1.40: Transoral Lateral Oropharyngectomy (Radical Tonsillectomy) for Cancer of the Tonsil
- Page ID
- 17677
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
TRANSORAL LATERAL OROPHARYNGECTOMY / RADICAL TONSILLECTOMY FOR CANCER OF THE TONSIL: ANATOMY, PRINCIPLES AND TECHNIQUES
Johan Fagan & Wayne Koch
In developed countries, early (T1/2) tonsil cancers are commonly resected by lateral oropharyngectomy (radical tonsillectomy) employing transoral CO2 laser microsurgery or transoral robotic surgery (TORS) techniques. Yet most surgeons in the world do not have access to CO2 laser or TORS. In such centers early tonsil cancers are often resected by simple tonsillectomy. However, dissecting along the tonsillar capsule and not including the pharyngeal constrictors as the deep margin often results in close or involved deep margins necessitating adjuvant (chemo)radiation.
Because cancers of the tonsil are in a direct line-of-sight for the surgeon when using a simple tonsillectomy gag, there is little reason why the surgical principles that apply to lateral oropharyngectomy by transoral CO2 laser or TORS techniques should not be employed to lateral oropharyngectomy performed with headlight/diathermy, or microscope/diathermy, or loupes/headlight/diathermy techniques to secure adequate resection margins.
Regardless of the surgical tools being used, lateral oropharyngectomy requires a detailed understanding of the “inside-out” 3D anatomy of the oropharynx, and of the parapharyngeal (PPS) and retropharyngeal spaces. Without such an understanding one is less likely to achieve adequate resection margins and more likely to encounter bleeding, nerve damage and injury to the internal carotid artery.
This chapter details the surgical anatomy of the oropharynx, PPS and retropharyngeal spaces, and discusses principles and techniques relating to transoral resection of tonsil cancers regardless of the surgical tools being used.
Surgical anatomy
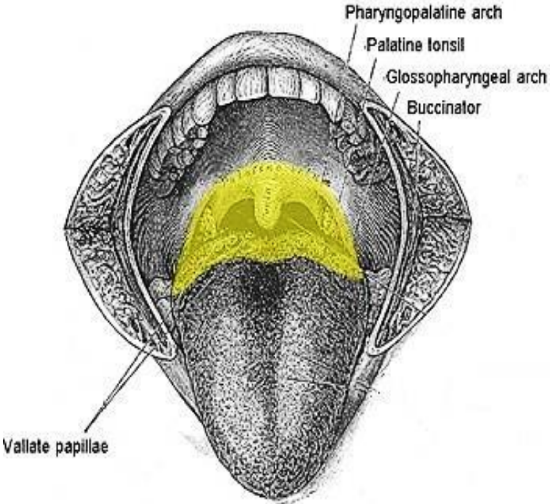
Figure 1: Oropharynx
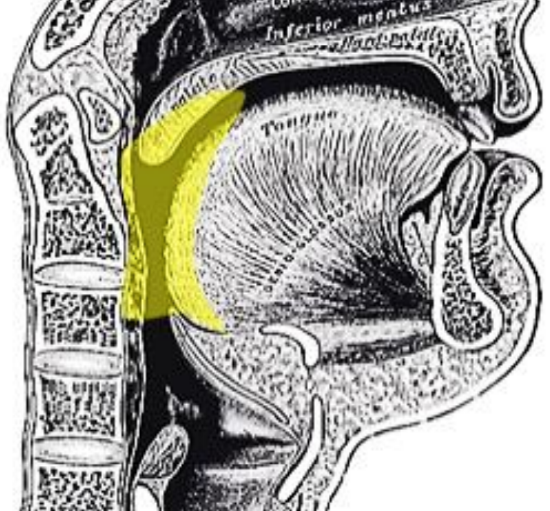
Figure 2: Oropharynx
The oropharynx encompasses the base of tongue, tonsils, soft palate, and lateral and posterior walls of the pharynx between the levels of the hard palate and hyoid bone (Figures 1a, b).
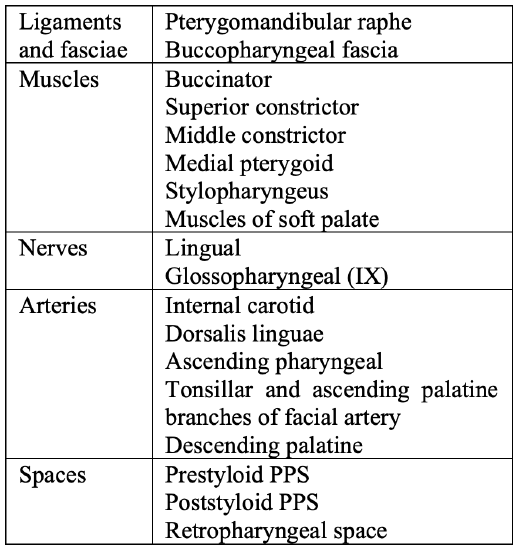
Table 1: Key anatomy for lateral oropharyngectomy
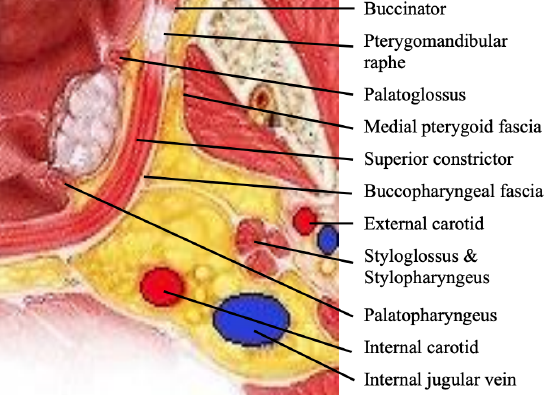
Figure 2: Key anatomical structures for lateral oropharyngectomy at level of tonsil; yellow tissue is parapharyngeal fat (Adapted from Ento Key)
Key anatomical structures relevant to lateral oropharyngectomy are listed in Table 1 and illustrated in Figure 2.
Base of tongue (BOT)
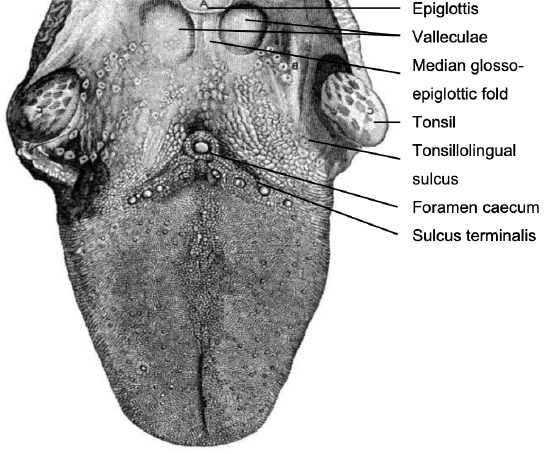
Figure 3: Topography of BOT
This comprises the posterior 1/3 of the tongue behind the foramen caecum and sulcus terminalis (Figure 3). The mucosa is rough, thick and fixed to the underlying muscle and contains lymphoid follicles (lingual tonsil); this makes it difficult to identify the edges of a BOT tumor; hence frozen section is especially useful to assess resection margins. Posterolaterally the tonsillolingual sulci separate the tongue from the tonsillar fossae. The valleculae separate the BOT from the lingual surface of the epiglottis and are separated in the midline by the median glossoepiglottic fold (Figure 3).
Soft palate
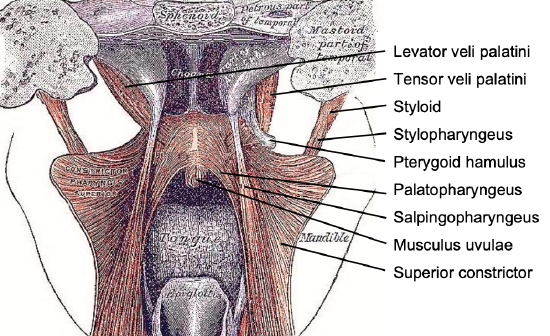
Figure 4: Posterior view of soft palate and pharynx with superior constrictor splayed open
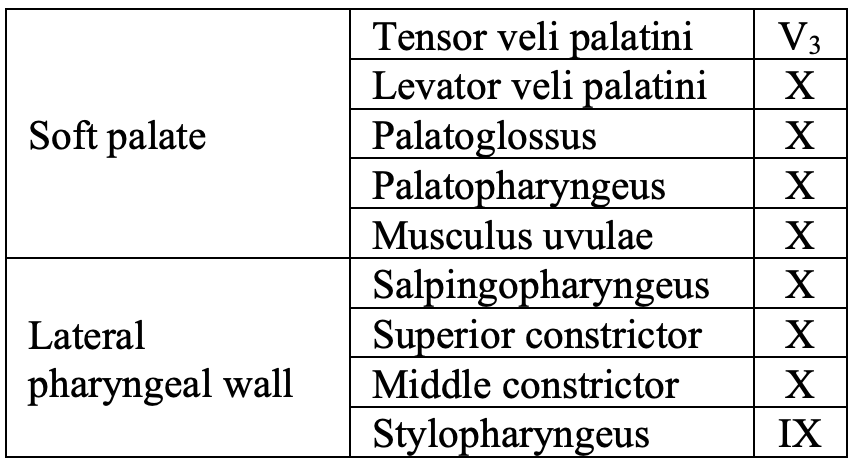
Table 2: Muscles of soft palate and oropharynx and cranial nerves which innervate them
The soft palate has a complex muscular structure and innervation. It has key functions relating to speech and swallowing. Resection and inadequate reconstruction of the palate results in loss of nasal separation which manifests clinically as nasal regurgitation of fluids and food, and hypernasal speech which can be quite disabling. The complex muscular anatomy of the soft palate and lateral pharyngeal wall is illustrated in Figure 4. Muscles that contribute to the soft palate and lateral pharyngeal wall are summarized in Table 2.
Lateral and posterior pharyngeal walls
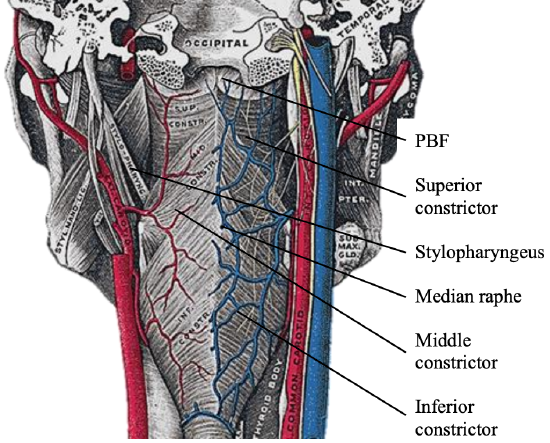
Figure 5: Posterior view of pharynx illustrates attachment of the superior constrictor to pharyngobasilar fascia (PBF) above and the median raphe to which pharyngeal constrictors attach; note close anatomical relationships of internal and external carotid artery systems to pharynx
Lateral oropharyngectomy involves dissecting along the outer aspect of the pharyngeal constrictors. The oropharynx has several layers i.e. mucosa, submucosa, muscle and buccopharyngeal fascia. The submucosa is represented by the pharyngobasilar fascia that lines the inner aspect of the constrictor muscles. It thins as it extends inferiorly from its attachment to the skull base and bridges the gaps between the skull base and the superior constrictor, the superior and middle constrictors, and the middle and inferior constrictors (Figure 5). Posteriorly it forms a median raphe to which the pharyngeal constrictors attach (Figure 5).
The buccopharyngeal fascia invests the pharyngeal constrictor muscles and is continued forward from the superior constrictor over the buccinator (Figure 2). It is loosely attached to the prevertebral layer by connective tissue, with the retropharyngeal space between them.
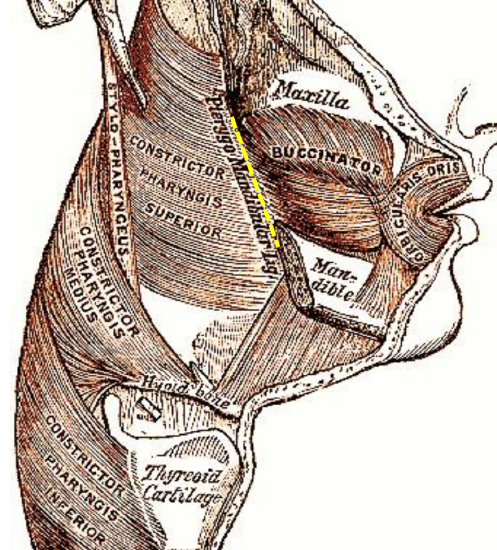
Figure 6: Note how buccinator and superior constrictor muscles attach to the pterygomandibular raphe (yellow line)

Figure 7: Pterygomandibular fold represents the surface marking of pterygomandibular raphe
The pterygomandibular raphé/ligament is a tendinous band of buccopharyngeal fascia and is a key structure to identify initially in lateral oropharyngectomy to gain access to the correct lateral dissection plane. It is attached at one end to the hamulus of the medial pterygoid plate, and at the other end to the posterior end of the mylohyoid line of the mandible (Figures 6, 7).
It is interposed between the buccinator muscle which is attached to its anterior edge, and the superior constrictor muscle which is attached to its posterior edge (Figures 2, 6). Medially it is covered only by buccal mucosa. Laterally it is separated from the ramus of the mandible and medial pterygoid muscle and fascia by adipose tissue (Figure 2). The pterygomandibular fold represents the surface marking of the pterygomandibular raphe (Figure 7).
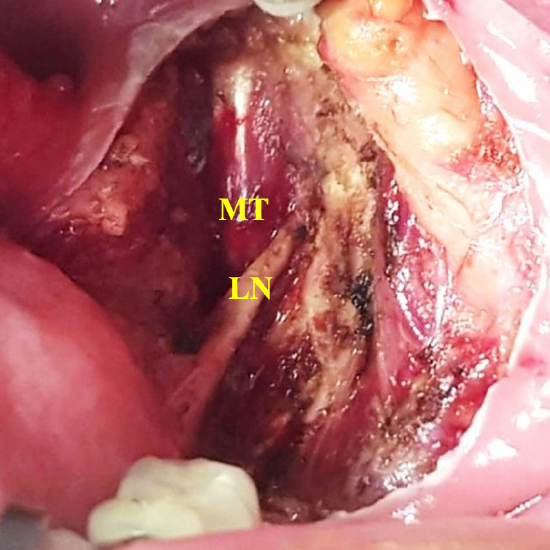
Figure 8: The lingual nerve (LN) courses lateral to the medial pterygoid muscle (MT)
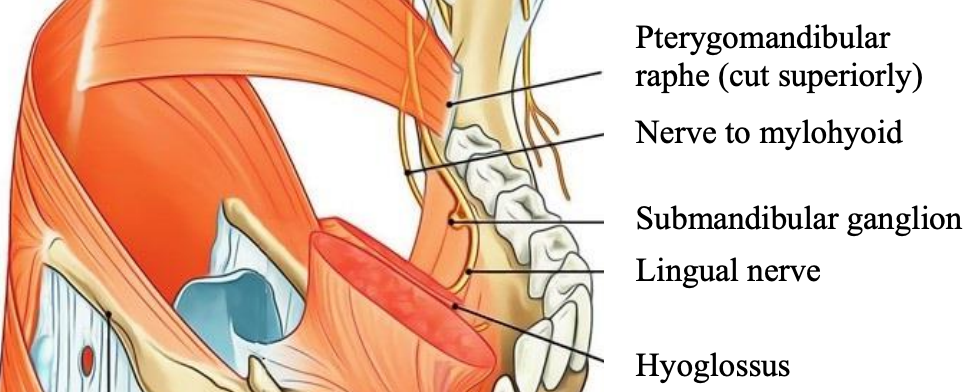
Figure 9: Lingual nerve emerging between lower attachment of raphe to the mandible and the mylohyoid muscle (adapted from Earthslab.com)
The lingual nerve emerges anteriorly between the medial pterygoid and the vertical ramus of the mandible (Figure 8). It is therefore protected by the medial pterygoid muscle during lateral oropharyngectomy. However, it is vulnerable to injury when dissecting inferiorly where it courses above the mylohyoid muscle (Figure 9).
The buccinator muscle is transected during lateral oropharyngectomy just anterior to the pterygomandibular raphe. It is a thin, quadrilateral muscle in the cheek, and originates from the outer surfaces of the alveolar processes of the maxilla and mandible. Posteriorly it attaches along the length of the pterygomandibular raphe (Figures 2, 6).
Medially, it is covered by submucosa and mucosa of the cheek. Laterally it is related to the ramus of the mandible, the masseter and medial pterygoid muscles, the buccal fat pad and the buccopharyngeal fascia.
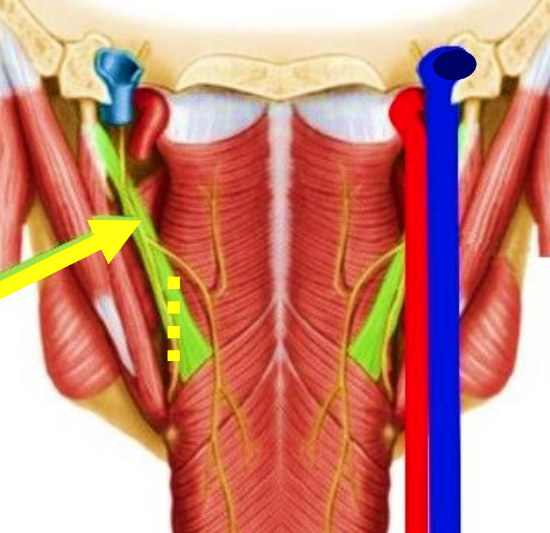
Figure 10: Relationships of stylopharyngeus muscle (green) and internal carotid artery and internal jugular vein. Yellow arrow points to IX nerve. Yellow broken line indicates division of stylopharyngeus muscle during lateral oropharyngectomy (adapted from Netter’s Anatomy)
The superior and middle constrictor muscles form the lateral and posterior walls of the oropharynx (Figures 4, 5, 6, 9, 10), with lesser contributions from the salpingopharyngeus (Figure 4), stylopharyngeus (Figures 4, 5, 6, 10) and palatopharyngeus (Figure 4) muscles.
The stylopharyngeus arises from the medial side of the base of the styloid process, passes downward through the fat of the PPS along the side of the pharynx, then between the superior and middle constrictors, and fans out beneath the mucosa (Figures 2, 5, 6, 10). The glossopharyngeal (IX) nerve innervates the stylopharyngeus. It runs on the lateral side of the muscle and crosses over it to reach the base of the tongue (Figure 10).
The deep dissection plane during lateral oropharyngectomy is between the buccopharyngeal fascia/fat of the prestyloid, retrostyloid and retropharyngeal spaces, and the constrictors. Because the stylopharyngeus crosses the PPS to join the pharynx, it must be transected to enable the surgeon to follow the plane along the constrictors towards the retropharynx (Figures 2, 10).
The muscles of the soft palate are not individually dissected and identified but are simply transected with the primary tumor.
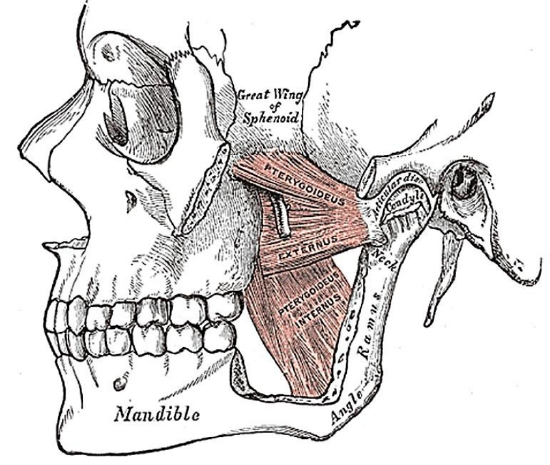
Figure 11: Medial and lateral pterygoids
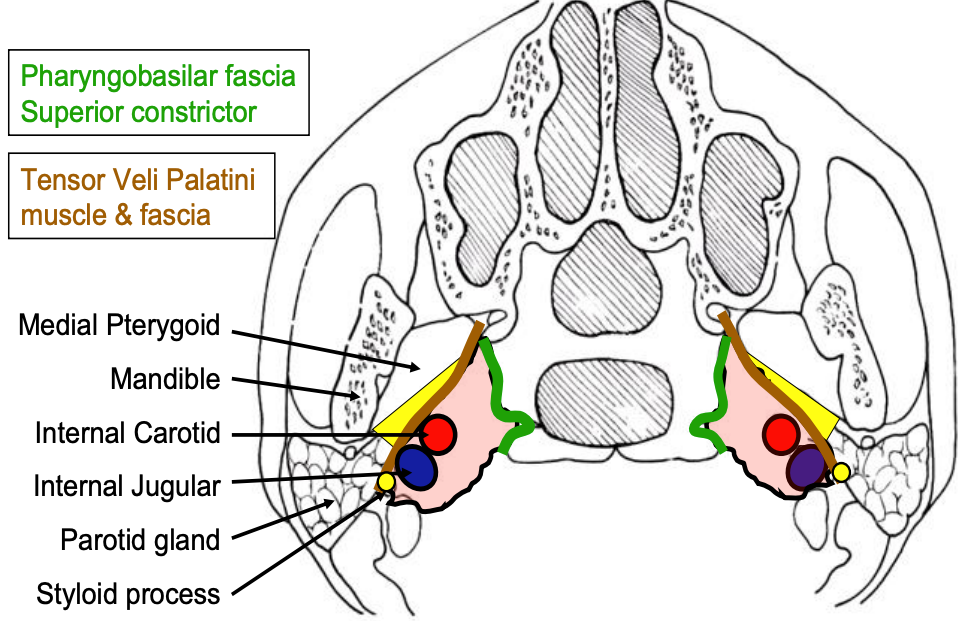
Figure 12: Axial view of prestyloid (yellow) and poststyloid (pink) PPS
The medial pterygoid (Figures 2, 8, 11, 12) constitutes the anterolateral border of the prestyloid PPS and is exposed early in the dissection. It has two heads: the larger deep head arises from just above the medial surface of the lateral pterygoid plate; the smaller superficial head arises from the maxillary tuberosity and the pyramidal process of the palatine bone (Figure 11). The muscle passes inferolaterally to insert onto the inferomedial surface of the ramus and angle of the mandible.
Parapharyngeal space (PPS)
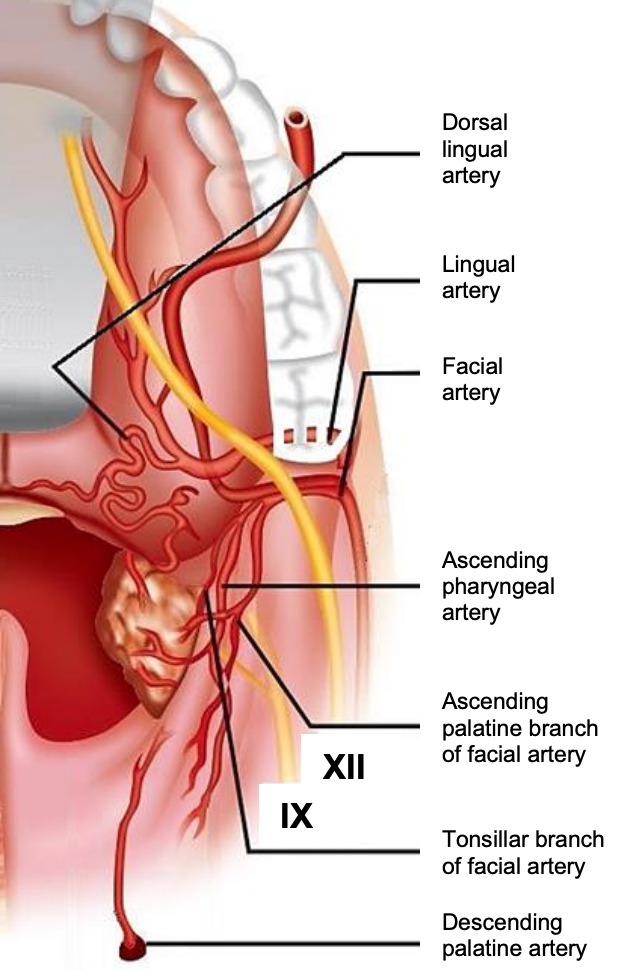
Figure 13: Arterial supply of tonsil and lateral oropharyngeal wall
The pharyngeal constrictor muscles form the medial border of the PPS, and the dissection therefore proceeds alongside, or within the fat of the PPS (Figures 12, 13). Therefore, the surgeon must be familiar with the anatomy of the PPS to anticipate the location of blood vessels, the stylopharyngeus muscle and the ICA.
The PPS extends as an inverted pyramid from the base of the skull superiorly, to the hyoid bone inferiorly. Figures 2 and 12 illustrate axial views of the prestyloid and poststyloid components of the PPS, separated by the styloid process, tensor veli palatini muscle and its fascia (brown). The prestyloid PPS is bordered anterolaterally by the medial pterygoid muscle, and posterolaterally by the deep lobe of the parotid gland (Figures 2, 12) and contains mainly fat. It is traversed by the arteries and veins supplying the pharynx and tonsil. The poststyloid PPS is confined medially by the pharyngobasilar fascia above, and the superior and middle constrictor muscles of the pharynx and contains the internal carotid artery and the internal jugular vein, as well as lower cranial nerves IX -XII, and the sympathetic trunk.
Arteries and veins (Figures 13, 14)
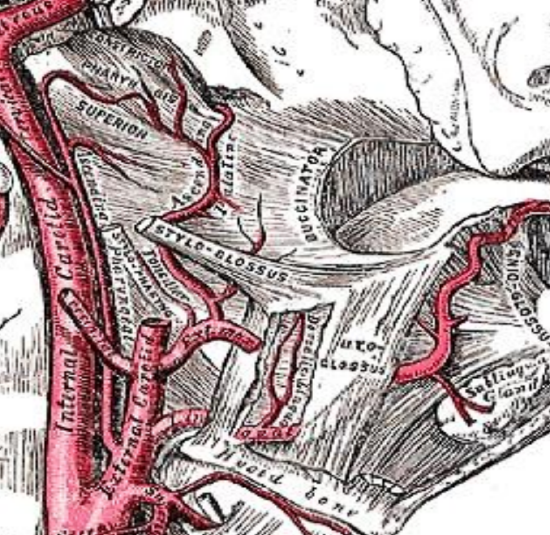
Figure 14: The ascending pharyngeal and ascending palatine and tonsillar branches of the facial (external maxillary) artery lie on the pharyngeal constrictor in the PPS
Knowledge of the vascular anatomy enables the surgeon to anticipate where arteries will be encountered and to minimize blood loss. Depending on the surgical procedure, vessels that may be encountered include the tonsillar and ascending palatine branches of the facial artery that arise in Level 1 of the neck, and the ascending pharyngeal artery, a branch of the external carotid artery (Figure 13). If the dissection includes BOT, the dorsalis linguae branches of the lingual artery may be encountered (Figures 13, 14). If the dissection is extended superiorly, the descending palatine artery may be encountered at the junction of the soft and hard palates (Figure 13).
Venous drainage is via the pharyngeal venous plexus to the internal jugular vein (Figure 5). The internal jugular vein is located posterolateral to the carotid and is hence not a concern (Figures 2, 5, 10).
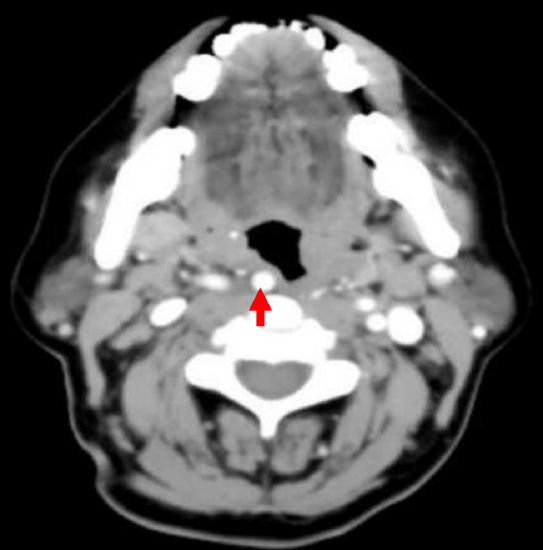
Figure 15: Retropharyngeal internal carotid artery
The internal carotid artery is generally not exposed, although pulsations of the vessel through the surrounding fat should be looked out for. Dividing the stylopharyngeus muscle gives direct access to the poststyloid PPS and artery (Figures 2, 5, 10, 14). The artery is normally located about 20-30 mm posterolateral to the outer aspect of the constrictors but may be ectatic (Figure 15) in up to 40% of the cases. A retropharyngeal ICA must be recognized preoperatively and protected and may be a relative contraindication to transoral resection.
Glossopharyngeal nerve (IXn)
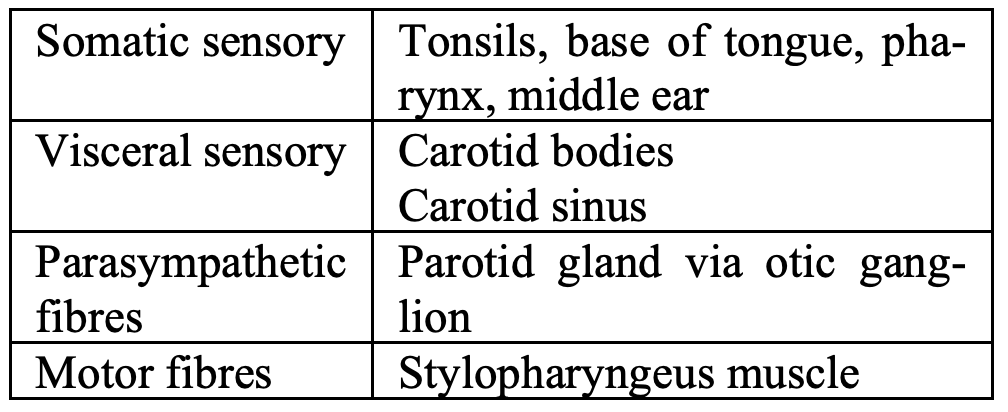
Table 3: IXn functions
Figures 10 and 13 show the course of the XIn in the PPS. The main trunk of the nerve curves anteromedially around the lateral border of stylopharyngeus and courses between the superior and medial pharyngeal constrictors. Of the functions of the IXn listed in Table 3, injury to the nerve during lateral oropharyngectomy would only affect taste and sensation to the base of tongue.
Lateral Oropharyngectomy
Lateral oropharyngectomy for cancer of the tonsil and lateral pharyngeal wall may be performed with a headlight and monopolar electrocautery, operating microscope and electrocautery, transoral CO2 laser microsurgery or TORS. The latter two techniques provide superior visual detail of tissue planes, tumor margins, vasculature and nerves. The description of the surgical steps that follow apply equally to all these techniques.
Indications
- Tumors of the lateral pharyngeal wall and tonsil that can be resected transorally with clear margins
- The ideal tumor is a T1/2 tonsil cancer in which the constrictor muscles have not been invaded
Contraindications1
General
- Poor transoral surgical access
- Coagulopathy
- Cervical spine pathology
- Poor fitness for surgery
Oncologic
- Cancer invading beyond pharyngeal constrictors to involve tissues and structures in PPS, medial pterygoid muscle, mandible or maxilla (requires combined transoral and transcervical approaches)
- Clinical evidence of perineural extension along major nerves e.g. lingual / V3
- Posterolateral fixation of cancer to prevertebral fascia
- Substantial extension into tongue base beyond unaided transoral exposed view
Vascular
- Retropharyngeal carotid artery
- Cancer adjacent to ICA or carotid bulb which will result in exposure of vessel
- Tumor encasement of carotid artery
Functional
- Resection of >50% deep tongue base
- Resection of >50% of posterior pharyngeal wall
- Resection of up to 50% of tongue base as well as entire epiglottis
- Resection of soft palate causing debilitating velopharyngeal insufficiency
Clinical evaluation
- Location and extent of primary tumor determined by visual inspection, palpation (and ultrasound2 evaluation)
- Mobility of tumor with swallowing and on palpation: if mobile it suggests that the PPS is not involved
- Fixation to prevertebral fascia: assessed by gently rocking soft tissue of tonsil fossa medially and laterally using bimanual palpation with one finger intraorally and opposite hand extraorally
- Function of lingual, inferior alveolar, mental, and hypoglossal nerves
- Position of ICA (inspection and palpation)
- Cervical and distant metastasis
- Synchronous primaries
- Access
- Mouth opening
- Trismus (possible medial pterygoid and infratemporal involvement)
- Dentition
- Cervical spine extension
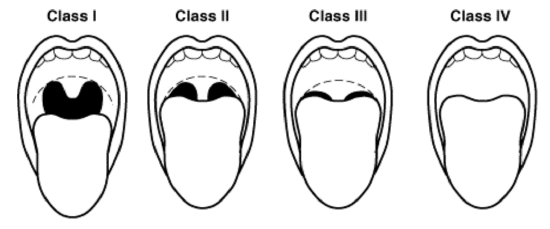
Figure 16: Mallampati scoring system
- Mallampati score (Figure 16)
Radiological evaluation
- Primary tumor
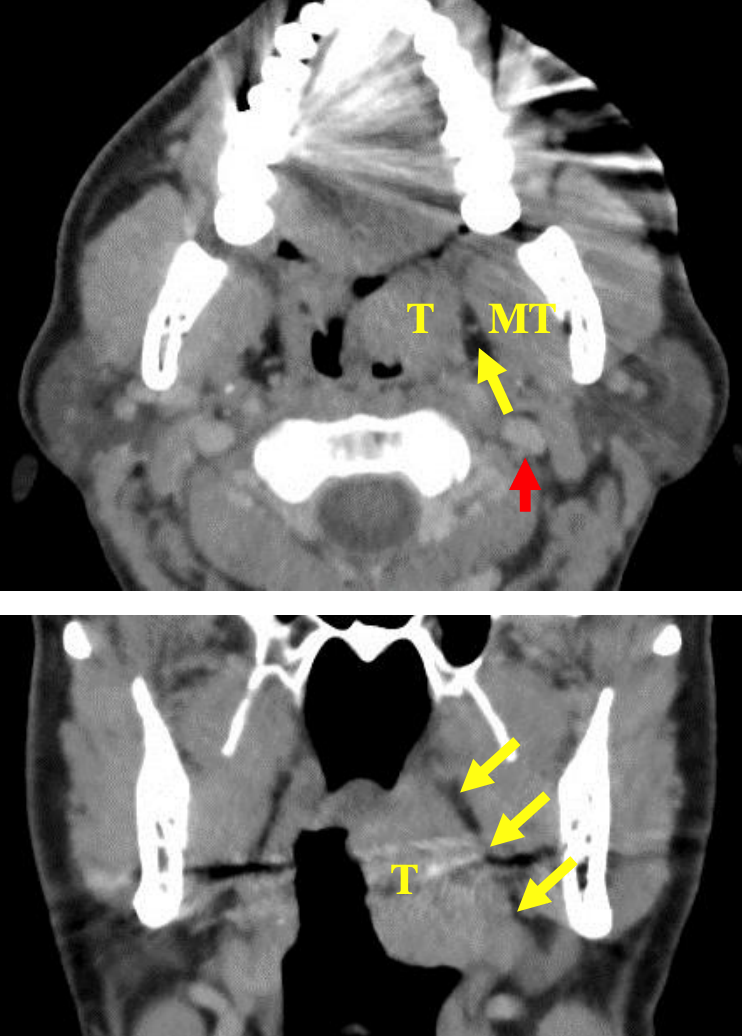
Figure 17ab: Axial and coronal CTs illustrate PPS fat (yellow arrows) separating tumor (T) from medial pterygoid muscle (MT), and the position of internal carotid artery (red arrow)
- CT / MRI / US2 (Figures 17ab)
- Not always required
- Mainly for advanced tumors if concern about extension to PPS and adjacent structures
- To determine position of internal carotid artery with larger resections
- Neck
- Chest
Informed consent
- Trauma
- Dental
- Lips, soft tissue
- Traction injury of lingual and hypoglossal nerves due to prolonged tongue depression
- Failure to complete transoral resection
- Possible conversion to combined transcervical approach
- Flaps o Oropharynx defect
- Cervical communication
- Neck dissection
- Tracheostomy
- Postoperative
- Feeding
- Analgesia
- Primary or secondary haemorrhage
- Healing time
- Anticipated functional outcomes
Anesthesia
- General anesthesia
- Orotracheal or nasotracheal intubation
- Nasogastric feeding tube contralateral to tumor (not always)
- Perioperative antibiotics if combined neck dissection
Surgical instrumentation (minimum)
The minimum instruments required for transoral lateral oropharyngectomy using a headlight +/- loupes include the following:
- Tonsillectomy instrument set

Figure 18: Dingman retractor
- Tonsil / Dingman retractor (Figure 18)
- Lindholm or other broad laryngoscope for reaching inferior extension, lateral wall or tongue base

Figure 19: Long-tipped insulated blade extension for monopolar cautery
- Standard or extended length monopolar electrocautery with insulated blade (for blunt dissection in PPS) (Figure 19)
- Bipolar long-tipped insulated electrocautery
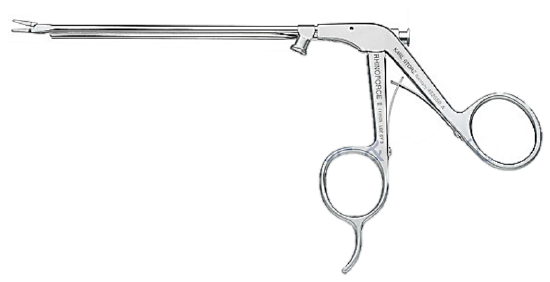
Figure 20: Liga clip applicator
- Liga clip applicator and clips, as used for transoral laryngeal microsurgery (Figure 20)
Surgical steps
- Perform panendoscopy to exclude synchronous tumors
- Inspect and palpate the tumor to determine mobility and extent
- Palpate tumor to ascertain extension to tongue base, fullness to superolateral aspect of pterygomandibular fold, soft palate, mobility with respect to pterygomandibular ligament
- Insert Dingman or tonsil retractor and place in suspension
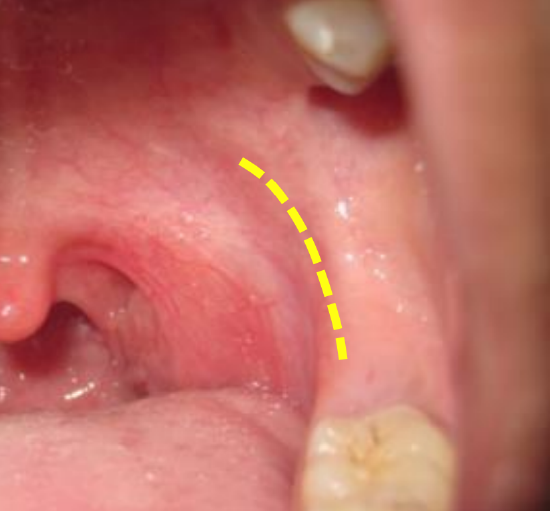
Figure 21: Pterygomandibular fold represents the surf
- Identify the pterygomandibular fold; it can be located by palpation (Figure 21)
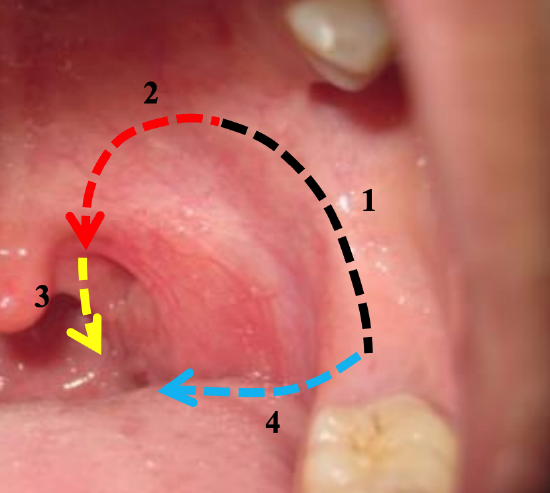
Figure 22: Typical sequence of incisions
- Incise the oral mucosa over the pterygomandibular fold to expose the pterygomandibular raphe; it is a key anatomical landmark to establish the correct lateral dissection plane (Figure 22)
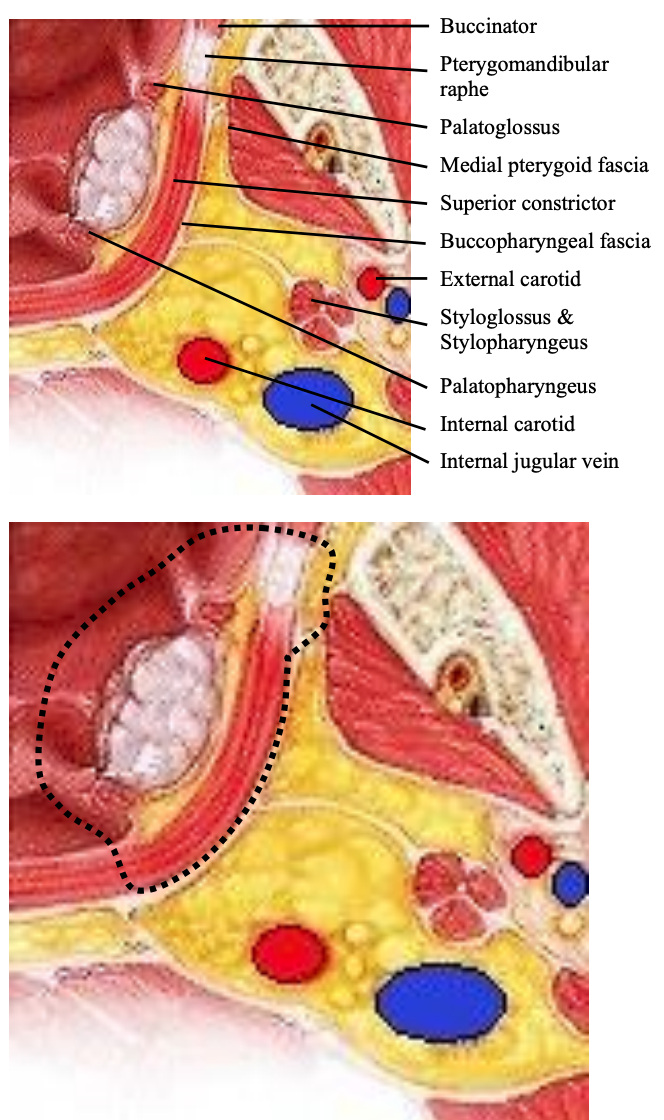
Figure 23: Key anatomical structures for lateral oropharyngectomy and typical dissection lines and planes for lateral oropharyngectomy (Adapted from Ento Key)
- Transect the buccinator muscle along its attachment to the pterygomandibular raphe (Figures 22, 23)
- Identify the fascia overlying medial pterygoid muscle (Figure 23)
- Dissect posteriorly along the medial pterygoid fascia while retracting the tumor and tonsil medially
- If possible, preserve the buccopharyngeal fascia to seal the oropharynx from structures in the PPS
- Free the superior pole of the specimen by incising through the pterygomandibular raphe, and soft palate mucosa and muscles (Figure 22)
- Free the tumor posteriorly by extending this incision inferiorly through the palatopharyngeus muscle (posterior tonsillar pillar) and pharyngeal mucosa and superior pharyngeal constrictor; this prevents the surgeon excising the posterolateral pharyngeal wall too far medially during the final steps of resection (Figures 20, 21)
- Free the tumor inferiorly by cutting below the tumor, including the tonsillolingual sulcus and lingual tonsil if required (Figures 22, 23)
- Continue the lateral dissection, taking care to remain medially in the dissecttion plane on the superior pharyngeal constrictor, palatoglossus, and palatopharyngeus muscles, using blunt dissection with the blade of the cautery
- Multiple branches of the facial, lingual and ascending pharyngeal arteries are seen to enter the specimen and are clipped, cauterized or tied and divided
- The facial or lingual arteries may have to be clipped or tied
- Identify the oblique-running styloglossus and vertically running stylopharyngeus muscles inferiorly in the surgical field
- The IX nerve may be seen coursing anterolaterally between these muscles (Figures 10, 13)
- The styloglossus and stylopharyngeus muscles obscure the internal carotid artery from the surgeon superiorly in the field (Figure 10). Transmitted pulsations, also from the external carotid artery, can be observed through the muscles, parapharyngeal fat and buccopharyngeal fascia
- Dissect bluntly when freeing the styloglossus and stylopharyngeus muscles inferiorly to avoid injury to the lingual artery
- Transect the styloglossus and stylopharyngeus muscles inferiorly as they course between the superior and middle pharyngeal constrictors
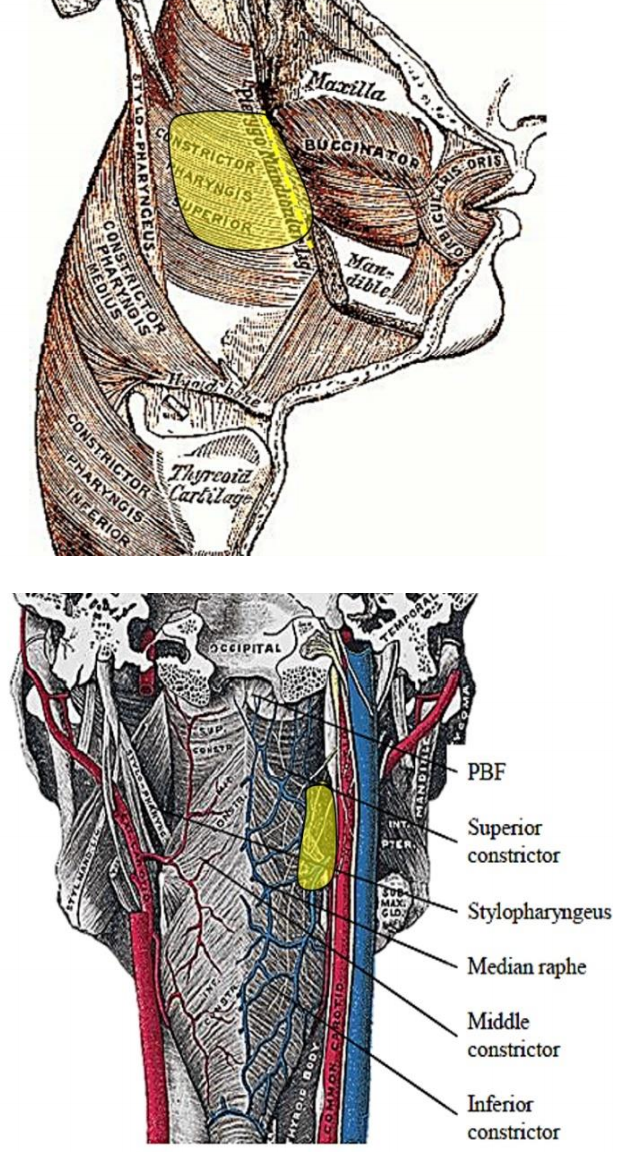
Figure 24ab: Typical resection (yellow)
- Release the specimen with final inferior cuts at the tonsillolingual sulcus and medial cuts through the superior pharyngeal constrictor (Figures 24 a,b)
- Carefully orientate and mark the specimen for the pathologist before removing it from the mouth
- If concern remains about inferior extension to lateral wall or tongue base, remove mouth retractor and examine with wide laryngoscope. Limited resection of residual disease may be undertaken with cup forceps and extended monopolar cautery using telescope for improved visualization and evacuating suction for smoke
- Obtain hemostasis
- If there has been a concurrent neck dissection, check for a direct communication with the neck
Postoperative care
- Analgesia
- Feeding: Commence when comfortable
- Airway
- Bleeding
- Antibiotics only if concomitant neck dissection
Complications
- Postoperative hemorrhage (1.5 - 13% of TORS)
- Up to a month postoperatively
- Potentially life-threatening
- Multiple large vessels are ligated and are left exposed to the pharynx to scar over by secondary intention
- With large resections one may elect to ligate the facial and lingual arteries or the ECA during the neck dissection to reduce the severity of postoperative bleeding
- Management depends on severity
- Minor: Observe in hospital
- Major
- Intubate/ tracheostomy
- Ligate/clip bleeders
- Ligate ECA
- Embolisation
- Airway obstruction
- Bleeding
- Oedema
- Flaps
- Secretions
- If in doubt, do a tracheostomy or keep intubated
- Dental trauma
- Lip or tongue lacerations
- Taste disturbance due to prolonged traction or surgical injury to the lingual nerve…recovers with time
- Hypoglossal nerve traction injury… recovers with time
Other issues
Can the specimen be removed piecemeal?
- It is a well-established, safe practice with transoral CO2 laser microsurgery to transect tumor to determine depth of invasion and to remove a tumor piecemeal, or to debulk the tumor to facilitate resection
- When a large oropharyngeal tumor prevents adequate exposure of the margins, it is therefore acceptable to transect the tumor and remove it piecemeal, taking care to accurately orientate the specimens for the pathologist
What constitutes a clear margin?
- It is not possible to achieve wide deep margins with cancers of the lateral pharyngeal wall without having to resect the contents of the PPS
- However, a 99% 5-year estimated local control was reported by Hinni (2013) following transoral resection of 128 tonsil cancers with average deep resection margins of only 1.98mm 3
- Therefore, favourable outcomes can be achieved provided microscopically clear margins are achieved
When is reconstruction required?
- An exposed carotid artery must be covered with a flap (note: full thickness removal of the pharyngeal constrictor muscle with extension into PPS fat is an indication for a combined open and transoral approach. This approach also provides access for flap inset, and is a natural extension of neck dissection, management of ECA)
- Significant resection of soft palate can cause palatal incompetence that manifests as nasopharyngeal reflux and impaired speech
- Function does improve as the tumor bed scars and contracts with time
- It remains a judgement call when reconstruction of the palate is required to prevent these sequelae
- Options include
- Local palatal flaps e.g. rotating uvula into the defect
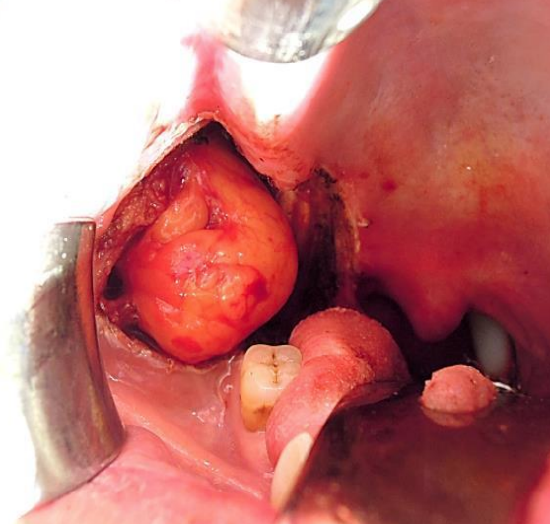
Figure 25: Buccal fat pad flap used to augment the palate or to close a pharyngocervical communication
- Buccal fat pad flap (Figure 25)
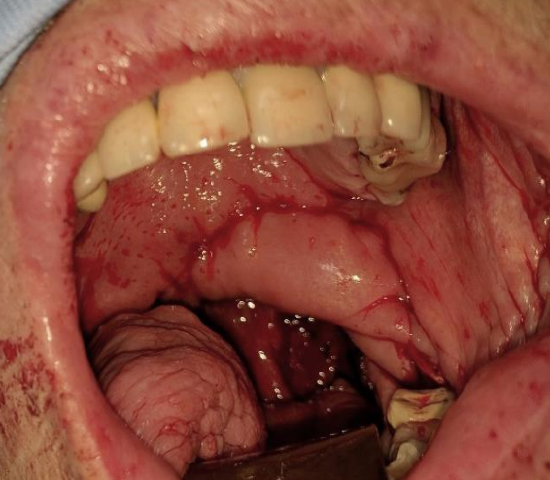
Figure 26: Soft palate and tonsil fossa defect reconstructed with buccinator flap
- Buccinator myomucosal flap (Figure 26)
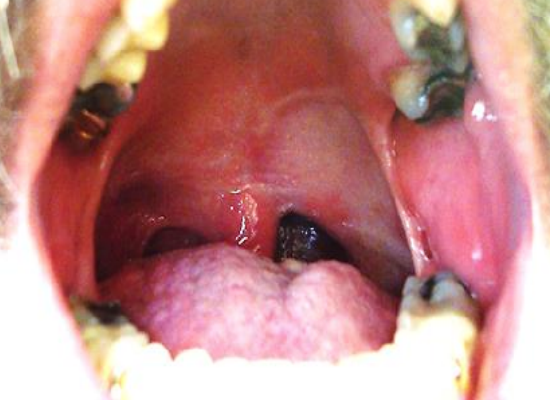
Figure 27: Radial free forearm flap reconstruction of oropharynx and soft palate defect
- Radial free forearm flap (Figure 27)
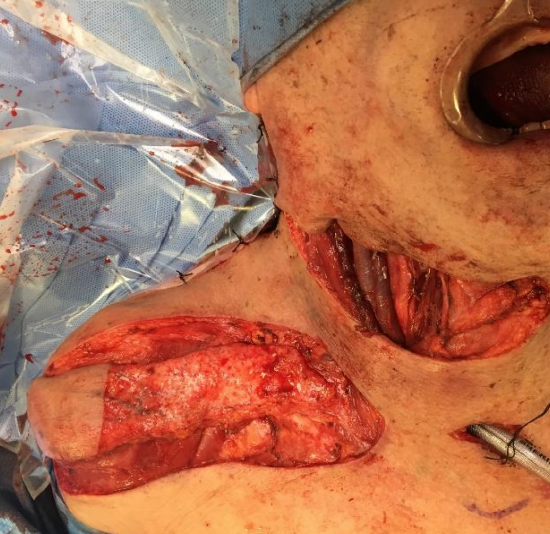
Figure 28: Supraclavicular flap
- Supraclavicular flap (Figure 28)

Figure 29: Submental artery island flap
- Submental artery island flap (Figure 29)
- Pectoralis major flap
- Anterolateral free thigh flap
Neck dissection
- Oropharyngeal squamous carcinomas generally need to have the N0 neck treated either surgically or with (chemo) radiation
- Neck dissection is ideally done at the same operation, but may be staged
- There is a risk of causing a communication between the pharynx and submandibular triangle at the tonsillolingual sulcus
- A communication can be avoided by
- Cutting through the submandibular gland with cautery, leaving the deep portion of the gland in situ
- Leaving the whole submandibular gland in situ, taking care to clear the facial nodes (there are no intraglandular lymph nodes)
- Should a communication occur, then it can be dealt with by
- Suturing the free margin of the mylohyoid to the posterior belly of digastric and avoiding placing the tip of the suction drain close to Level 1
- Repairing the defect with a flap
- Buccal fat pad flap (Figure 25)
- Buccinator myomucosal flap (Figure 26)
- Radial free forearm flap (Figure 27)
- Supraclavicular flap (Figure 28)
- Submental artery island flap (Figure 29)
- Pectoralis major flap
- Anterolateral free thigh flap
Feeding tube
It is simpler to remove a nasogastric feeding tube the day following surgery, than to have to insert it should the patient struggle to swallow.
Tracheostomy
Tracheostomy may be considered for two reasons i.e. concerns about the airway (edema, soft tissue reconstruction, patient factors) or when there are concerns about postoperative bleeding. It remains a judgement call by the surgeon in consultation with the anesthetist.
Salvage surgery
Salvage surgery may be considered following previous transoral resection and/or chemoradiation. It requires a higher level of surgical skill and experience, and a very detailed radiological assessment of resectability via a transoral approach. When concerns exist about injuring the ICA, the ICA may first be exposed via Level 2 of the neck and gauze packed anterior to the ICA in the PPS to protect it during the transoral phase of the dissection.
References
- Weinstein GS, O’Malley BW, Rinaldo A et al. Eur Arch Otorhinolaryngol 2015; 272 (7): 1551-2 https://doi.org/10.1007/s00405-014-3331-9
- Faraji F, Coquia SF, Wenderoth MB, Padilla ES, Blitz D, DeJong MR, Aygun N, Hamper UM, Fakhry C. Evaluating oropharyngeal carcinoma with transcervical ultrasound, CT, and MRI. Oral Oncology. 2018: 78:177-85
- Hinni ML, Zarka MA, Hoxworth JM. Margin mapping in transoral surgery for head and neck cancer. Laryngoscope. 2013 May;123(5):1190-8
Additional reading
- Chapter in Open Access Atlas of Otolaryngology Head and Neck Operative Surgery: Oropharyngeal cancer resection
- Gun R, Durmus K, Kucur C, et al. Transoral Surgical Anatomy and Clinical Considerations of Lateral Oropharyngeal Wall, Parapharyngeal Space, and Tongue Base. Otolaryngol Head Neck Surg. 2016 Mar;154(3):480-5
Author
Wayne M. Koch, MD
Professor of Otolaryngology-Head & Neck Surgery
Johns Hopkins University
Baltimore, MD 21287 USA
wkoch@jhmi.edu
Author & Editor
Johan Fagan
MBChB, FCS (ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


