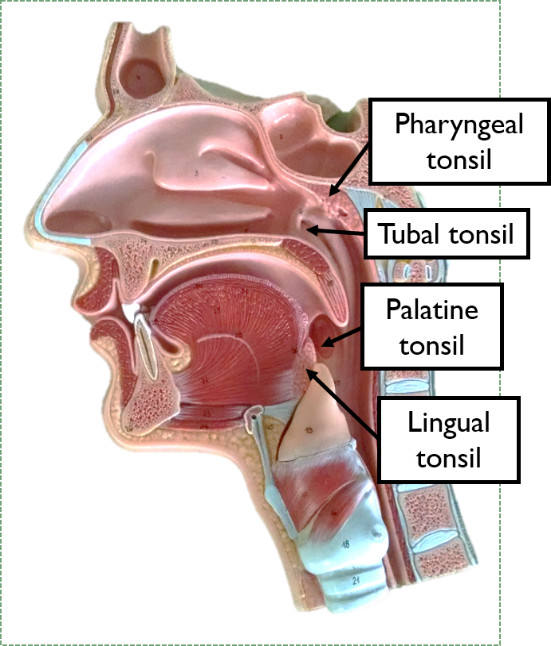
The tonsils
There are 4 major tonsils located the border of the oral cavity and pharynx: lingual, palatine, pharyngeal and tubal. These tonsils form a ring, called Waldeyer’s ring, which serves to identify pathogens that are either ingested or inhaled, and begin an immune response before they reach deeper locations, such as the lungs or stomach. Because of their anatomy (no vessels), tonsils do not filter debris or microorganisms out of bodily fluids, they only identify pathogens. The un-encapsulated side faces the lumen of the pharynx, coming into contact with many foreign molecules.

Clinical applications of lymphatic system histology

Lymphadenopathy of lymph nodes
In the absence of infection, lymph nodes are soft and moveable. However, if white blood cells detect a pathogen, they undergo cell division and release inflammatory molecules. This leads to lymph nodes becoming palpable, possibly visibly swollen, and likely sensitive to touch. The swelling of lymphatic tissue is called lymphadenopathy, and is a non-specific sign of immune system activation.

The mandibular incisors drain into sub-mental lymph nodes. The sub-mental lymph nodes and the rest of the teeth (other than maxillary 3rd molars) drain into sub-mandibular lymph nodes. The sub-mandibular lymph nodes then drain into superior deep cervical nodes. Swelling of some or all of these lymph nodes can indicate active periodontal disease.

Lymphadenopathy of tonsillar tissue
Tonsillar tissue can become inflamed, and when it does it is usually called tonsillitis. When it does, the increased number of white blood cells (living and dead) may be visible as white-ish patches within the inflamed tonsil(s). Tonsillitis is more common in children between pre-school and pre-teens because of the way the immune system develops immunocompetency and tolerance.
Para-nasal sinuses

Basic anatomy of the para-nasal sinuses
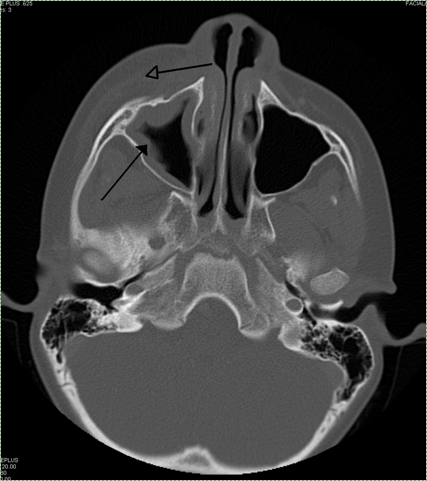
The para-nasal sinuses are spaces within the frontal, sphenoid, ethmoid and maxillary bones surrounding the nasal cavity. The maxillary, frontal and sphenoid sinus communicate with (connect to) the nasal cavity via small passageways. The para-nasal sinuses are lined with pseudostratified epithelium. This epithelium produces mucus which can trap pathogens and debris. With the aid of cilia, these harmful agents are removed from the body. Within the nasal cavity are 3 bumps called nasal conchae, which divide the nasal cavity into three winding spaces called the nasal meatuses. (for those who are counting, there is a fourth space above the superior nasal conchae called the spheno-ethmoid recess, it is not a meatus because it does not form a pathway from the nasal vestibule to the nasopharynx).
Clinical applications of para-nasal sinus histology
Inflammation within the para-nasal sinuses
When the para-nasal sinuses become inflamed (known as sinusitis), the small ducts leading to the nasal sinuses may become obstructed. The increase in fluid that accompanies inflammation l has nowhere to drain, leading to pressure within the sinuses. Furthermore, one response of goblet cells to inflammatory signals is to produce more mucous proteins, which again has nowhere to drain.
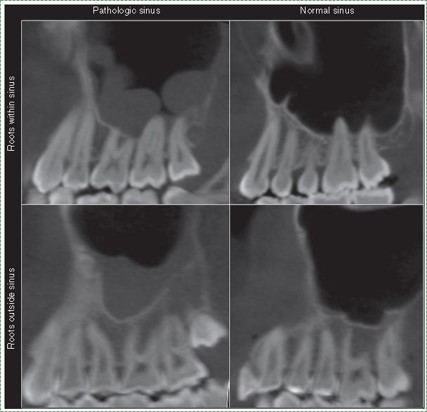
The posterior maxillary teeth lie close to, or partly within the maxillary sinuses. Therefore, if inflammation occurs within these sinuses, it can cause discomfort to the significantly more-sensitive teeth. Furthermore, sinus infections may spread to the posterior maxillary teeth.
Chapter 4 * Chapter 6


