4.9: Endoscopic Ethmoidectomy (FESS) Surgical Technique
- Page ID
- 48897
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
ENDOSCOPIC ETHMOIDECTOMY (FESS) SURGICAL TECHNIQUE
Pedro Monteiro, Darlene Lubbe
Endoscopic ethmoidectomy refers to exenteration of the anterior +/- posterior ethmoid cells.
The ethmoids are in close proximity to the orbit and its contents, the optic nerve, the sphenoid sinus, the paper-thin cribriform plate with meninges above, the ethmoidal arteries and the olfactory nerves. Like all endoscopic sinus surgery, the anatomy and surgical technique are best learned on a cadaver, followed by surgery under direct supervision of an experienced endoscopic sinus surgeon. Ethmoidectomy done by a surgeon unfamiliar with the detailed anatomy of the nose and paranasal sinuses, especially in the absence of a CT scan or when unable to properly interpret a CT scan, or by a surgeon untrained in endoscopic sinus surgery, is high-risk.
This chapter presents the relevant anatomy, indications for surgery, preoperative workup, surgical instrumentation, anesthesia, surgical technique, postoperative care and pitfalls of endoscopic ethmoidectomy.
Relevant Anatomy
Ethmoid Bone
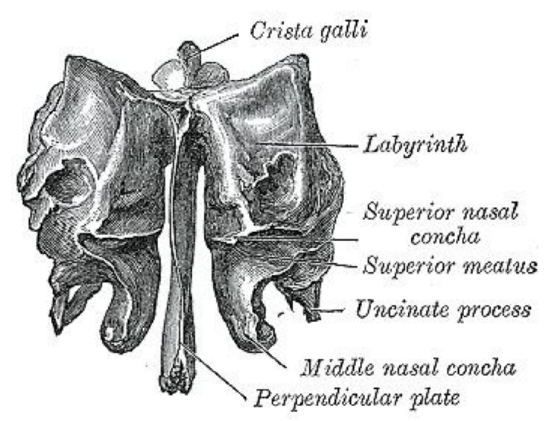
Figure 1: Anterior view of ethmoid bone demonstrating cribriform plate, crista galli, perpendicular plate, and labyrinths
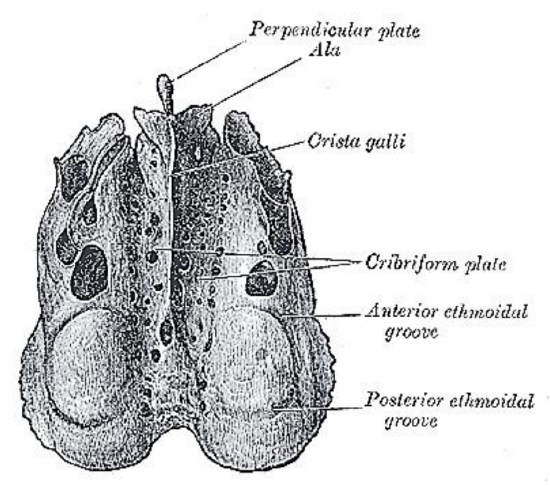
Figure 2: Superior view of ethmoid bone
The ethmoid has 3 parts: cribriform plate; perpendicular plate; and labyrinths/ lateral masses (Figures 1, 2).
Cribriform plate
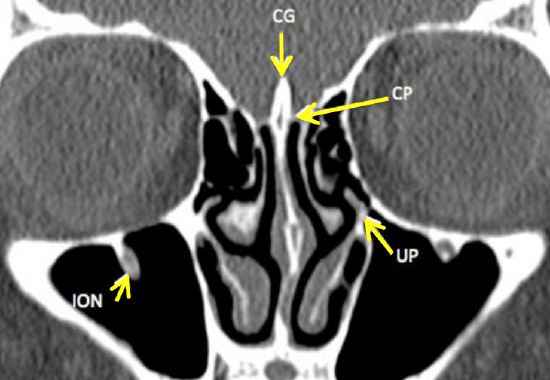
Figure 3: Coronal CT scan through the anterior ethmoids demonstrates the cribriform plate (CG = crista galli, CP = cribriform plate, UP = uncinate process, ION = inferior orbital nerve (V2))

Figure 4: Falx cerebri attaches to crista galli, and foramen caecum contains the emissary vein
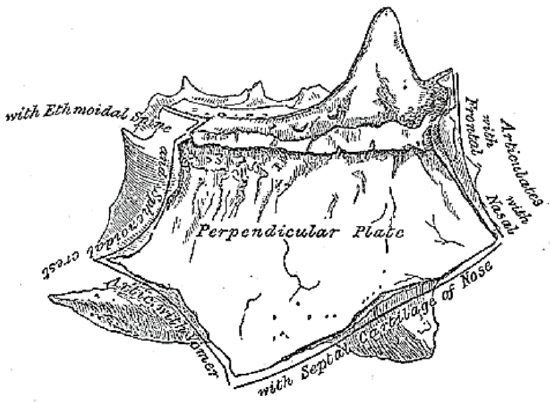
Figure 5: Ethmoid bone, lateral view
The cribriform plate is a paper-thin bone that forms the roof of the nasal cavity and the medial roof of the ethmoids (Figures 2, 3). It articulates with the ethmoidal notch of the frontal bone anteriorly (Figure 2). The crista galli projects superiorly from the cribriform plate in the midline and is in contact with the falx cerebri along its posterior border (Figure 4). Two projecting alae (Figures 2, 5) help complete the foramen caecum which contains the emissary vein that drains to the superior sagittal sinus (Figure 4).
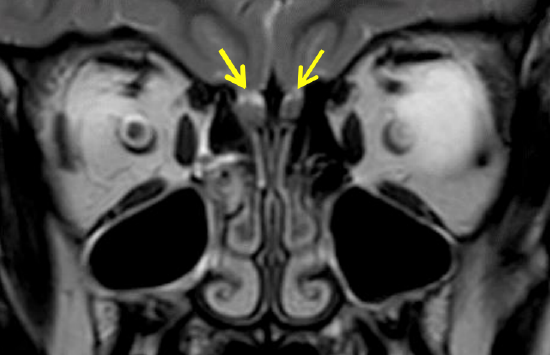
Figure 6: Coronal MRI demonstrating the olfactory bulbs (arrows) to either side of the crista galli
The cribriform plate is narrow and deeply grooved on either side of the crista galli where it contains the olfactory bulbs (Figures 3, 6) from which olfactory fibers pass through multiple foramina in the cribriform plate to the superior turbinate, upper nasal septum and middle turbinate.
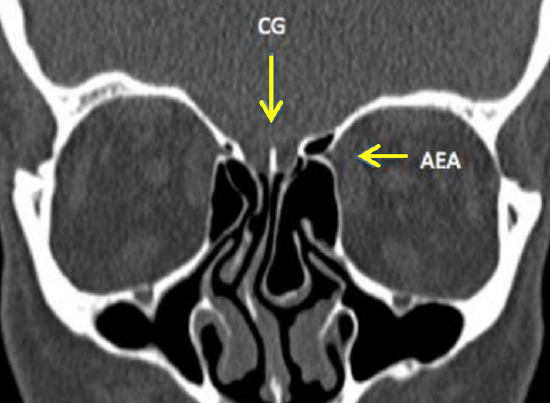
Figure 7: Coronal CT scan of fissure to either side of crista galli (CG) and a foramen transmitting the nasociliary nerve and anterior ethmoidal artery (AEA)
In the anterior cribriform plate is a fissure to either side of the crista galli that is occupied by a process of dura mater. Lateral to this fissure, a foramen transmits the nasociliary nerve and anterior ethmoidal artery (Figure 7).
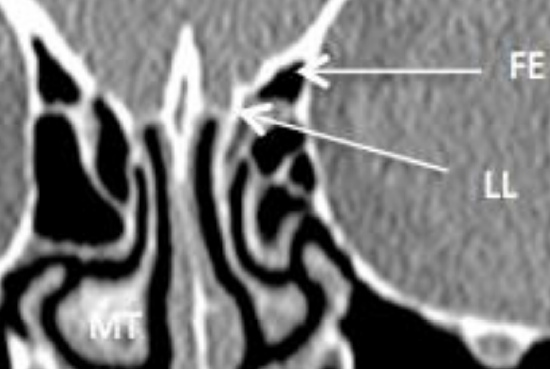
Figure 8: Coronal CT scan demonstrating the fovea ethmoidalis (FE), lateral lamella of the cribriform plate (LL) and middle turbinate (MT)
The roof of the ethmoids is a high-risk surgical area due to its proximity to dura and brain, the risk of causing a CSF leak and meningitis, and its relations to the anterior ethmoidal artery. Laterally it is formed by a thicker horizontal portion (fovea ethmoidalis), and medially by a thinner vertical portion (lateral lamella of cribriform plate) (Figure 8). The superior/vertical attachment of the vertical lamella of the middle turbinate divides the anterior skull base into the cribriform plate medially and the fovea ethmoidalis laterally.
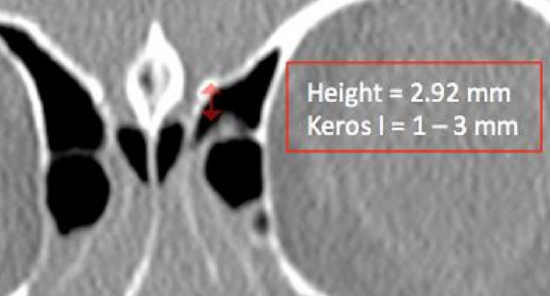
Figure 9a: Keros classification: Type I = 1-3 mm (15%)
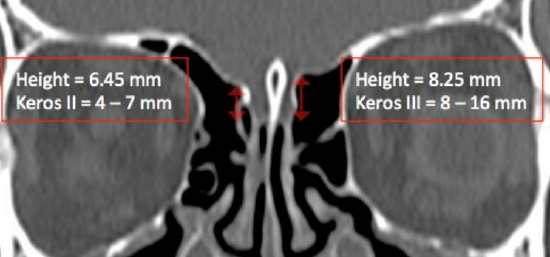
Figure 9b: Keros classification: Type II = 4-7 mm (70%), Type III = 8-16 mm (15%). Note that Keros classification can be different on either side
The lateral lamella of the cribriform plate is only 0.05 - 0.2 mm thick and is at high risk of injury during surgery. The Keros classification describes the depth of the olfactory fossae (Figures 9a, b). It is a measurement of the height of the lateral lamella at its highest point and is measured from the fovea ethmoidalis to the cribriform plate. This measurement is asymmetrical in up to 15% of patients. A higher value is associated with increased risk of cribriform plate injury, CSF leaks and injury to the anterior ethmoidal artery.
Perpendicular plate of ethmoid
The perpendicular plate of the ethmoid is an inferior vertical projection below cribriform plate of the crista galli and forms the upper part of the posterior bony septum (Figures 1, 5). Anterosuperiorly it articulates with the spines of the frontal and nasal bones; posteriorly it articulates with the sphenoidal crest and vomer; and anteroinferiorly with the quadrangular cartilage of the nasal septum (Figure 5).
Labyrinths / lateral masses
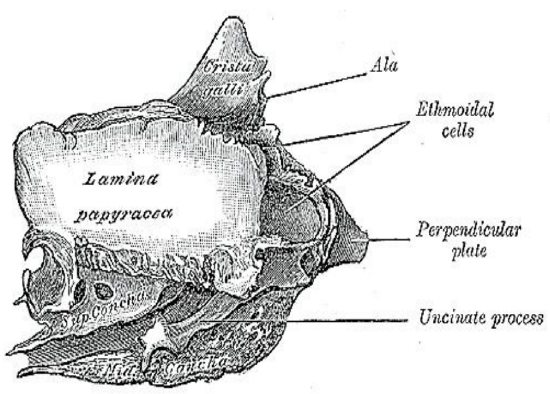
Figure 10: Lateral view of the right lamina papyracea which constitutes the lateral wall of the ethmoid sinuses
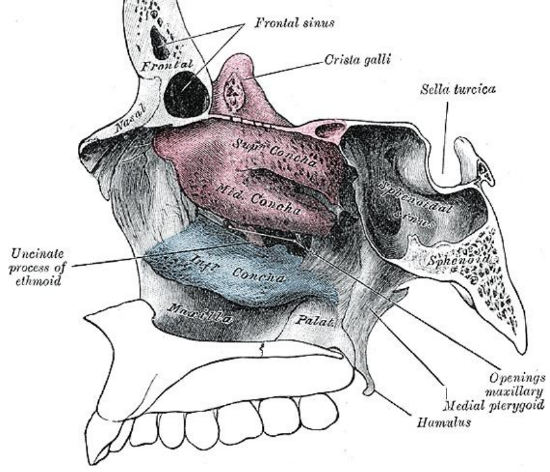
Figure 11: Medial view of the ethmoid bone and the ethmoid sinuses
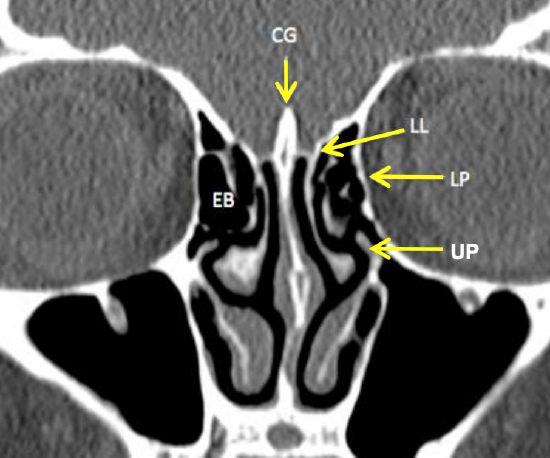
Figure 12: Coronal CT scan of ethmoid sinuses demonstrating the lamina papyricea and the vertical lamella of the middle turbinate (LL = lateral lamella of cribriform plate, LP = lamina papyracea, EB = ethmoidal bulla, UP = Uncinate process)
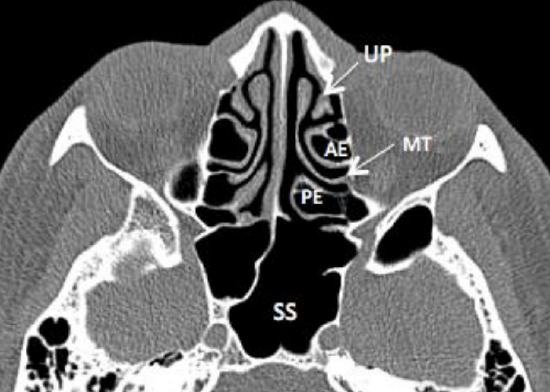
Figure 13: Axial CT demonstrating uncinate process (UP), anterior ethmoids (AE), basal (ground) lamella of middle turbinate (MT), posterior ethmoids (PE) and sphenoid sinus (SS)
The labyrinths (lateral masses) contain the ethmoid cells that are exenterated during ethmoidectomy. They consist of numerous thin-walled cavities known as ethmoidal cells or ethmoid sinuses and lie between two vertical bony plates i.e. the orbital plate (lamina papyracea) laterally and the basal or vertical lamella of the middle turbinate medially (Figures 10, 11, 12, 13).
It is crucial to carefully study the CT scans preoperatively to detect aberrations of sinus anatomy and to avoid losing your way while traversing the sinuses; hence the need to understand variations of ethmoid anatomy.
Recognised groups of ethmoid cells are:
- Anterior ethmoidal cells
- Agger nasi
- Haller cells
- Frontal / frontoethmoidal cells
- Suprabullar cells
- Frontal bullar cell
- Supraorbital ethmoidal cell
- Posterior ethmoidal cells
- Onodi cell
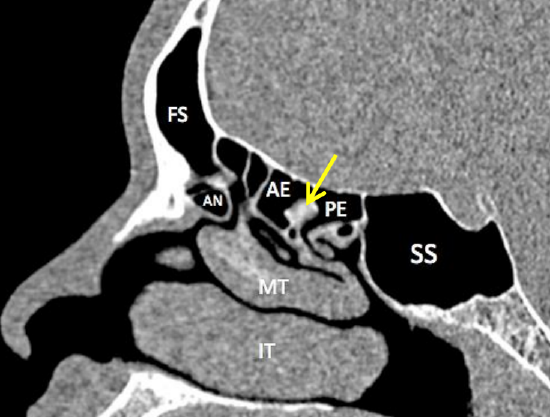
Figure 14: Sagittal view through ethmoids to demonstrate frontal sinus (FS), agger nasi (AN), anterior ethmoids (AE), basal/ ground lamella (yellow arrow), posterior ethmoids (PE) and sphenoid sinus (SS)
The anterior ethmoidal cells are separated from the posterior ethmoidal cells by the basal/ground lamella, which is the lateral extension of the middle turbinate at its posterior end (Figure 14). The anterior ethmoidal cells drain into the middle meatus.
The posterior ethmoidal cells are situated posterior to the basal lamella of the middle turbinate. They drain into the superior meatus.
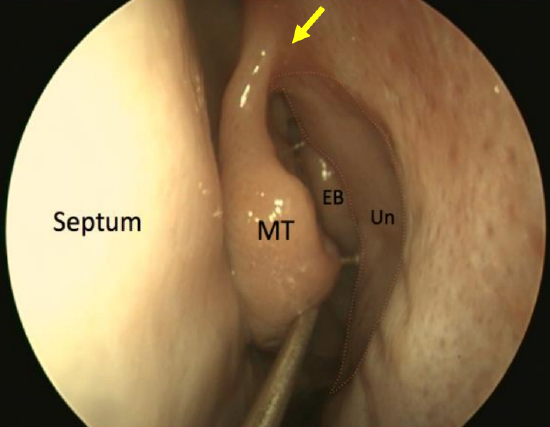
Figure 15: Endoscopic view of left ethmoid bulla (EB) in the middle meatus, behind the sickle shaped uncinate process (Un). Arrow points to “axilla”
The ethmoidal bulla (bulla ethmoidalis) is a constant landmark during ethmoid surgery and is the largest anterior ethmoid air cell. It lies posterior to the uncinate process (Figures 15).

Figure 16: Coronal CT shows agger nasi cell (AN), inferior (IT) and middle turbinates (MT), and maxillary sinus (MS)
The agger nasi is the most anterior ethmoid air cell (Figures 14, 16). It is located in the lacrimal bone anterior and superior to the axilla, which is the attachment to the lateral nasal wall of the middle turbinate (Figure 15). The agger nasi is present in 90% of CT scans, and is the 1st anterior ethmoidal cell to become pneumatized. It is seen just superior to the lacrimal sac on coronal CT scan (Figure 16). The posterior wall of the agger nasi forms the anterior boundary of frontal recess (Figure 14), and its medial wall is closely related to the vertical lamella of middle turbinate (Figure 16). The superior part of the uncinate process forms the medial wall of the agger nasi. Laterally it is bounded by the lamina papyracea (Figure 16).
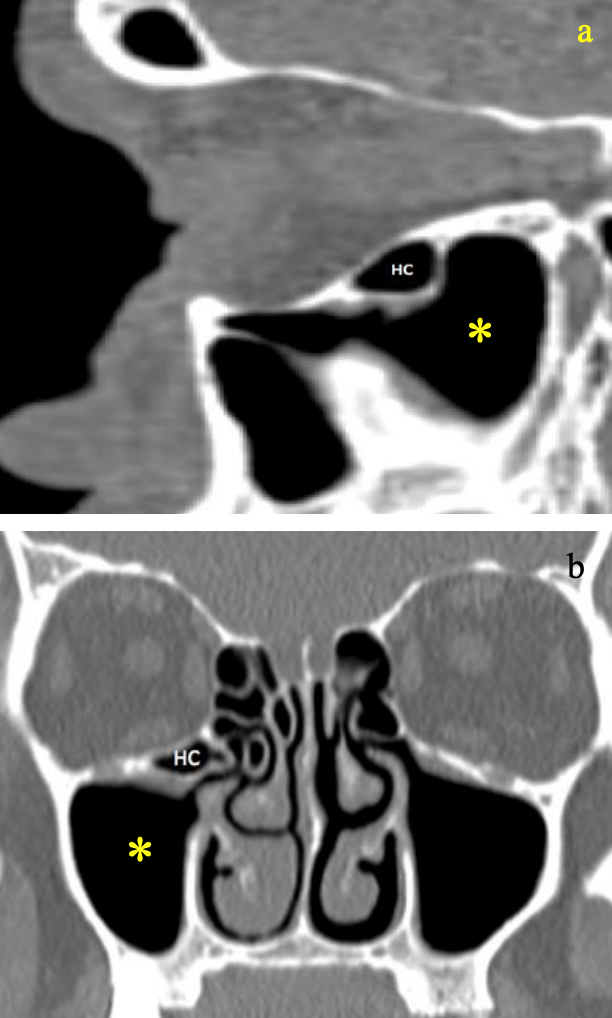
Figures 17a, b: Sagittal (above) and coronal (below) CTs demonstrating Haller cell (HC) extending into maxillary sinus *
Haller cells are anterior ethmoid air cells extending into the maxillary sinus (Figure 17). They can obstruct the outflow tract of the maxillary sinus and must be removed when there is pathology within the maxillary sinus. These cells are important to identify preoperatively on CT scan if surgery to the maxillary sinus is anticipated.
Frontal cells, also referred to as frontoethmoidal cells, are anterior ethmoid cells that pneumatise the frontal recess/sinus above the agger nasi. Bent & Kuhn classified these frontal cells into 4 types:
- Type I: Single cell above agger nasi not extending into frontal sinus (25%)
- Type II: Group of cells (>2) above agger nasi cell but below orbital roof (5%)
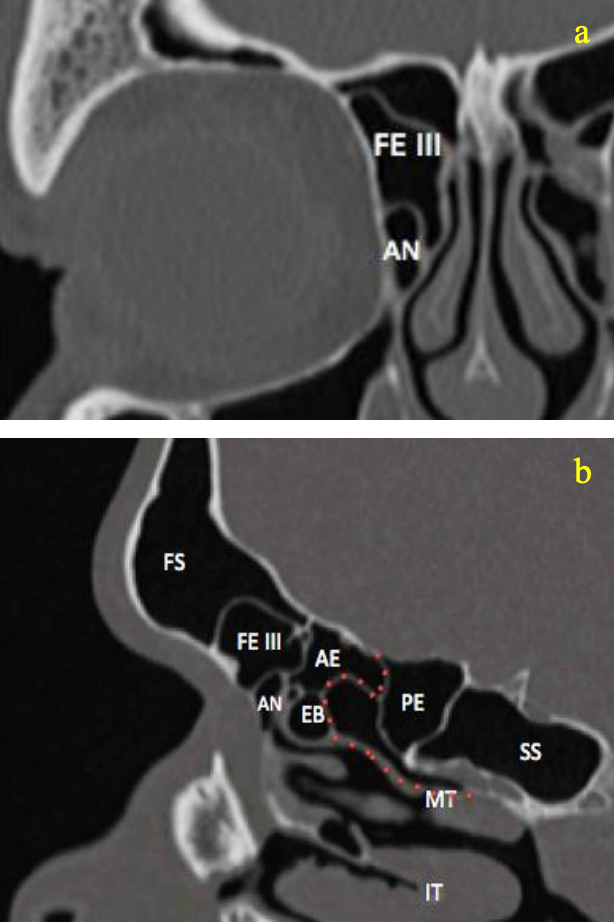
Figures 18a, b: Coronal and sagittal CTs demonstrate Type III Kuhn cell: extension into frontal recess (FE III), agger nasi (AN), ethmoid bulla (EB), anterior ethmoid cell (AE), posterior ethmoid cell (PE), sigmoid sinus (SS), inferior turbinate (IT) and middle turbinate (MT) with basal lamella (red dotted line)
- Type III: Single cell extending from agger nasi into frontal sinus (3%) (Figure 18)
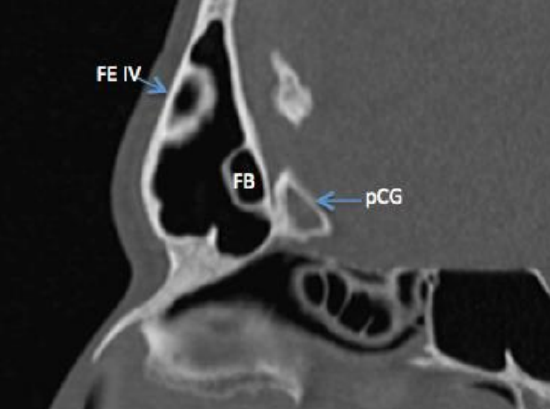
Figure 19: Sagittal CT demonstrating a Type IV Kuhn cell (isolated cell within the frontal sinus) as well as frontal bullar cell (pneumatizes along skull base within the frontal sinus)
- Type IV: Isolated cell within frontal sinus, not contiguous with agger nasi (<1%) (Figure 19)
Excessive pneumatization of these cells (especially Types III and IV) may obstruct the frontal recess and predispose to frontal sinus disease.
Suprabullar cells are anterior ethmoidal air cells located above the bulla ethmoidalis and extend towards the frontal recess, but not into the frontal sinus.
A frontal bullar cell is a suprabullar cell that pneumatizes from the posterior frontal recess and pneumatizes along the skull base into the frontal sinus (Figure 19).
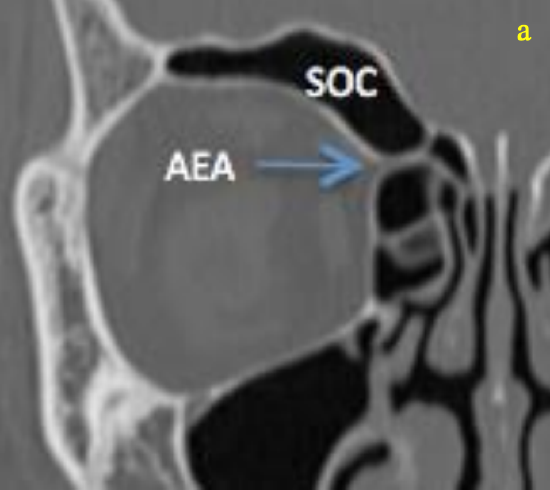
Figure 20a: Coronal CTs demonstrating a supraorbital ethmoid air cell (SOC). It can be distinguished from the frontal sinus by pneumatization posterior to the anterior ethmoidal artery (AEA)
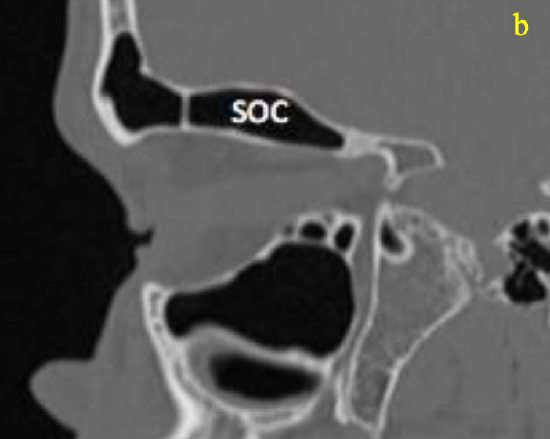
Figure 20b: Sagittal CTs demonstrating a supraorbital ethmoid air cell (SOC) with pneumatization seen posterior to the anterior ethmoidal artery
A supraorbital ethmoidal cell is a suprabullar anterior ethmoidal air cell that arises behind the frontal recess and extends over the orbit by pneumatizing the orbital plate of the frontal bone (Figures 20a, b). When it is large, it may be mistaken for the frontal sinus and it may obstruct the frontal recess.
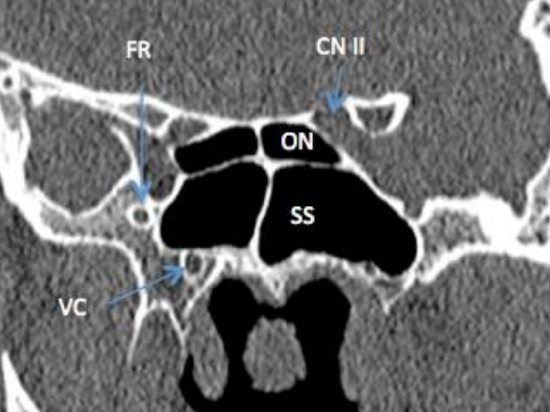
Figure 21: Coronal CT demonstrating proximity of Onodi cell (ON) to optic nerve (CN II)
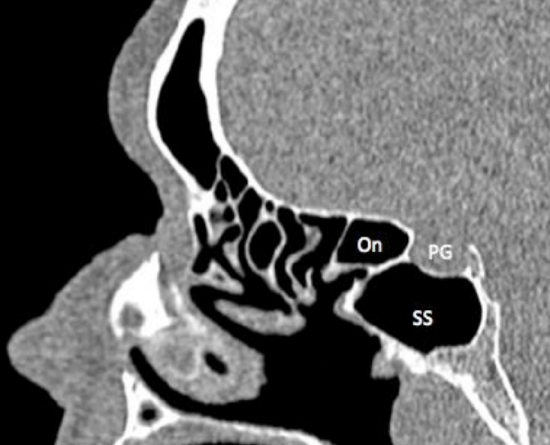
Figure 22: Sagittal CT demonstrating Onodi cell (On), pituitary gland (PG) and sphenoid sinus (SS)
An Onodi cell is a posterior ethmoid (sphenoethmoidal) cell that extends superior and often lateral to the sphenoid sinus (Figures 21, 22).
Horizontal septations within the sphenoid sinus seen on CT represent an Onodi cell, with the Onodi cell being the posterolateral cell at the level where the horizontal septation is seen (Figures 21, 22). It is found in up to 25% of patients, and is important to identify on a preoperative CT scan because if there is no sphenoid sinus behind it (because the sphenoid sinus is below the Onodi cell), then the middle cranial fossa is immediately behind the Onodi cell. It is often closely related to the optic nerve and the nerve is therefore at great risk during posterior ethmoid surgery. There is an increased risk of optic nerve injury (15% dehiscent in Onodi cell), carotid artery injury (20% dehiscent in Onodi cell) or brain injury.
Anatomy of turbinates, uncinate process, lamina papyracea and lateral nasal wall
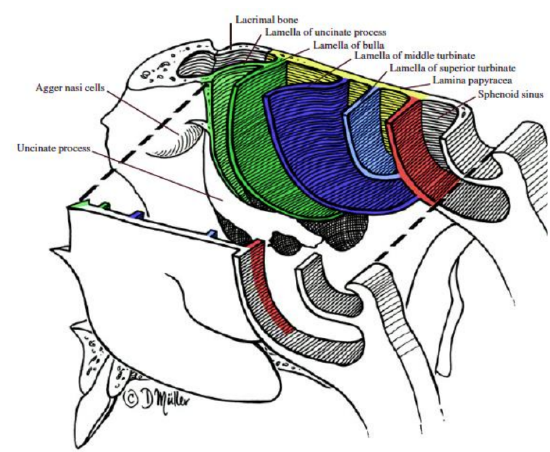
Figure 23: Messerklinger’s 5 lamellae
Messerklinger described 5 lamellae (bony structures) that traverse the ethmoids and extend from the lamina papyracea laterally to the cribriform plate superiorly and between fovea ethmoidalis and the frontal bone (Figure 23).
1st Lamella: Uncinate process (incompletely developed lamella)
2nd Lamella: Bulla lamella (pneumatization of this lamella forms the ethmoidal bulla)
3rd Lamella: Ground / basal lamella of the middle turbinate (most constant and completely formed lamella)
4th Lamella: Superior turbinate
5th Lamella: Supreme turbinate (only occasionally present)
Middle turbinate
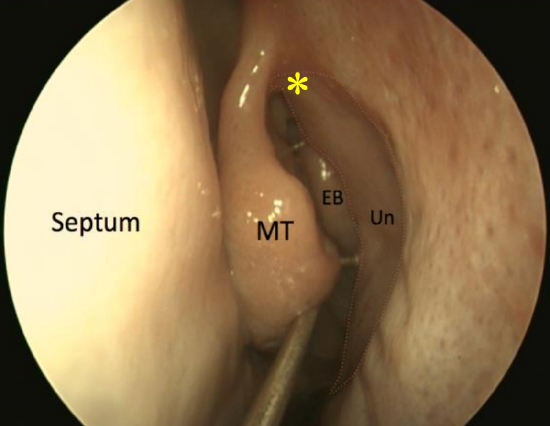
Figure 24: Endoscopic view of (L) ethmoid bulla (EB) in the middle meatus, behind the uncinate process (Un), and the axilla (*)
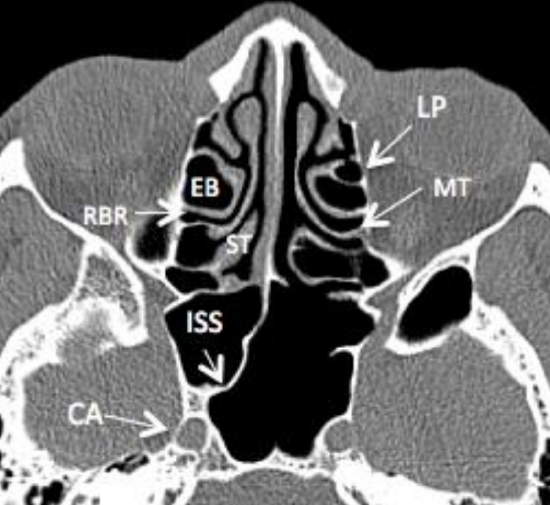
Figure 25: Axial CT scan of ethmoid sinuses demonstrates the lamina papyracea (LP), the basal or ground lamella of the middle turbinate (MT), ethmoidal bulla (EB), retrobullar recess (RBR), superior turbinate (ST), intersinus septum of sphenoid (ISS), and its relation to carotid artery (CA)
Because it is a key anatomical landmark during sinus surgery, the middle turbinate should always be preserved. The middle turbinate is part of the ethmoid bone. It comprises vascular, erectile glandular tissue on spongy bone and is lined by pseudostratified columnar ciliated respiratory epithelium. Anteriorly it fuses with the agger nasi to form the axilla (Figure 24). Superiorly it attaches to the lateral lamella of the cribriform plate in a sagittal plane. Posteriorly it rotates to lie in a coronal plane (basal lamella) and attaches to the lamina papyracea, thereby separating the anterior from the posterior ethmoid cells (Figure 25). Posterior to the sphenopalatine foramen it attaches to the perpendicular plate of the palate in a horizontal plane.
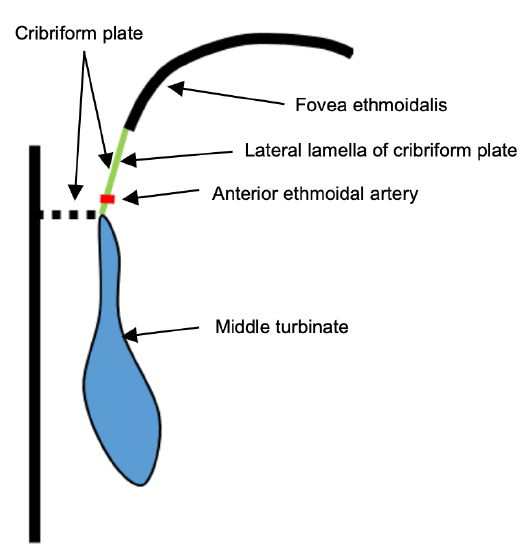
Figure 26a: Anatomy of middle turbinate: Coronal cut through anterior ethmoids demonstrating paper-thin cribriform plate, thicker fovea ethmoidalis, and point where anterior ethmoidal artery traverses the lateral lamella of the cribriform plate
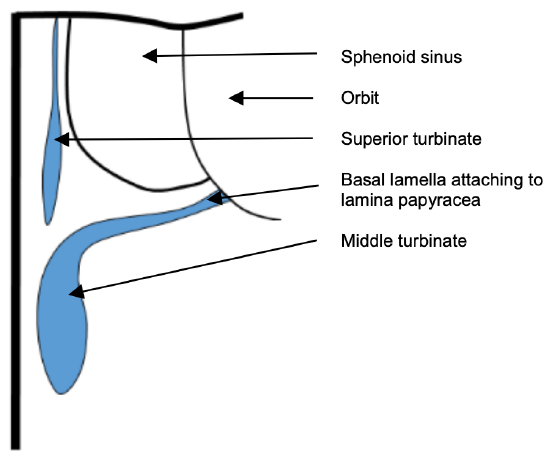
Figure 26b: Anatomy of middle turbinate: Coronal view to illustrate the ground lamella running horizontally and attaching to lamina papyracia to separate the anterior and the posterior ethmoids
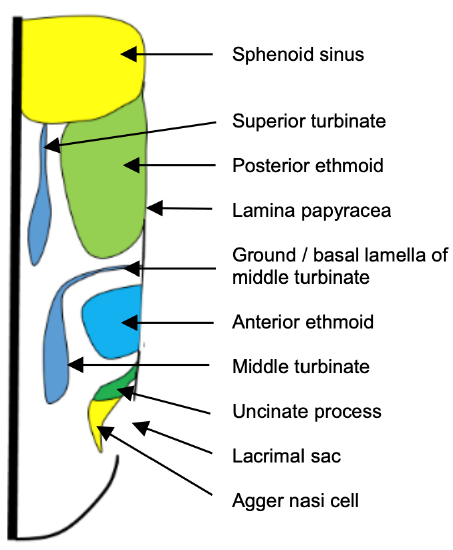
Figure 26c: Anatomy of middle turbinate: Axial view to illustrate the ground lamella separating the anterior and posterior ethmoids
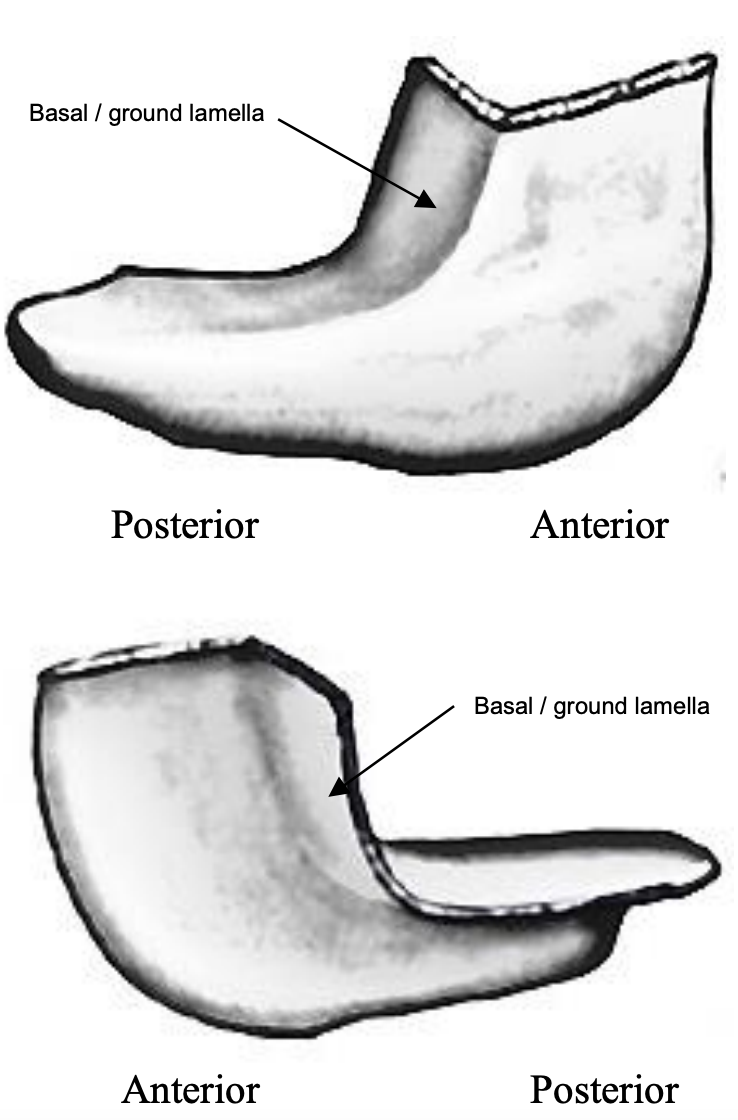
Figure 27: Shape of (L) middle turbinate
The basal (ground) lamella is the lateral extension of the middle turbinate that attaches to the lamina papyracea. It is an important surgical landmark to identify during surgery as it separates the anterior from the posterior ethmoid cells (Figures 25, 26, 27).
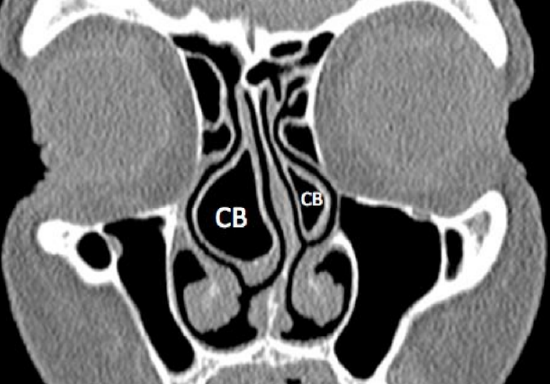
Figure 28: Concha bullosa (CB)
A concha bullosa is a pneumatized middle turbinate and is present in up to 50% of people (Figure 28).
Even though it may obstruct the ostiomeatal complex and predispose to acute or chronic rhinosinusitis, most people with concha bullosae are asymptomatic. A concha may impede access to the middle meatus and need to be reduced prior to uncinectomy or ethmoidectomy.
The middle turbinate must be handled with great care for the following reasons:

Figure 29: Middle turbinate (MT) attaches to paper-thin cribriform plate above, which is especially thin medially. Note the then lamina papyracea (LP)
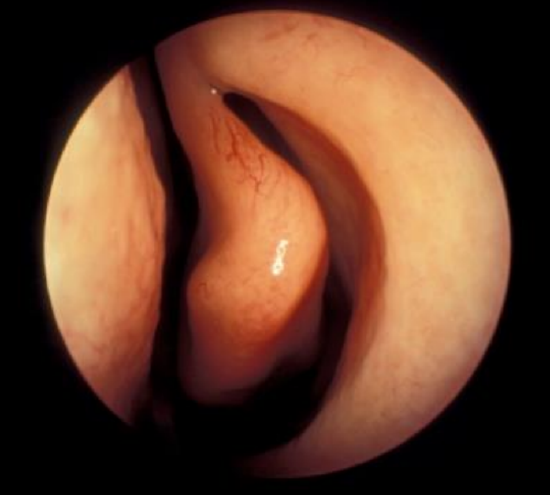
Figure 30: Paradoxical middle turbinate curving away from the middle meatus
- It is attached to the paper-thin cribriform plate above; excessive manipulation of the turbinate can fracture the cribriform plate and cause a CSF leak (Figure 29)
- The cribriform plate is very thin medial to the turbinate; hence surgeons should avoid this area during surgery (Figure 29)
- The olfactory area of the nose is located between the turbinate and the septum; hence surgery and consequently adhesions occurring medial to the turbinate can cause anosmia
- The lateral extension of the middle turbinate called the basal/ground lamella, divides the anterior from the posterior ethmoid air cells and should be identified at surgery as an anatomical landmark
- The free edge of the middle turbinate typically faces medially towards the middle meatus, but can also paradoxically face laterally (Figure 30)
Uncinate process
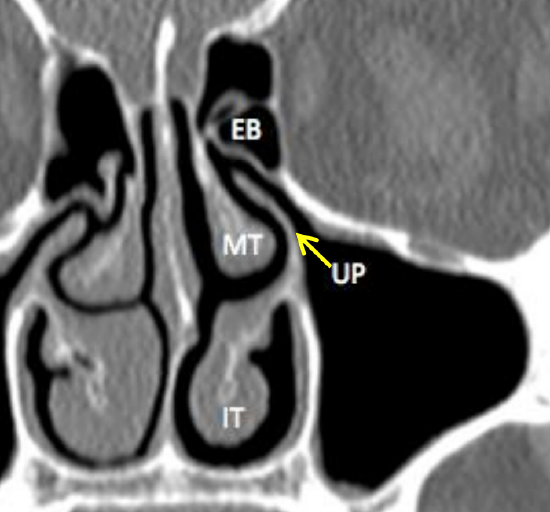
Figure 31: Coronal CT scan demonstrating the uncinate process (UP), ethmoidal bulla (EB), middle turbinate (MT), inferior turbinate (IT). Note close proximity of uncinate process to orbital wall
The uncinate process is a thin, sickle-shaped projection of ethmoid bone that is encountered anteriorly in the lateral nasal wall (Figures 10, 11, 12, 13, 23, 24, 30, and 31). Removing the uncinate provides access to the hiatus semilunaris and the ethmoidal bulla. It has a free posterior edge which lies anterior to the ethmoidal bulla (Figure 23). The uncinate attaches to the posterior edge of the lacrimal bone anteriorly and to the superior edge of the inferior turbinate inferiorly, and has a free edge posteriorly covered by mucosa. Superiorly it has a variable attachment to the lamina papyricea, fovea ethmoidalis or middle turbinate. This superior attachment influences the frontal sinus drainage pathway (either medial to, or directly into superior ethmoid infundibulum). Note its close proximity to the orbital wall (Figure 31), which may be injured should surgeon use poor surgical technique. The uncinate process may be pneumatized and cause obstruction to the infundibulum or have more than one attachment superiorly.
Lamina papyracea (Figures 26, 32)
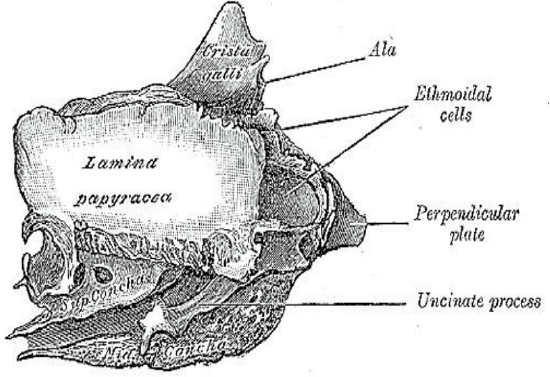
Figure 32: Lateral view of the right lamina papyracea which constitutes the lateral wall of the ethmoid sinuses
The lateral wall of the labyrinth is formed by the orbital plate of the ethmoid (lamina papyracea). It articulates with the orbital plate of the frontal bone superiorly, the maxillary and orbital processes of the palatine inferiorly, the lacrimal bone anteriorly and the sphenoid posteriorly (Figure 29).
Maxillary sinus ostium (Figure 33)
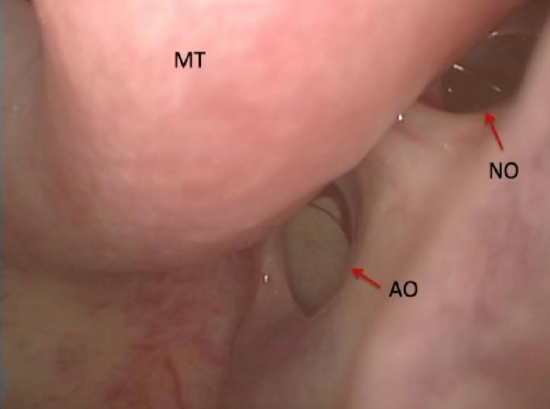
Figure 33: Left natural maxillary sinus ostium (NO) and accessory ostium (AO)
The maxillary sinus ostium is located on the supermedial aspect of the maxillary sinus. It opens into the ethmoidal infundibulum. The natural ostium is typically oval shaped and orientated obliquely. The natural ostium is not visible under endoscopic visualization unless the uncinate process has been removed.
Anterior and posterior fontanelles and accessory ostia (Figure 33)
The anterior and posterior fontanelles are bony defects in the medial wall of the maxillary sinus above the inferior turbinate. The fontanelles are covered only by mucosa and connective tissue. Defects in the fontanelles are called accessory ostia (Figure 33). They are more commonly located posteriorly and are spherical with the long axis in a horizontal plane.
Anatomy of ostiomeatal complex, meati and recesses
Ostiomeatal complex (Figure 34)
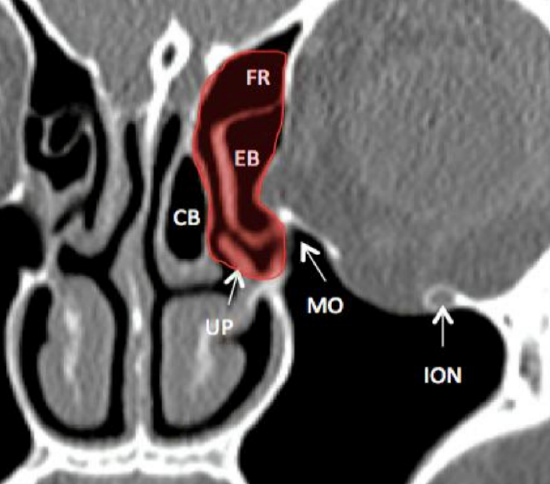
Figure 34: Coronal CT demonstrating the ostiomeatal complex (shaded red) and how a pneumatised middle turbinate (concha bullosa) may impede access to the middle meatus. Frontal recess (FR), ethmoidal bulla (EB), concha bullosa (CB), uncinate process (UP), natural maxillary ostium (MO), inferior orbital nerve (ION)
This is a functional unit which is the common drainage pathway for the frontal, maxillary and ethmoid sinuses. It includes the ethmoidal infundibulum, middle turbinate, ethmoidal bulla, uncinate process, hiatus semilunaris and frontal recess.
Middle meatus (Figure 35)
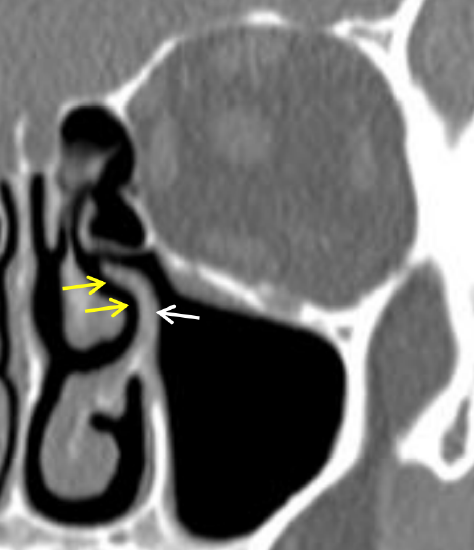
Figure 35: Yellow arrows point to middle meatus between middle turbinate and lateral wall of nose, and uncinate process (white arrow)
The middle meatus is the curved anteroposterior passage above the superior border of the inferior turbinate, between the middle turbinate and lateral nasal wall.
Hiatus semilunaris (Figures 36, 37)
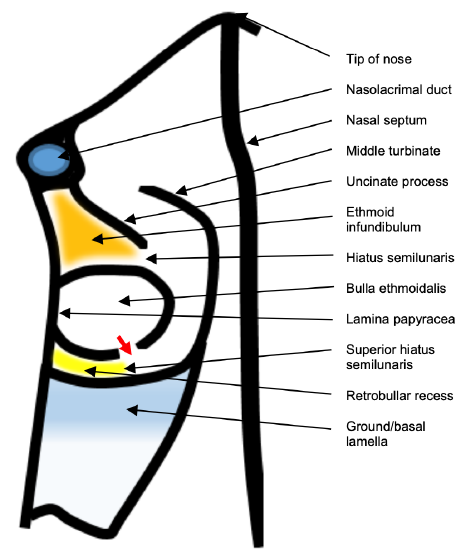
Figure 36: Superior axial view of hiatus semilunaris, ethmoidal infundibulum, superior hiatus semilunaris, retrobullar recess, ethmoidal bulla; nasolacrimal duct, uncinate process, lamina papyracea; ground/ basal lamella, and middle turbinate
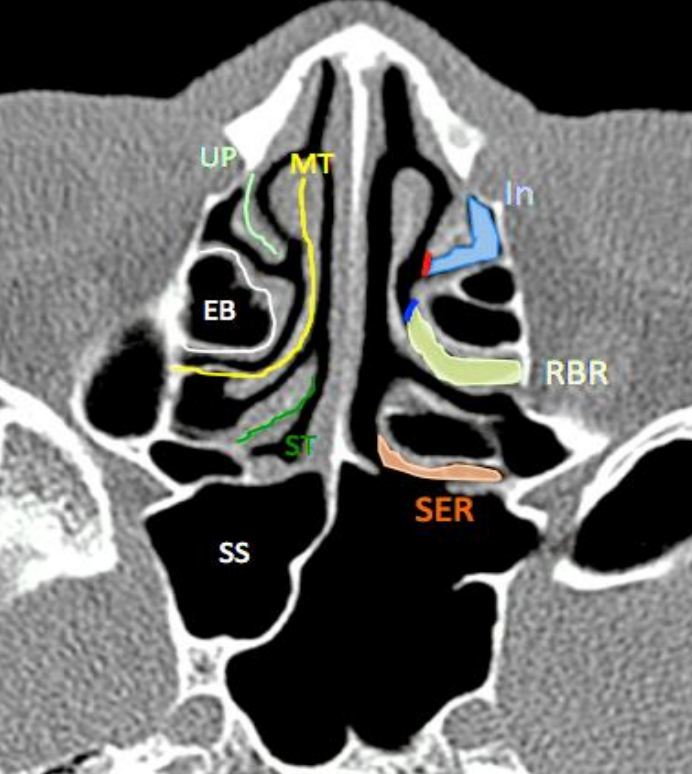
Figure 37: Axial CT demonstrating the relationships of various structures, clefts and spaces. Hiatus semilunaris (red line), uncinate process (UP), middle turbinate (MT), ethmoidal bulla (EB), superior turbinate (ST), sphenoid sinus (SS), ethmoidal infundibulum (In), retrobullar recess (RBR), sphenoethmoidal recess (SER)
The hiatus semilunaris is the ‘entrance’ to the ethmoidal infundibulum. It is a 2-dimensional opening between the free posterior edge of the uncinate process and the anterior face of the bulla ethmoidalis.
Ethmoidal infundibulum (Figures 36, 37)
This is a 3-dimensional space bound by the uncinate process medially, maxillary sinus ostium inferiorly, lamina papyracea and frontal process of maxilla (+/- lacrimal bone) laterally and the ethmoidal bulla posteriorly. Anteriorly it ends blindly in an acute angle where the uncinate process attaches to the lateral nasal wall and has a variable superior configuration depending on the attachment of the uncinate process (either ending blindly in the recessus terminalis if the attachment is to lamina papyracea, or into the frontal recess if attached to the skull base or middle turbinate)
Retrobulbar recess (Figures 36, 37)
The retrobullar recess is a space that may be present between the posterior surface of the bulla ethmoidalis and the basal lamella.
Suprabullar recess
The suprabullar recess may be present between the superior surface of the bulla and the fovea ethmoidalis.
Sphenoethmoidal recess (Figures 37, 38)
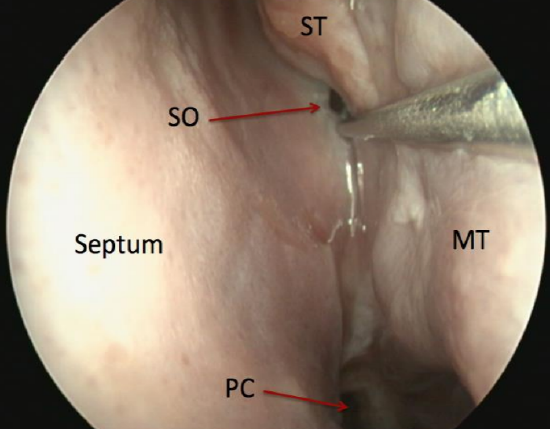
Figure 38: View of the sphenoid sinus ostium (SO) in sphenoethmoidal recess; this ostium is 3 sucker tips above the posterior choana (PC)
The sphenoethmoidal recess lies anterior to the sphenoid face (anterior wall of sphenoid) and medial to the superior turbinate. The sphenoid ostium is located medial to the superior turbinate (85%) at a level horizontal to the superior border of the natural maxillary ostium.
Anatomy of arteries
Anterior ethmoidal artery
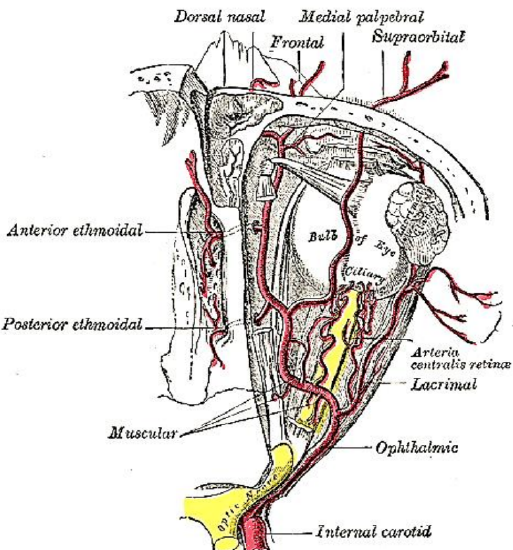
Figure 39: Ophthalmic artery gives rise to anterior and posterior ethmoidal arteries
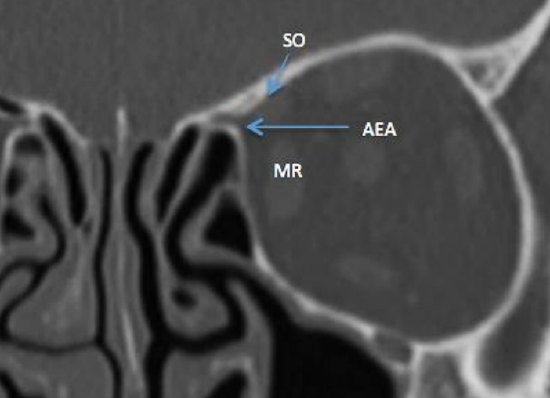
Figure 40: Coronal CT of anterior ethmoidal artery (AEA) as it exits the orbit at anterior ethmoid foramina (between superior oblique (SO) and medial rectus (MR) muscles)
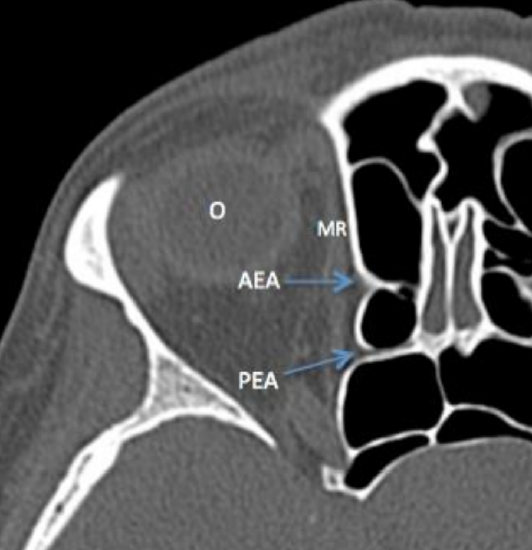
Figure 41: Axial CT shows anterior (AEA) and posterior ethmoidal arteries (PEA), and medial rectus (MR) and orbit (O)
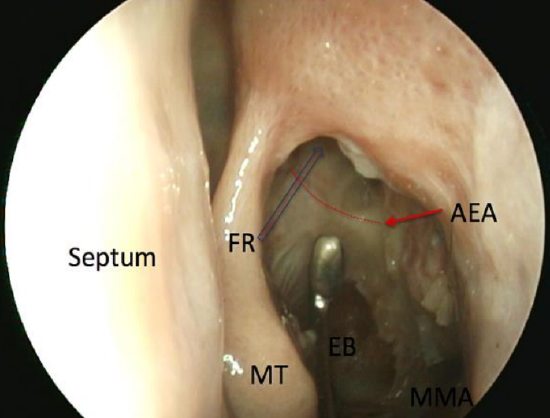
Figure 42: Position of the anterior ethmoidal artery (AEA) with lamina papyracea removed and its relation to the frontal recess (FR) indicated by blue arrow. Middle turbinate (MT), opened ethmoidal bulla (EB), middle meatal antrostomy (MMA)
The anterior ethmoidal artery is a branch of the ophthalmic artery, which is a branch of the internal carotid artery (Figure 39). In the orbit it passes between the medial rectus and superior oblique muscles to exit via the anterior ethmoidal foramen where it forms a “beak” as it traverses the lamina papyracea (Figures 40, 41). It traverses the ethmoid roof obliquely from posterolateral to anteromedial (Figure 42).
Its relation to skull base is important as it may be covered by bone or be suspended in a mesentery up to 5 mm below skull base which puts it at increased risk of injury intraoperatively, especially during anterior ethmoidectomy or during surgery in the frontal recess. It is important to note that its position may vary on each side. Injury to the artery can cause it to retract into the orbit resulting in a rapidly expanding orbital hematoma. This can cause traction on the optic nerve and blindness. It is therefore important to know how to perform a lateral canthotomy and decompression (medial and /or lateral) in the event of injury to the artery to prevent visual impairment.
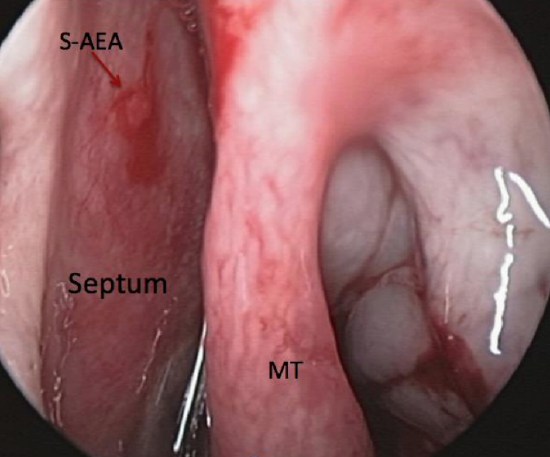
Figure 43: Septal branch of anterior septal artery (S-AEA)
The anterior ethmoidal artery enters the anterior cranial fossa through the lateral lamella of the cribriform after traversing the anterior ethmoids and then turns anteriorly in the anterior ethmoidal sulcus before reentering the nose to supply the superior septum and middle turbinate (Figures 39, 43). The anterior ethmoidal sulcus is the thinnest part of the skull base and is a common site of a CSF leak, both spontaneous and acquired. The septal branch (Figure 39) of anterior ethmoidal artery is a common site of epistaxis and should be carefully looked for in patients presenting with intractable epistaxis. Nasal packing often does not compress this branch of the anterior ethmoidal artery, which lies about 1 cm below the level of the cribriform plate and just posterior to the anterior aspect of the middle turbinate, on the superior septum (Figure 43).
Posterior ethmoidal artery
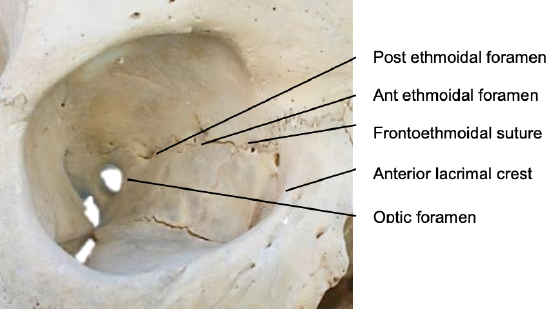
Figure 44: Right medial orbital wall
The posterior ethmoidal artery is also a branch of the ophthalmic artery (Figure 39). It exits the orbit via the posterior ethmoidal canal (Figures 41, 44). The distances between anterior lacrimal crest, the anterior ethmoidal foramen, and the posterior ethmoidal foramen, and the optic canal are approximately 24 mm, 12 mm and 6 mm (Figure 44).
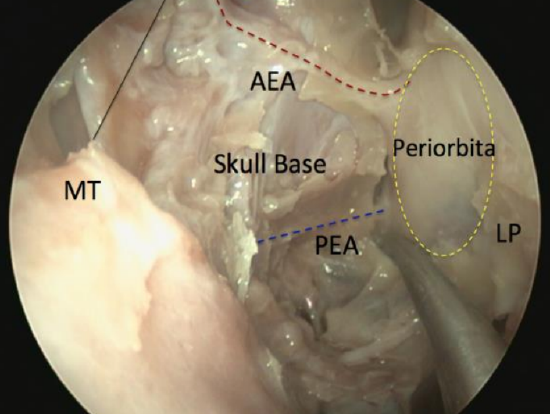
Figure 45: Left anterior (AEA) and posterior ethmoidal arteries (PEA), viewed with a 30° endoscope as they traverse the anterior skull base (skull base, superior attachment of middle turbinate (MT) and lamina papyracea (LP) have been removed)
The posterior ethmoidal artery crosses the anterior skull base anterior to sphenoid face and is usually covered by bone, making it less vulnerable to surgical injury (Figure 45). The artery can often be seen at the junction between skull base (fovea ethmoidalis) and the sphenoid face.
Sphenopalatine artery (Figure 46)
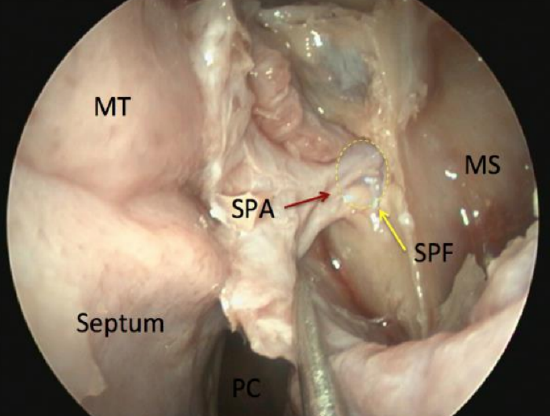
Figure 46: The sphenopalatine artery (SPA) and its branches as they exit the sphenopalatine foramen (SPF) behind the posterior wall of left maxillary sinus (MS)
The sphenopalatine artery is a branch of the internal maxillary artery (IMA), which is a branch of external carotid artery. It accounts for up to 90% of the blood supply to the nasal cavity (lateral nasal wall, turbinates and septum). The IMA runs behind the posterior wall of the maxillary sinus in the pterygopalatine fossa and exits as the sphenopalatine artery via the sphenopalatine foramen, which is formed by the body of the sphenoid posteriorly and the orbital process of palatine bone anteriorly. The sphenopalatine artery may have as many as 10 branches, and these may divide before (40%) or after the sphenopalatine foramen.
The posterior septal branch ofsphenopalatine artery runs across the face of the sphenoid below the sphenoid ostium to supply the posterior septum. The Hadad-Bassagasteguy vascularized nasoseptal pedicled flap is based on this artery. Intranasally, a projection of palatine bone, called the ethmoidal crest, is the most reliable landmark to find the sphenopalatine artery; the artery runs immediately behind this crest.
CT scan: Preoperative checklist
CT scans of the paranasal sinuses are essential before embarking on any form of endoscopic sinus surgery to
- Plan the best surgical approach (endoscopic/open/combined)
- Detect anatomical anomalies
- Assess risks to vital structures
- Assist with diagnosis
- Determine extent of surgery required
CT scans are generally indicated for
- Chronic rhinosinusitis (CRS) that persists despite 6-12 weeks’ medical treatment
- Complicated sinusitis (with contrast)
- Unilateral nasal signs/symptoms
- Suspected tumor (with contrast; consider MRI)
Before embarking on endoscopic ethmoidectomy it is essential to assess the following on the CTs
- Are all sinuses present?
- What is the degree of pneumatization, particularly of the frontal and sphenoid sinuses, and the depth of the maxillary sinuses in younger patients? Well pneumatized sinuses pose a bigger risk to vital structures
- Septum and turbinates; is there a choncha bullosa?...Important for access
- Lamina papyracea intact?
- Ethmoidal air cells: Agger nasi, ethmoidal bulla, suprabullar, supraorbital, Onodi, Haller, Khun cells?
- Basal lamellae: indicate transition between anterior and posterior ethmoids
- Relations of posterior ethmoids to internal carotid artery and sphenoid
- Keros classification
- Anatomy of anterior ethmoid artery
- Sphenoid sinus and surrounds, and relation of septae to internal carotid artery
- Foramina…rotundum, vidian canal
- Outside the sinuses: Internal carotid artery, optic nerve
Ethmoidectomy: Surgical approaches
Ethmoidectomy can be done by external, endoscopic or combined approaches. Readers are referred to the Open Access Atlas chapter on External ethmoidectomy.
External ethmoidectomy is now rarely performed but can be indicated for:
- Complicated sinusitis or acute infection not responding to antibiotics when endoscopic visualization may be severely restricted by bleeding from inflamed mucosa
- Massive facial trauma
- Ligation of anterior and posterior ethmoidal arteries
- Laterally placed mucoceles
- External DCR
- CSF leaks
- Orbital decompression
- Tumors
- Unavailability of endoscopes
Endoscopic Ethmoidectomy
Important considerations when taking consent
- Is a septoplasty indicated for access? This may be difficult to determine preoperatively with Grade 3 polyps
- Is there a possibility that frontal sinus trephination is required (especially if neuronavigation is not available)?
- All risks must be mentioned but address high-risk areas according to the patient’s specific pathology and CT findings; make the patient aware that you will be cautious in these areas
- Is there a risk to the extraocular muscles i.e. superior oblique/ or medial rectus muscle injury causing diplopia?
- CSF leak if working close to skull base
- Meningitis if CSF leak occurs
- Blindness if damage to the optic nerve; inform the patient if work in this area is planned or not
Preoperative optimization
- Anticoagulant medication including aspirin is stopped 5-10 days prior to surgery
- The authors do not routinely prescribe steroids, antibiotics or nasal decongestants
Operating room setup

Figure 47: Positioning the patient: head is in a neutral position with endotracheal tube taped to the left corner of the mouth and the camera stack is positioned directly opposite the surgeon
CT scans must be displayed as they may need to be reviewed during surgery. Because endoscopic sinus surgery causes back, neck and knee strain for surgeons, it is important to position the camera so that it is most ergonomic for the surgeon. Our preference is for the camera stack to be placed opposite to the surgeon, and not at the head of the bed, so that the surgeon operates without having to twist his/her body to view the screen (Figure 47).
Anesthesia
- Surgery is done under general anesthesia
- Secure the endotracheal tube at the left corner of mouth for a right-handed surgeon standing on the right side of the bed
- The endotracheal tube and filter should be out of the way of the endoscope or instruments
- The patient is placed supine, either flat or slightly flexed to 15 degrees, or slightly rotated towards the surgeon
- Lubricate the corneas, close the eyes and cover them with clear adhesive tape; the drapes should not obscure the eyes
- The anesthetist should optimize the surgical field by keeping the patient normotensive with a slow heart rate
- The authors prefer total intravenous anesthesia (TIVA)
- Throat packs are not routinely used, unless significant bleeding is anticipated
- Cefazolin is administered at induction
Surgical equipment

Figure 48: Septoplasty: Killian’s nasal speculum (1), dental syringe and needle (2), Adson tissue forceps (3), 15 blade (4), iris sharp scissors (5), Freer suction elevator (6), Freer elevator (7), Cottle elevator (8), Blakesley forceps (9), gouge (10), straight chisel (11), mallet (12), 0° 4 mm x 18 cm endoscope
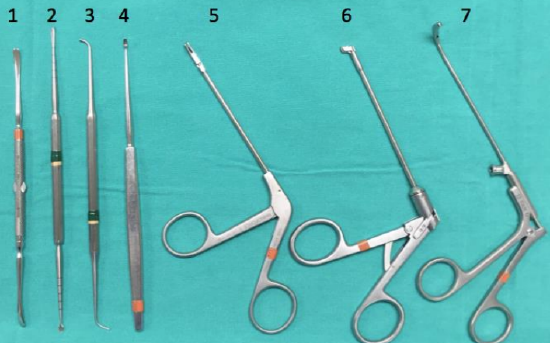
Figure 49: Middle meatal antrostomy, ethmoidectomy: Freer elevator (1), Cottle elevator (2), ball probe (3), straight curette (4), 45° backbiter (5), downbiter (6), maxillary antrum forceps (7)
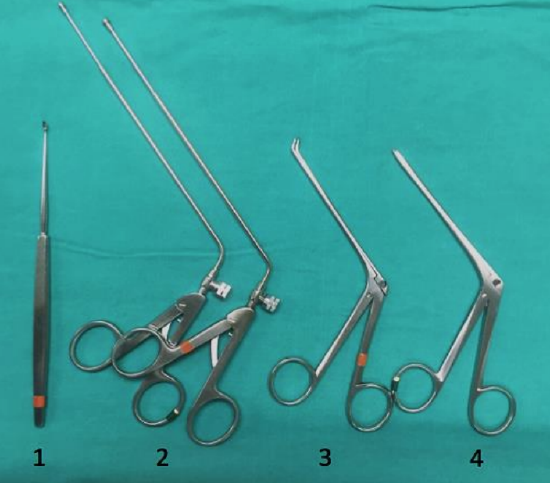
Figure 50: Sphenoidotomy: straight curette (1), mushroom punches (2), 45° Blakesley (3), straight Blakesley (4)
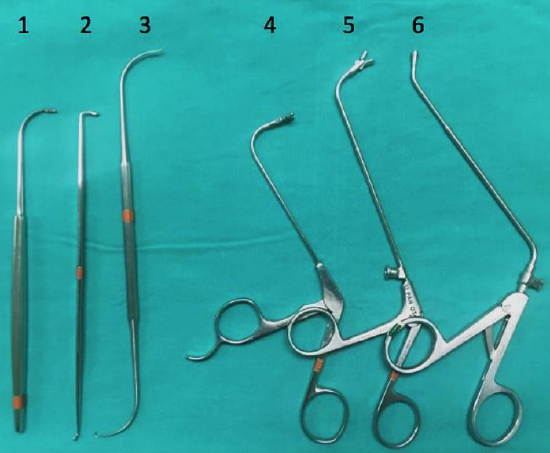
Figure 51: Frontal sinus: frontal sinus curette (1), 90° frontal sinus curette (2), frontal sinus probe (3), frontal sinus giraffe forceps horizontal jaws (4), frontal sinus giraffe forceps vertical jaws (5), frontal sinus mushroom punch (6)
Surgical instruments are illustrated in Figures 48-51. Neuronavigation is not routinely employed but can be helpful in revision surgery and with difficult frontal sinus surgery.
Surgical steps
Preparation & Inspection
- Achieve topical decongestion by inserting ribbon gauze or neurosurgical patties soaked in 2 mL of 1:1000 adrenaline between the inferior turbinate and the nasal septum and in the middle meatus if possible
- Oxymetazoline can be used instead of adrenaline in patients with cardiac disease
- Carefully inspect the nose with the endoscope; this is an essential step before beginning any procedure
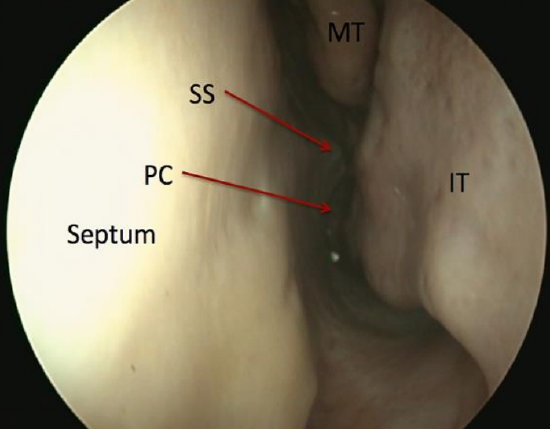
Figure 52: 1st pass along left nasal floor / inferior meatus up to posterior choana (PC); note septal spur (SS), middle turbinate (MT), and inferior turbinate (IT)
- 1st pass: Inferior meatus/nasal floor to postnasal space. Always examine the postnasal space for lesions or adenoidal tissue (Figure 52)

Figure 53: 2nd pass along middle meatus. Middle turbinate and axilla should be visible. Note posterior septal spur (SS) not obstructing access to middle meatus
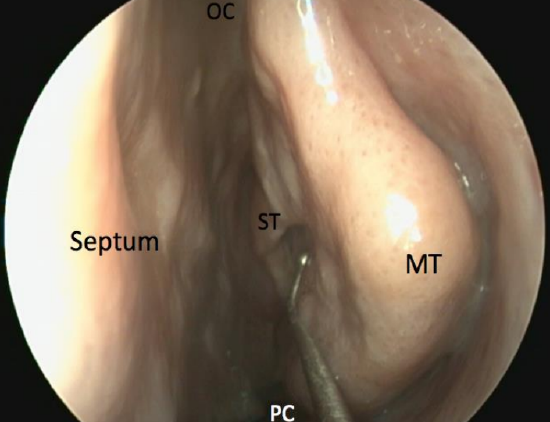
Figure 54: Inspection medial to middle turbinate shows superior turbinate (ST). This is not always possible in live patients, and care must be taken not to manipulate the middle turbinate too vigorously as this might cause a CSF leak. It is important to only mobilise the middle turbinate at its posterior aspect where it is more mobile and not anteriorly. Olfactory cleft (OC)
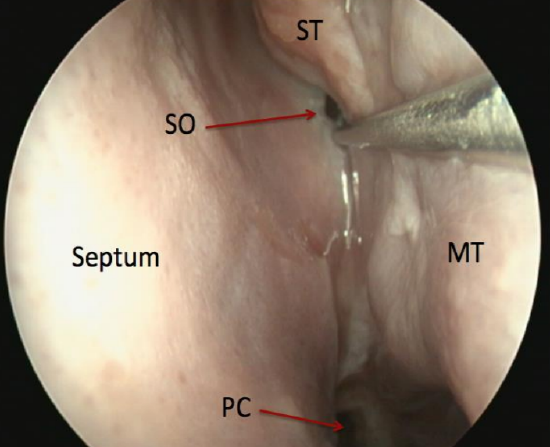
Figure 55: View of the sphenoid sinus ostium (SO) in sphenoethmoidal recess; this ostium is 3 sucker tips above the posterior choana (PC)
- 2nd pass: Middle meatus – retract the endoscope from the posterior nasal cavity into the middle meatus, keeping lateral to the posterior aspect of the middle turbinate; pay careful attention to the inferior and middle turbinates including the axilla of the middle turbinate (conchae, hypertrophy, paradoxical turbinates), the nasal septum (deviation, spurs which may impede surgical access to middle meatus), uncinate process (may be everted) and ethmoidal bulla (most constant landmark) (Figures 53, 54, 55)
- Inject local anesthetic and adrenaline using a dental syringe (Authors use 2% lignocaine/1:80,000 adrenaline preparation) into the nasal septum (if septoplasty required, middle turbinate, axilla of middle turbinate, and inferior turbinate (very slow injection into turbinates). There is a risk of a hypertensive episode if adrenaline is injected too quickly or if too large a volume is injected. This can cause brain hemorrhage, especially in the elderly with vascular problems
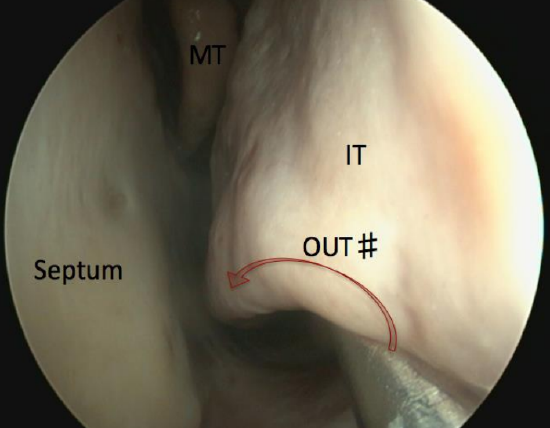
Figure 56: Outfracturing of the inferior turbinate (IT) using a Freer dissector. The instrument is placed under the turbinate and medialized
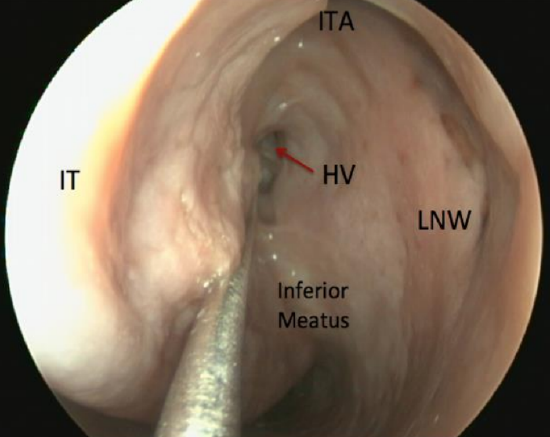
Figure 57: View of Hasner's valve (HV) in inferior meatus. Inferior turbinate axilla (ITA), lateral nasal wall (LNW)
- In- and out-fracture the inferior turbinate to improve access to the uncinate process and middle meatus (Figures 56, 57).
- This is performed with the blunt end or shaft of the Freer dissector to minimize mucosal injury and troublesome bleeding. Insert the instrument under the inferior turbinate and use it to medialize (in-fracture) the turbinate, starting at the axilla and moving posteriorly. The turbinate is then lateralized (outfractured) under direct vision, starting posteriorly and moving anteriorly
Retrograde uncinectomy
- The uncinate process represents the 1st lamella as described by Messerklinger (Figure 23)
- Identify the free posterior edge of the uncinate in front of the ethmoidal bulla
- The uncinate process always lies posterior to the anterior aspect of the middle turbinate
- Do not confuse the uncinate process with the maxillary line (frontal process of maxilla)
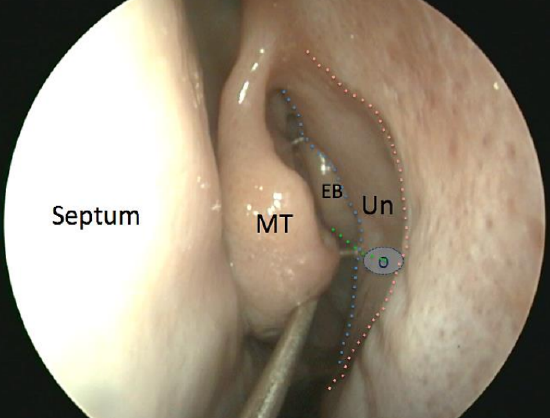
Figure 58: Insert a ball probe behind the free edge of the uncinate process (Un) (blue line). This must not be mistaken for the frontal process of maxilla (red line). The natural ostium of the maxillary sinus (O) lies at the level where the inferior edge ethmoidal bulla (green line) intersects with the free posterior edge of uncinate process (green line).
- Insert a ball probe through the hiatus semilunaris behind this free edge (Figure 58)
- Always insert the ball probe where two lines transect each other – a line at the lower border of the ethmoidal bulla and a line at the inferior aspect of the uncinate (Figure 58)
- Gently elevate the uncinate anteriorly thus creating some space behind it; the ball probe is now in the infundibulum
- Take care not to over-manipulate or over-medialize the middle turbinate, as fracturing the superior attachment of the middle turbinate at the lateral lamella of the cribriform plate may cause a CSF leak
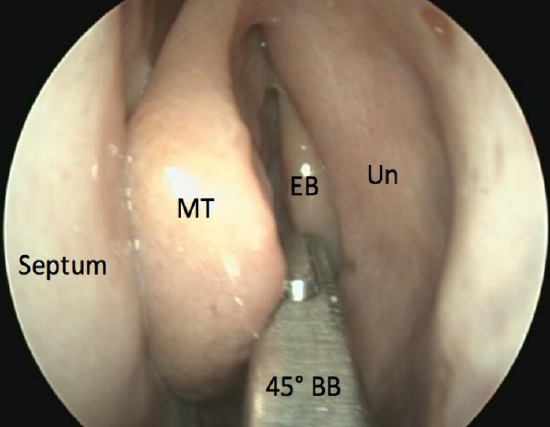
Figure 59: Insert a closed 45° backbiter (BB) up to face of ethmoidal bulla (EB) in middle meatus. Uncinate process (Un)
- Use a 45° backbiter / side-biter to complete the uncinectomy; insert the closed instrument, then open it on the face of the ethmoidal bulla, so that the open blade can be manipulated behind the free edge of the uncinate (Figure 59)
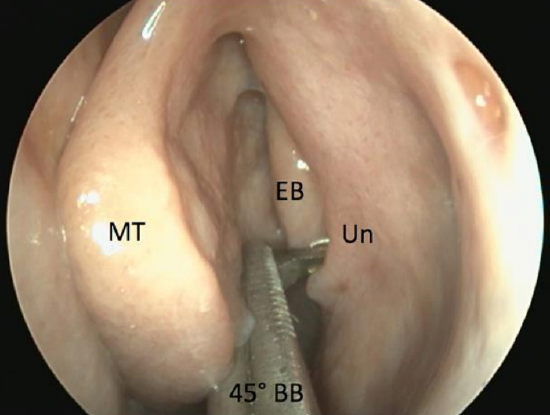
Figure 60: Open 45° backbiter (BB) and insert open blade behind free edge of uncinate process (Un)
- Close the instrument working anteriorly in a safe manner away from lamina papyracea thus minimizing the risk to the eye (Figure 60)
- It is important to resect the uncinate with all 3 its layers (mucosa/bone/ mucosa)
Anterograde Uncinectomy
- Uncinectomy can also be performed anterogradely with a sickle knife or Freer dissector
- Identify the anterior attachment of the uncinate
- Make an incision with a sickle knife or Freer dissector to release it from its anterior attachment to the lacrimal bone
- All 3 layers must once again be incised (mucosa/bone/mucosa)
- Remove the uncinate with a through cutting instrument
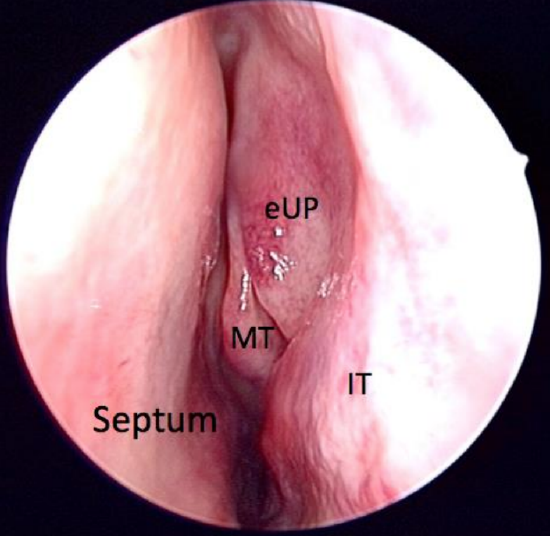
Figure 61: Everted uninate process (eUP)
- The anterograde technique carries a greater risk of injury to the lamina papyracea and the eye, but may be necessary with a very everted uncinate when it is not possible to get an instrument behind its free edge (Figure 61)
Middle meatal antrostomy
- Proceed to middle meatal antrostomy
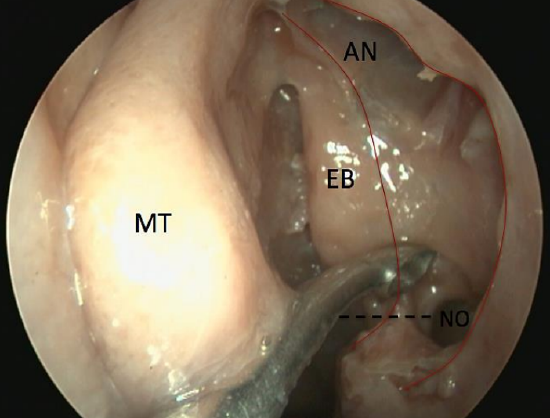
Figure 62: Identifying the maxillary sinus natural ostium (NO). Uncinate process has been removed (red lines). Agger nasi (AN), ethmoidal bulla (EB). Black dashed line shows how the natural maxillary ostium is at the same level as where ethmoidal bulla intersects with free edge of uncinate process (inferiorly)
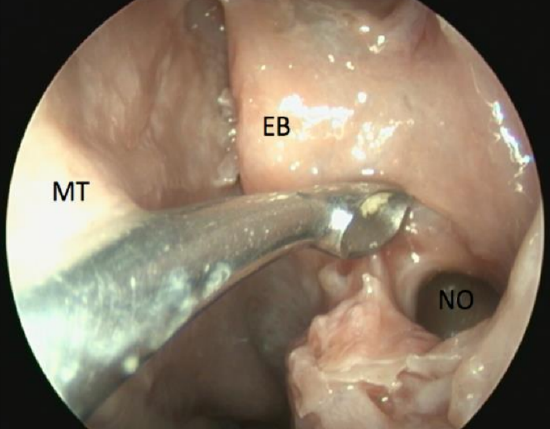
Figure 63: Close-up view of natural ostium of maxillary sinus (NO), ethmoidal bulla (EB)
- Identify the natural maxillary ostium at the same level as the inferior edge of the middle turbinate (Figures 62, 63)
- Insert a curved ball probe into the maxillary antrum via its natural ostium
- Widen the opening of the natural ostium posteriorly and inferiorly by removing mucosa with through cutting or back/ side biting instruments
- If accessory ostia have previously been identified, then these ostia should be interconnected to avoid a subsequent recirculation phenomenon
- The size of the maxillary sinusotomy depends on the disease process. For severe nasal polyposis a large (type III) middle meatal antrostomy is required. For minimal disease, an infundibulotomy (uncinate window) may be all that is required
- Take a pus swab from the maxillary sinus
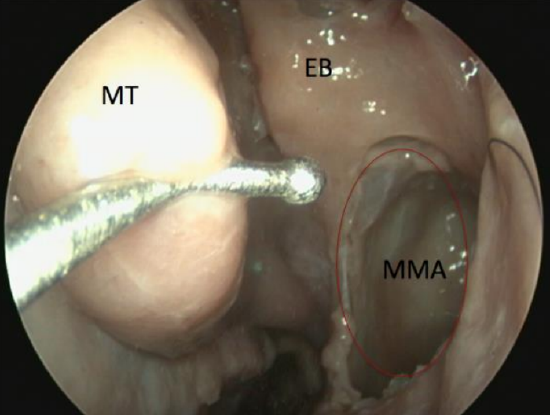
Figure 64: Type III middle meatal antrostomy (MMA)
- Simmens classifies maxillary sinusotomy as follows:
- Infundibulotomy (uncinectomy): Removal of uncinate process, preserving the mucosa of the natural maxillary ostium. The superior attachment of the uncinate can be left intact, particularly if attached to the skull base or middle turbinate to avoid potential complications e.g. adhesions around the frontal recess and CSF leaks
- Type I maxillary sinusotomy: Enlarging the natural maxillary ostium posteriorly by <1 cm. If an accessory ostium is present, this should be combined with the natural ostium to avoid a recirculation phenomenon
- Type II maxillary sinusotomy: Antrostomy is opened 2 cm posteriorly and inferiorly
- Type III maxillary sinusotomy (Figure 64): Antrostomy is opened up to posterior wall of maxillary antrum, anteriorly to the lacrimal sac and inferiorly to the base of the inferior turbinate
Anterior ethmoidectomy
- The lateral attachment of the ethmoidal bulla represents the 2nd lamella as described by Messerklinger (Figure 23)
- The straight curette and 45° Blakesley are the most important instruments for ethmoidectomy; the curette is used to break the bony lamellae and the 45° Blakesley is used to remove the cells
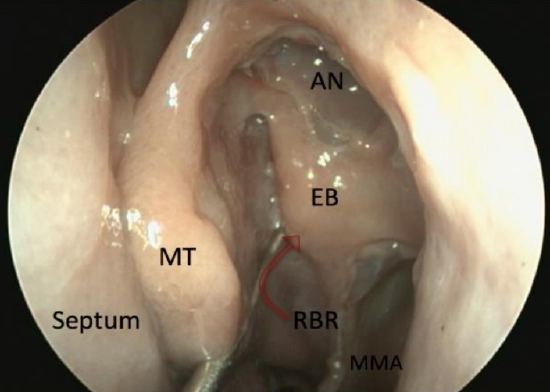
Figure 65: Retrobullar recess (RBR) is between ethmoidal bulla (EB) and middle turbinate (MT) basal lamella. It is not always present
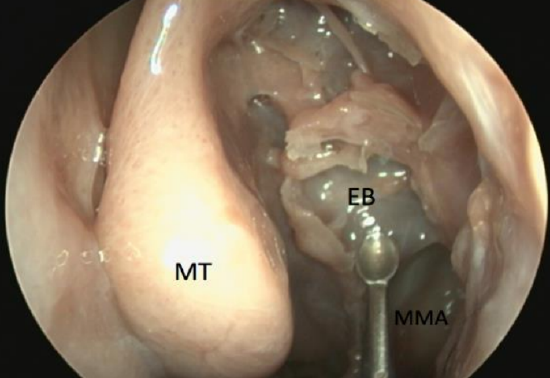
Figure 66: Face of ethmoidal bulla (EB) removed
- First open the bulla ethmoidalis by placing a straight curette behind the ethmoidal bulla into the retrobullar recess or into the bulla from below and breaking the bulla down by moving the instrument towards yourself (Figures 65, 66)
- Other anterior ethmoidal air cells are similarly opened
- Once the cell walls are fractured, remove them with a 45° Blakesley (Figure 50)
- Loose tissue can be removed by grasping and rotating medially
- Remember never to pull on any tissue;
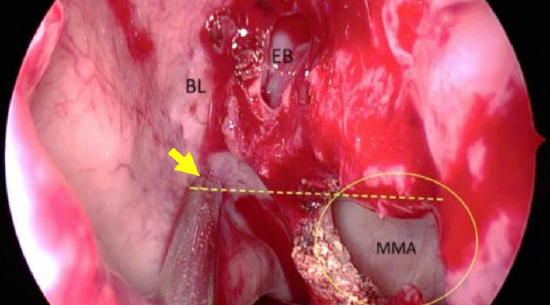
Figure 67a: Close-up view of middle meatus after middle meatal antrostomy (MMA) showing basal lamella (BL) of middle turbinate, ethmoidal bulla (EB) face removed. The suction tip (yellow arrow) indicates level at which basal lamella is to be perforated
- The basal lamella of the middle turbinate now comes into view (Figure 67a)
Basal/ground lamella
- The lateral insertion of the middle turbinate to the lamina papyracea is called the basal lamella. It is posterior to the bulla ethmoidalis and separates the anterior from posterior ethmoid air cells, and represents the 3rd lamella as described by Messerklinger (Figure 23)
- Open the basal lamella at the level of the superior aspect of the maxillary sinus ostium, pointing the sucker medially towards the septum. This will be in line with the sphenoid ostium (Figures 67a)
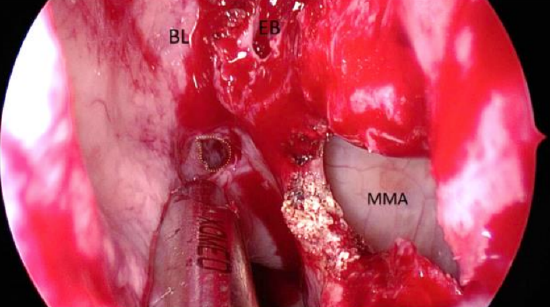
Figure 67b: Perforating the basal lamella (BL) of middle turbinate. This initial perforation is subsequently enlarged using a shaver or Kerrison punch
- Use a thin straight sucker to break through the basal lamella to enter the posterior ethmoidal cells (Figures 67b)
- Pass a straight curette through this opening in the basal lamella and enlarge the opening, first superiorly, and then laterally towards the lamina papyracea
- Remove the medial aspect of the basal lamella with a sphenoid or Kerrison punch
- Be careful not to pull on this area as the middle turbinate may be avulsed or fractured during this part of the procedure
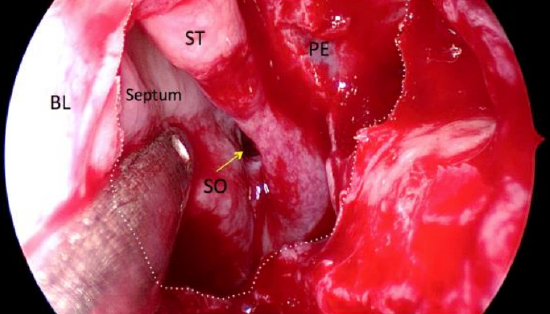
Figure 68: Dashed line indicates opening of basal lamella (BL) of middle turbinate. Entire edge of superior turbinate (ST), sphenoid ostium (SO) and posterior ethmoidal air cell (PE) are now visible
- Open the basal lamella until the entire free edge of the superior turbinate is visible (Figure 68)
Posterior ethmoidectomy
- Proceed to posterior ethmoidectomy in a similar anterior-to-posterior stepwise fashion, working up to the sphenoid face and skull base
- To identify these structures, it is often good to first locate the sphenoid ostium
- This is done after medially breaking through the basal lamella of the middle turbinate (Figure 68)
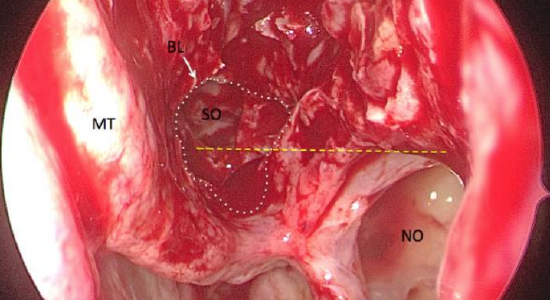
Figures 69: The sphenoid ostium can be located by perforating the basal lamella of the middle turbinate (BL). The window in the basal lamella is demonstrated by dashed line. The inferior margin of sphenoid ostium (SO) is at the same level as the superior margin of maxillary sinus natural ostium (NO) demonstrated by yellow dashed line.
- The inferior border of the sphenoid ostium is seen at a level approximately horizontal to the superior border of the maxillary ostium, medial to superior turbinate (Figure 69)
- Once the ostium has been identified, you know where the sphenoid face is; this represents the posterior limit of the ethmoidectomy dissection
Onodi cell
- Horizontal septations seen on CT within the sphenoid sinus represent an Onodi cell
- An Onodi cell is associated with an increased risk of optic nerve injury (15% dehiscent in Onodi cell) as it is often closely related to the optic nerve and care needs to be taken not to injure the optic nerve within this cell. It is also associated with carotid artery (20% dehiscent in Onodi cell) or brain injury
Completing the ethmoidectomy
- Once the sphenoid ostium has been identified, the posterior and superior limits of the dissection can easily be determined
- The authors now break through the lamella of the superior turbinate (preserving the superior turbinate) using a small straight sucker and 1 mm 45-degree Kerrison punch so that the sphenoid ostium can be directly visualized from the middle meatus via the ethmoidectomy
- Use a straight curette to break down the posterior ethmoidal cells, working from posteriorly to anteriorly and away from the skull base
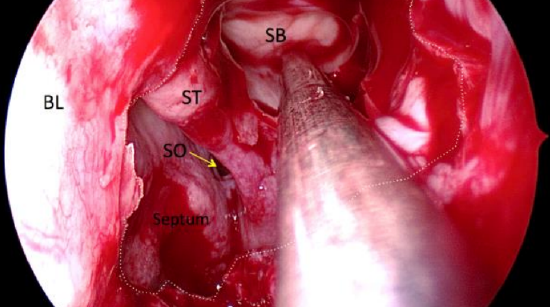
Figure 70: Fovea ethmoidalis (skull base) now clearly visible
- The fovea ethmoidalis (skull base) can now be clearly seen (Figure 70)
Frontal recess and frontal sinus drainage pathway
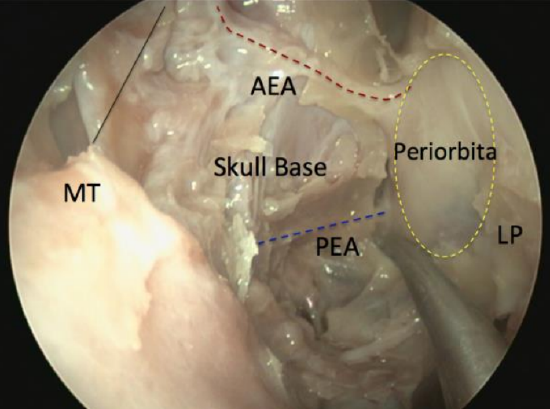
Figure 71: Anterior (AEA) and posterior ethmoidal arteries (PEA), viewed by 30° endoscope as they traverse anterior skull base (skull base, superior attachment of middle turbinate (MT) and lamina papyracea (LP) all removed)
- Continue the dissection from posterior-to-anterior with the skull base kept in full view during the dissection (Figure 71)
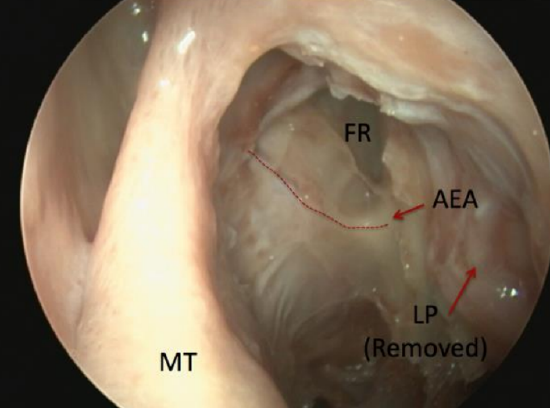
Figure 72: The anterior ethmoidal artery (AEA) is closely associated with the posterior boundary of the frontal recess (FR). It runs from posterolateral to anteromedial on the skull base (above) or occasionally in a mesentry below skull base which is more vulnerable to injury
- Once the frontal recess area is reached, care needs to be taken to avoid injury to the anterior ethmoidal artery (Figure 72)
- It is the authors’ preference to first identify the frontal sinus drainage pathway before removing the remaining cells around the area of the anterior ethmoidal artery or posterior aspect of the frontal recess
- These cells are left undisturbed until last as the highest risk of an anterior ethmoidal artery bleed and CSF leak is during this part of the procedure
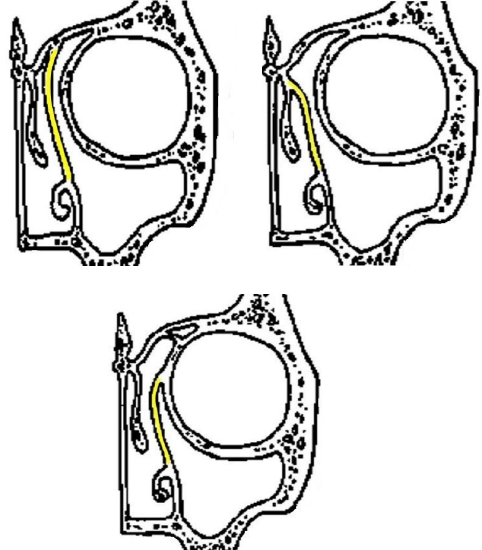
Figure 73: Frontal sinus drainage pathway is determined by insertion of the uncinate process to the: roof of ethmoid centrally; middle turbinate; and lamina papyracea laterally
- Review the frontal sinus drainage pathway on the CT scan; it is important to examine the insertion of the uncinate process and the anatomy of the agger nasi cell and bulla ethmoidalis to determine the frontal sinus drainage pathway (Figure 73)
- A ball probe can usually be carefully inserted into the drainage pathway
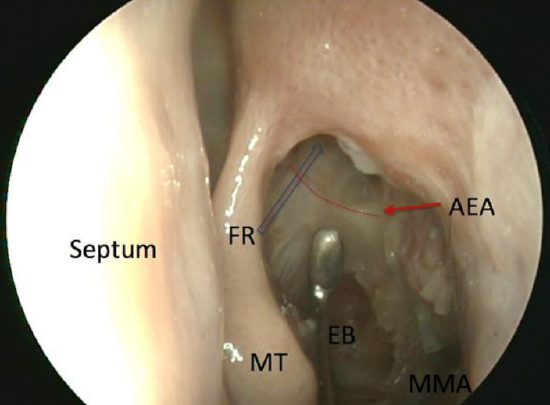
Figure 74: Anterior ethmoidal artery (AEA) with lamina papyracea (LP) removed. Frontal recess (FR) indicated by blue arrow
- Once the frontal sinus has been entered and the posterior border of the frontal sinus has been identified, the remaining cells around the anterior ethmoidal artery can be safely removed (Figure 74)
Nasal Packing
- Packing may be used to control bleeding, prevent adhesions or provide compression to avoid a septal hematoma if septoplasty has been done
- The authors commonly use topical hemostatic powder (Nexstat®) for hemostasis and to avoid packing
- If the middle turbinate needs to be medialized to prevent adhesions, dissolvable packing such as Nasopore is favored as a temporary spacer
Postoperative in hospital care
- Regular analgesia
- Pulse, blood pressure and Glasgow coma scale are carefully monitored
- Observe for epistaxis, headaches, orbital swelling, diplopia, reduced visual acuity and clear rhinorrhea
- Remove nasal packs the following day
Postoperative ambulatory care
- Antibiotics are not routinely prescribed
- Instruct patient not to blow the nose hard for at least 48 hours and only gently thereafter
- Day 1: Commence topical decongestants for 5 days and a saline spray or douche for 6 weeks
- Day 2: Check intraoperative pus swab results; if a specific organism has been isolated, prescribe appropriate antibiotics
- Day 4: Suction-toilet the nose, check for septal hematoma or infection
- 1 week: Recommence long-term nasal steroids with nasal polyposis
- 6 weeks: Decrust the nose with a rigid endoscope in the clinic if necessary
Pearls and Pitfalls
Excessive intraoperative bleeding
- Pack with adrenaline or oxymetazoline soaked gauze
- Work on the opposite side of the nose and return to complete surgery once hemostasis has been achieved
- Sphenopalatine artery ligation may be required
- Staged surgery is often better to reduce the risk of serious complications; therefore abandon surgery if there is uncontrollable bleeding or poor visibility
Frontal sinus surgery
- Surgery to the frontal sinus is often easier to perform once infection and inflammation have settled
Anterior ethmoidal artery injury
- Preoperative CT evaluation of the location of the ethmoidal arteries relative to the skull base is essential
- Injury to the anterior or posterior ethmoidal arteries causes them to retract into the orbit and cause an orbital hematoma
- Proptosis and orbital hematoma increases intraocular pressure causing blindness
- Intraoperative signs: Orbital hematoma, proptosis, periorbital swelling
- Therefore, it is essential that eyes remain visible during surgery through a clear adhesive dressing
- Attempt to control bleeding in the nose with bipolar cautery
- Never use monopolar cautery due to the risk of blowing a hole in the thin bone of the skull base and causing a CSF leak
- Orbital hematoma and proptosis either intra- or postoperatively requires urgent lateral canthotomy
- As lateral canthotomy is only a temporary solution and should be followed by a full medial orbital decompression
Breach of lamina papyracea
- Generally, has no consequences if it is recognized
- Be aware of possible risk of injury to the periorbita
- Does not required repair
- Avoid blowing nose for 10 days as at risk of pneumo-orbit
Exposed orbital fat
- Medial rectus muscle is at risk
- Stop surgery for a moment, and carefully assess the area
- Confirm that it is fat by placing tissue in normal saline or water; if it floats, it is fat
- If comfortable with the situation, then proceed with the surgery
- Avoid the microdebrider in this area
- No repair required
- Avoid blowing nose for 10 days as at risk of pneumo-orbit
Diplopia due to medial rectus injury
- Urgently consult an ophthalmologist
- Medial rectus injury causes diplopia
- Cannot easily be corrected
- Is a life altering complication and hard to legally defend
CSF leak
- If noticed intraoperatively, repair immediately
- Depending on the location of the leak, this can be done with bipolar cautery, local mucosal flaps, facial underlay grafts and/or Duraseal
- Lumbar drains not indicated
How to prepare and administer a saline douche
Nasal irrigation is a safe and natural way to help wash crusts and mucus from the nose. Although there are many over-the-counter saline solutions, patients can make their own:
Saline solution
- ¼ teaspoon of bicarbonate (baking) soda
- ¼ teaspoon of salt (non-iodised)
- 1 cup of boiled then cooled water
Method
- Fill a large syringe (10 or 20 mL) or a sinus rinse bottle (available from many pharmacies) with the saline solution
- Stand over a basin
- Keep the head straight
- Put the nozzle towards the back of the nose
- Squirt into one nostril and then repeat on the other side Or
- Pour some of the solution into the palm of the hand and sniff it into each nostril
- The mixture should run into the mouth – spit this out
- Swallowing the solution is harmless
- Repeat two times per day
- If a medicated nasal spray has been prescribed, the douching solution should be used before using the nasal
Authors
Pedro Monteiro MBBCh, MMed, FCORL
University of Cape Town
Karl Storz Rhinology Fellow
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
mail@pmonterio.com
Darlene Lubbe MBChB, FCORL
Associate Professor
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
doclubbe@gmail.com
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


