5.9: Radial Free Forearm Flap (RFFF)- Surgical technique
- Page ID
- 52961
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
RADIAL FREE FOREARM FLAP (RFFF): SURGICAL TECHNIQUE
Ottie van Zyl
The radial free forearm flap (RFFF) was one of the first free tissue transfer flaps to be described. It has since become a workhorse for soft tissue replacement in head and neck cancer surgery, being commonly used to replace external skin and internal mucosal linings. It is an extremely versatile flap allowing intricate folding of the skin, using two or more skin paddles/ islands, and incorporating vascularized tendon and/or bone (osteocutaneous flap).
Common reconstructive applications
- Floor of mouth, tongue, soft and hard palate, buccal mucosa, pharynx and esophagus
- Lips
- Orbit
- External skin defects
- Incorporating part of radius as osteocutaneous flap for premaxillary, maxillary, nasal, and selected mandibular defects
- Incorporating palmaris longus tendon sling to support lower lip reconstruction
Advantages
- Very pliable, thin skin, especially at distal forearm (one of thinnest skin flaps)
- Usually very little soft tissue bulk
- Large flap may be harvested (30 x 15 cm)
- Multiple skin islands can be used
- Sensory innervation possible
- Can incorporate radius bone or tendon
- Easy flap elevation
- Large, reliable, constant vessels
- Long pedicle usually available
- Distant location of donor site from head and neck resection permits simultaneous harvesting and resection
- Large distal size of vessel allows it to be used as a "flow-through-flap" for an additional flap to be attached distally
Caveats
- Potentially poor skin quality: in certain individuals the flap may be quite bulky, especially proximally; this can compromise certain reconstructions
- Donor site morbidity: loss of skin graft and tendon exposure; visible donor site and possible poor cosmetic result
- Vascular: atherosclerosis (seldomly); postoperative vascular compromise of hand (rarely)
Surgical anatomy of volar forearm
The skin of the volar (anterior) surface of the forearm is usually thin and pliable, especially the distal half. It is however unfortunately hair-bearing skin, especially on the proximal and lateral sides of the forearm; consequently, one might have hair growth e.g. in the oral cavity. The subcutaneous fat is thin, especially over the distal third of the forearm. However, overweight patients and even some normal individuals may have a disproportionate amount of fat in this distal area.
Venous system
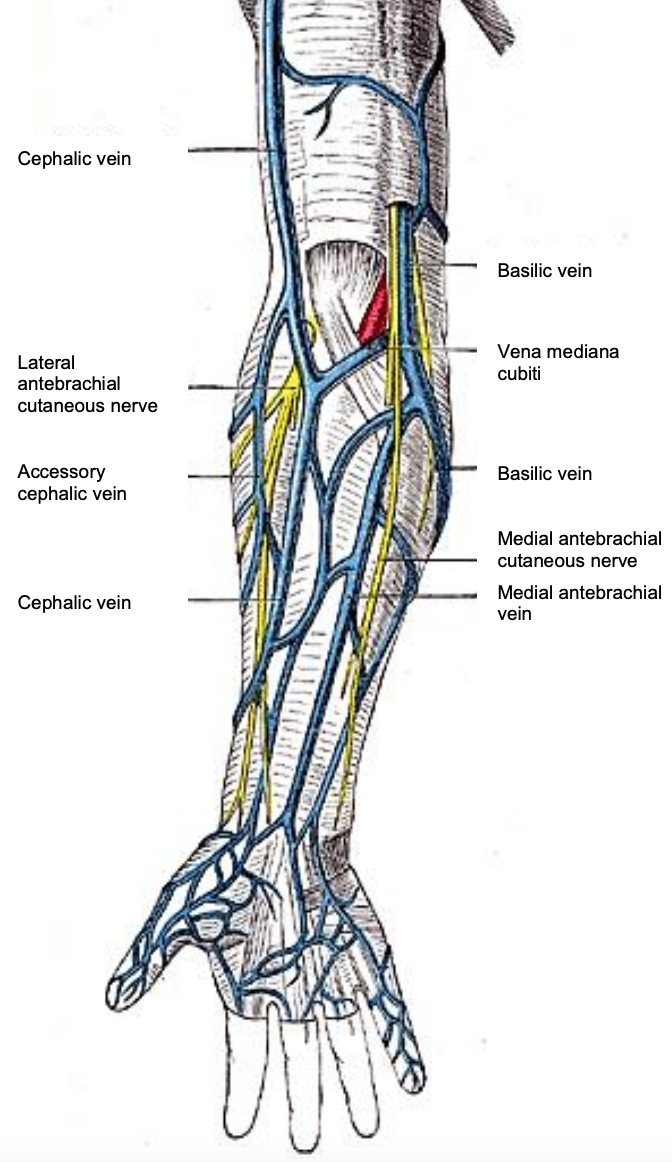
Figure 1: Volar surface of right forearm demonstrating cephalic and basilic venous systems, the median antebrachial vein of the forearm and the associated nerves
In the subcutaneous tissues lie the small venous tributaries of the main superficial venous drainage system of the forearm, i.e. the cephalic and basilic veins, which lie deep to the fatty layer (Figure 1).
The cephalic vein is the most commonly used single vein for venous drainage of RFFFs (Figure 1). It is a large, thick-walled vein and is found in a relatively constant location deep beneath the subcutaneous fat. Unfortunately, due to its size and superficial position, it is also very often used for intravenous lines, which may cause fibrosis and/or thrombosis of the vessel. It drains the anterolateral forearm and is formed mainly by the confluence of superficial veins on the dorsal aspect of the hand (Figure 1). From there the vein, or its tributaries, traverses the lateral "snuffbox" area to lie over the lateral side of the distal forearm. It gradually courses more medially towards the mid-lateral cubital fossa. It is accompanied by the lateral antebrachial nerve (Figure 1). The superficial branch of the radial nerve lies in close proximity to the vein in the distal third of the lateral forearm and over the "snuffbox” area up to the lateral aspect of the dorsum of the hand.
The basilic vein runs towards the lateral cubital fossa along the medial side of the forearm and is located deep beneath the subcutaneous fat.
The median (antebrachial) vein of the forearm lies between the cephalic and basilic veins. Occasionally it may be large and be a better drainage system to use for a flap (Figure 1). It is usually thin-walled and is situated more superficially in the subcutaneous fat than the cephalic and basilic veins.
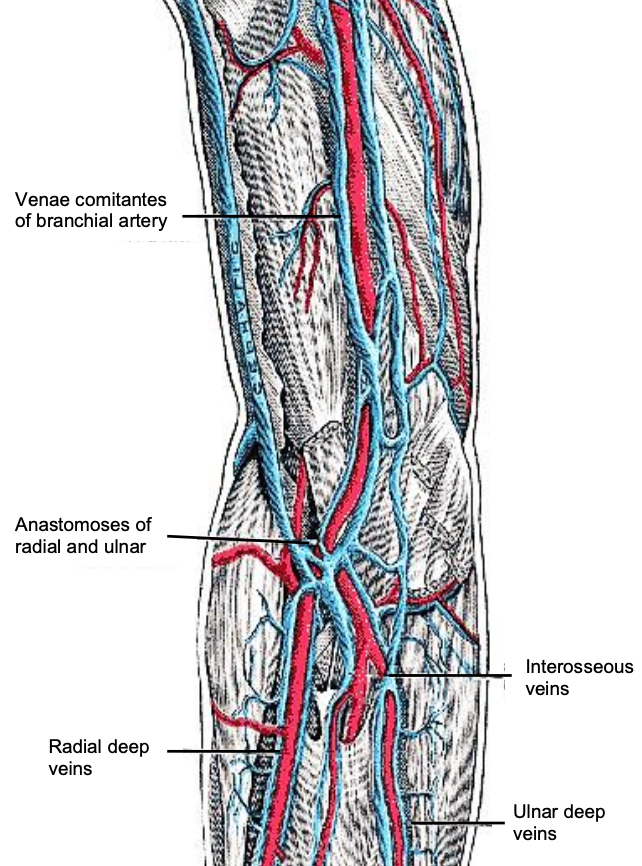
Figure 2: Venous anatomy at right cubital fossa
A great variety of venous interconnections may be encountered in the cubital fossa. The median cubital vein (vena mediana cubiti) runs obliquely from lateral to medial to connect the cephalic and basilic systems (Figures 1, 2). There is often an important connection between the superficial veins and the deep brachial venous system in the cubital fossa; this is usually between the brachial venae comitantes and the median cubital vein or the cephalic vein.
The forearm and cubital fossa are invested by the deep fascia; in the cubital fossa it is strengthened by the bicipital aponeurosis (Figure 1). The perforating vein connecting the superficial and deep venous systems lies lateral to the bicipital aponeurosis and the brachial vessels immediately deep to it (Figure 1).
Nerves
The superficial nerves accompany the superficial veins (Figure 1). The lateral antebrachial nerve (Figure 1) is the termination of the musculocutaneous nerve which, after supplying the flexors of the upper arm, pierces the deep fascia just proximal to the cubital fossa. The anterior branch of the antebrachial nerve then accompanies the cephalic vein distally (Figure 1) and supplies sensation to the anterolateral forearm, (which is also the main area of a distal RFFF). The posterior branch supplies sensation to the posterolateral forearm.
The medial antebrachial nerve runs with the basilic vein; they pierce the deep fascia in the medial part of the mid-upper arm. It too, has an anterior branch supplying sensation to the anteromedial forearm and a posterior branch to the posteromedial forearm.
Deeper nerves include the median, ulnar nerves. These are usually not at risk when elevating the flap. The median nerve lies between the flexor carpi radialis and palmaris longus tendons. The palmar cutaneous branch of the median nerve arises just above the flexor retinaculum at the wrist and becomes cutaneous between the tendons of palmaris longus and flexor carpi radialis. Elevation of a very distal skin flap may injure the latter branch and cause sensory loss of the proximal midpalm.
Muscles
The muscles of the forearm will be described according to their relationships to the radial artery.
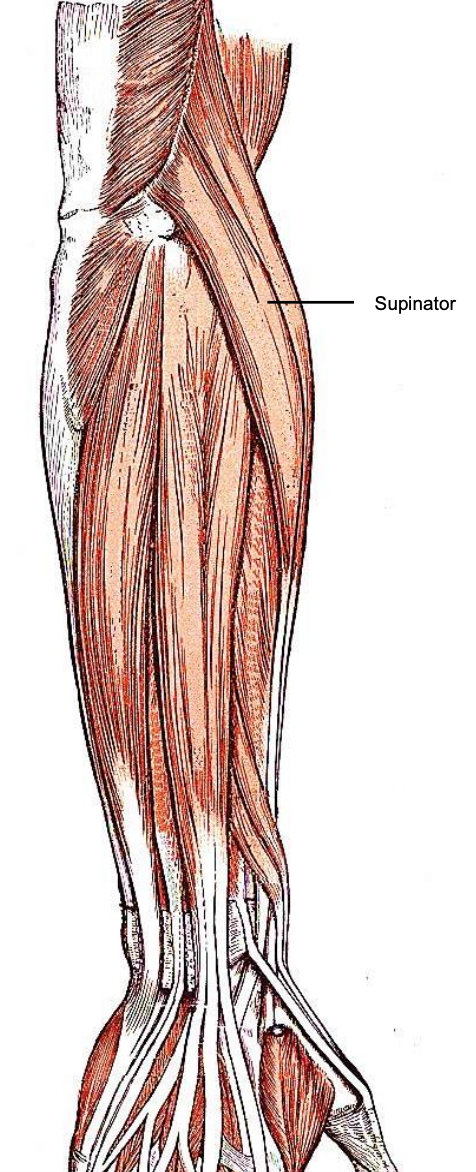
Figure 3: Dorsal view of right forearm demonstrating the supinator muscle

Figure 4: Volar view of right forearm: a: biceps brachii; b: brachioradialis; c: biceps brachii tendon d: pronator teres; e: flexor carpi radialis; f: palmaris longus; g: flexor carpi ulnaris; flexor digitorum longus
Where the radial artery enters the forearm it lies superficial to the supinator (Figure 3), pronator teres and flexor digitorum superficialis (FDS) muscles in the proximal third of the forearm, and superficial to the flexor pollicis longus (FPL) and pronator quadratus muscles in the distal third (Figure 4).
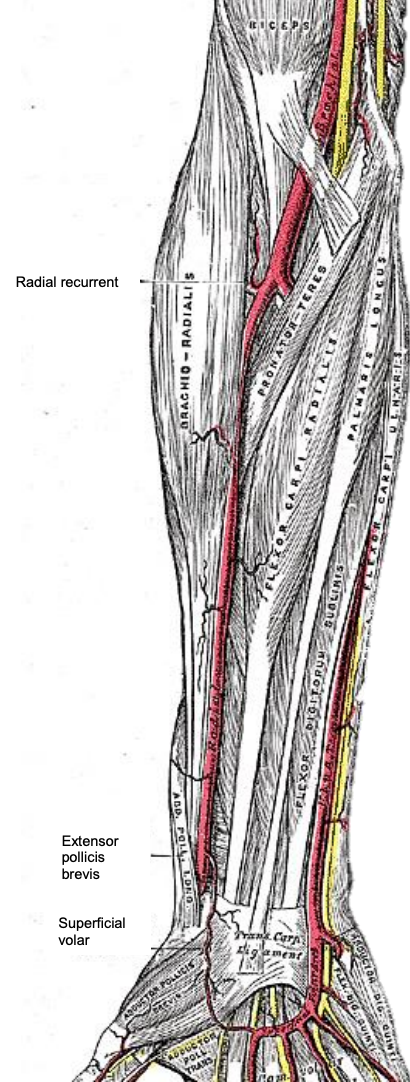
Figure 5: Volar view of right forearm demonstrating course of radial artery relative to brachioradialis, pronator teres and flexor carpi radialis muscles
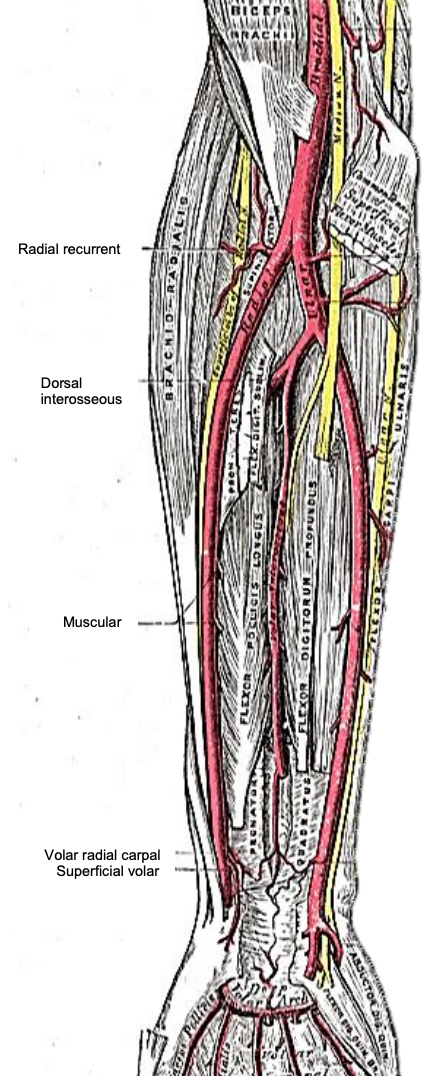
Figure 6: Volar view of right forearm demonstrating course of radial artery with brachioradialis muscle reflected
The radial artery runs in the lateral intermuscular septum which separates the flexor and extensor compartments of the forearm. Medially are the flexor carpi radialis (FCR) and the other forearm flexor muscles (Figures 5, 6). Laterally is the extensor compartment.
The key muscle when elevating a RFFF is the brachioradialis muscle and its tendon (Figures 4, 5, 6). The muscle overlies the anterolateral side of the artery (Figures 5, 6). It is supplied by the radial nerve of the extensor compartment, even though it is an elbow flexor. This bulky muscle belly lies anterior to, and covers, the radial artery in the proximal half of the forearm (Figure 5). In the distal forearm the muscle be-comes a flat tendon. It is important to know that the tendon commonly covers the artery either partially or completely. The significance of this will become apparent during flap elevation and protection of the perforators. At the wrist the radial artery lies between the brachioradialis and flexi carpi radialis tendons (Figure 5).
The palmaris longus tendon (Figures 4, 5) can be sacrificed without causing a functional deficit. It is absent in ca. 13% of individuals. Its tendon and muscle can be incorporated in a forearm flap for various reconstructive possibilities and it may therefore be an extremely valuable adjunct in complex reconstructions.
Radial artery and its branches
The brachial artery bifurcates into ulnar and radial arteries (Figures 5, 6). The radial artery starts in the medial cubital fossa, 1 cm distal to the elbow crease, just medial to the biceps tendon (Figures 5, 6). It then courses down the forearm in the lateral intermuscular septum which separates the flexor and extensor compartments of the forearm to the (palpable) radial pulse, just medial to the tip of the styloid process of the radius. Branches in the forearm include the radial recurrent artery close to its origin (Figures 5, 6); and distally, the palmar carpal branch (Figure 6), the superficial palmar branch and the continuation of the artery, the dorsal carpal branch. Along its course in the forearm it gives off muscular branches (Figures 5, 6).
A variable number (average 12) of septocutaneous perforators exit the artery to supply the overlying fascia and skin. The greatest number of perforators is found in the distally third of the forearm, approximately 12-20 cm from the origin of the radial artery. A major perforator is located 0-2 cm proximal to the radial styloid process; and a cluster of perforators is located in the distal 1/5 of the forearm with another cluster in the proximal forearm1.
Periosteal blood supply to the distal radius is via branches to the deep flexor pollicis longus and pronator quadratus muscles; perforators also pass through the lateral intermuscular septum from the radial artery to the periosteum.
Radius bone (Figure 7)

Figure 7: Volar view of right radius bone
The distal 10-12 cm of the anterolateral radius can be harvested as an osteocutaneous RFFF. Knowledge of the anatomy of the shaft and its distal end are important when raising an osteocutaneous flap. The shaft increases in size from proximal to distal and bows laterally. The medial side of the shaft has a sharp interosseous border at the attachment of the interosseous membrane. The wide distal end tapers into the pyramidal styloid process.
Evaluation of vascular status
Harvesting the radial artery is associated with a remote possibility of vascular compromise causing claudication of the hand. The surgeon should confirm the presence of a radial arterial pulse. Enquire about the patient’s occupation or leisure activities e.g. a pianist may be concerned about claudication.
Modified Allen Test: This is used to assess the adequacy of the ulnar artery and crossflow through the palmar vascular arches of the hand
- Ask the patient to elevate the arm and to make a tight fist
- Occlude the radial and ulnar arteries for a few seconds by digital pressure
- Ask the patient to release the hand into a relaxed, slightly flexed position
- Check whether the palm and fingers have blanched; if not, then occlusion of the vessels is inadequate, and the test is repeated
- Release pressure from the ulnar artery
- With a positive Allen Test the hand flushes and the color changes from pallor to rubor within 5-15 seconds; it can be concluded that there is good crossflow from the ulnar artery
- With a negative Allen Test the circulation is considered inadequate and it is a relative contraindication to proceeding with a RFFF
- Even though there is controversy about the reliability of the Modified Allen Test, the author routinely does the test; in equivocal cases when there is some delay in the "flush", he has always continued with the RFFF and has never encountered symptomatic vascular compromise or ischemia in more than 700 RFFFs
Choice of arm
It is not as critical as with free fibular flaps what side to use. Although it is preferable to have the operating arm table on the contralateral side to the resection to create enough space for two surgical teams to work simultaneously, it is not that difficult to work on the same side of the patient. Previous intravenous lines, surgery, injury, scars, skin deformities, fractures or vascular compromise may necessitate one to use a specific arm. The patient's preference is also taken into account.
Preoperative counseling
Patients are properly counseled about the outcomes following flap harvest, particularly visibility of the scar or skin graft, a (possibly) poor cosmetic result, the possibility of hypertrophic scarring and using a prophylactic pressure garment to avoid it; delayed wound healing and possible loss of a skin graft. Mention should also be made of possible temporary or permanent variable sensory loss over the radial thenar region, the metacarpal region of the dorsum of the thumb or less commonly, of the dorsal hand; as well as claudication.
Operating room setup

Figure 8: Two-team setup: RFFF being harvested (foreground); head & neck resection (background); anesthetics (right)
- Resect the primary tumor and elevate the RFFF simultaneously as a 2-team approach to minimize the length of surgery (Figure 8)
- • Create working space around the head and torso by placing anesthetic and other equipment at the foot of the bed with extensions for intravenous lines and anesthetic tubes (Figure 8)
- Two bipolar and monopolar electrocautery systems are required
- Place the arm on an arm table
- Avoid hyperextending or hyperabducting the shoulder
- Shave the forearm
- Apply a tourniquet to the upper arm
- Adjust the operating table and/or the chairs so that the reconstructive surgeon and assistant are seated
Surface markings for RFFF
- Palpate and mark the radial artery at the wrist between the brachioradialis and flexor carpi radialis tendons
- Palpate the vessel proximally and mark its course on the skin up to the midmedial cubital fossa
- Draw the superficial venous vessels in the mid- and lateral forearm
- Inflating the tourniquet to just above diastolic pressure may help delineate the superficial veins
- Especially with fat arms, the cephalic vein may not be visible; use your anatomical knowledge to mark its probable course
- Before shaving the arm, note the hair growth in the intended harvesting area of the RFFF, in case the flap can be positioned more medially in the distal forearm where there is less hair (most flaps undergo radiation with loss of hair growth)
- Assess the fatty layer of the arm and reposition the flap if necessary
- Mark the flap design on the forearm
- Consider which side of the flap the vascular pedicle is to exit from:
- Which side of the neck will be used for the vascular anastomoses?
- What is the most favorable position for the pedicle at the reconstruction site to avoid kinking the pedicle?
- Determine the pedicle length required and draw the flap as distal as necessary
- Let the pedicle exit the flap on the edge closest to the anastomosis site
- Generally, the flap is centered over the radial artery
- The flap may be placed more medially if an osteocutaneous flap is to be used to provide more skin and soft tissue cover over the area of bone harvesting and the (probable) area of prophylactic plating of the radius
- Do not extend the flap too far over the lateral aspect of the forearm, because the cosmetic outcome of donor site will be worse. Sensitivity of the superficial radial nerve is also avoided if skin protection can be achieved over the nerve
- A risk of placing the flap too medially is that the cephalic vein may be positioned too laterally to be safely used as the draining vein. However, this is generally not the case; and the lateral part of the skin flap does not need to extend fully to the cephalic vein, as long as the intervening subdermal tissue between the skin flap and vein is preserved
Tourniquet
- Elevate the arm without exsanguinating it and inflate the tourniquet to at least 100 mmHg above the patient's systolic blood pressure. (Usually set at 250 mmHg)
- Record the tourniquet time (maximum time of 90 minutes permitted)
Elevating the RFFF
Many methods have been described. Some advocate elevating the flap from distal-toproximal in its entirety; others elevate the flap medially, then laterally, then distal-toproximal. The author has done >700 RFFFs and describes his preferred method.
Critical points
- Careful flap and template design
- Flap design on the forearm to include the lateral intermuscular septum as well as a superficial vein (usually cephalic)
- Elevate medial and lateral fasciocutaneous parts of the flap and dissect towards the lateral intermuscular septum
- Brachioradialis muscle is most critical element of elevating the flap
- Start flap elevation at lateral edge over brachioradialis muscle
- Progress towards intermuscular septum (not always well defined) and down to the lateral aspect of the artery
- Proceed to medial dissection
- Dissect vessels and elevate flap from distal-to-proximal
Author’s reasoning for above sequence
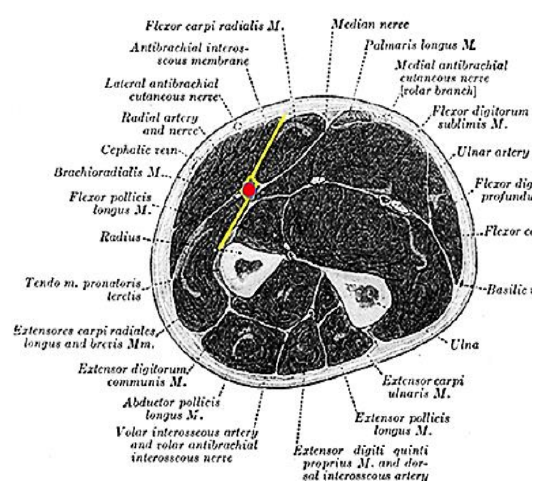
Figure 9: Cross-section of forearm demonstrating brachioradialis muscle, radial artery and oblique plane of the intermuscular septum
- Refer to the anatomy of the forearm (Figure 9)
- Note how the radial artery lies within the lateral intermuscular septum which extends obliquely (anteromedially) towards the skin (Figure 9)
- Posteromedial to the septum are the flexor muscles and specifically flexor carpi radialis
- Anterolaterally lie the muscle belly of brachioradialis proximally, and its flat tendinous part that covers the artery distally
- Therefore, to reach the radial artery the brachioradialis muscle and tendon need to be elevated like "opening a book"
- The artery and perforators are then visible as they run obliquely anteriorly, from lateral-to-medial
Subfascial RFFF elevation technique
This is the preferred technique for less experienced surgeons. Readers are referred to a later description of an alternate suprafascial/fascia-sparing elevation technique

Figure 10: Flap designed to include lateral intermuscular septum and superficial vein
- Design the flap on the forearm to include the lateral intermuscular septum as well as a superficial vein, usually the cephalic vein; the preferred position of the proximal extension is laterally between the radial artery and cephalic vein (Figure 10)
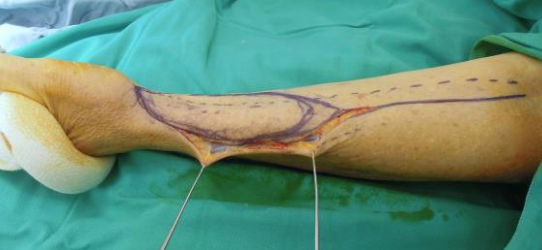
Figure 11: Skin incision along lateral aspect of flap (Left arm)
- Start the dissection laterally, with two skin hooks anchoring the skin lateral to the flap (Figure 11)
- Incise the circumference of the skin flap and the proximal curvilinear extension towards the cubital fossa with a No. 15 scalpel blade
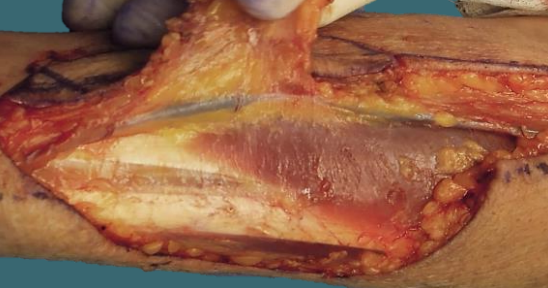
Figure 12: Skin flap elevated in deep subcutaneous plane to expose the cephalic vein
- Elevate the flap with a scalpel from laterally in a deep subcutaneous (not subdermal) plane until the cephalic vein which lies deep to the subcutaneous fat comes into view (Figure 12)
- Using a scalpel, elevate the cephalic vein from lateral-to-medial with the intervening subcutaneous tissue between vein and flap (Figure 12)

Figure 13: Arrow points to lateral antebrachial cutaneous nerve parallel to cephalic vein
- Elevate and skeletonize the cephalic vein proximal to the flap (Figure 13)
- The lateral antebrachial cutaneous nerve accompanies the cephalic vein in the same subcutaneous plane (Figure 13). If an innervated flap is planned, this nerve is elevated with the cephalic vein
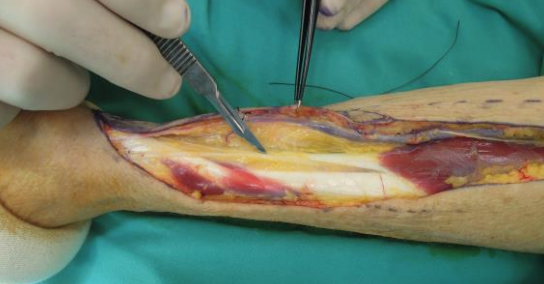
Figure 14: Scalpel points to superficial branch of radial nerve lateral to brachioradialis
- Separate the vein without its surrounding soft tissue from the main vascular pedicle using sharp scalpel dissection
- Elevate the lateral aspect of the flap in a subfascial plane over the extensor and abductor tendons with a No. 15 scalpel blade (Figure 14)
- Identify the superficial branch of the radial nerve lateral to the brachioradialis and medial to the extensor pollicis brevis and abductor pollicis longus (Figure 14)
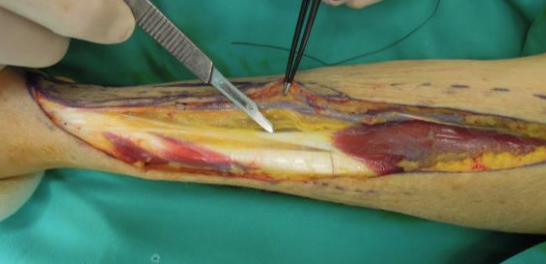
Figure 15: Scalpel points to brachioradialis tendon
- Extend the dissection medially over the epitenon covering the latter two tendons and the radial nerve, until the flat tendon of brachioradialis is visualized (Figure 15)
- It is very important to maintain epitenon over these tendons to provide a "cover" for skin grafting, if required
- Carefully continue with sharp dissection over the brachioradialis tendon up to its sharp medial edge
- To retract the brachioradialis muscle and tendon, the assistant stands on the radial side of the arm and the surgeon sits next to the trunk of the patient where he/she is protected from physical interference by the resection team

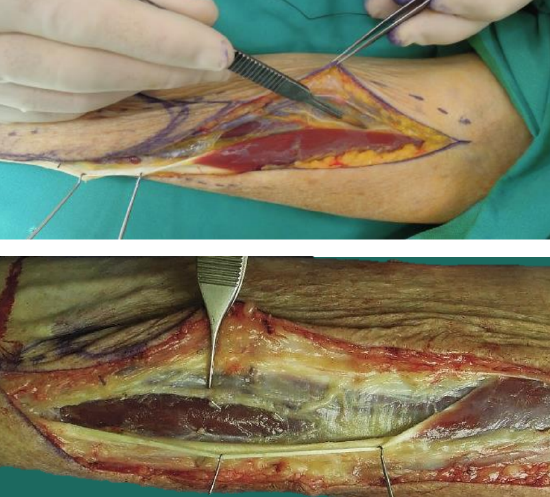
Figure 16: Sharp medial edge of brachioradialis tendon, and cutting along undersurface of brachioradialis tendon
- While the assistant applies lateral traction to the muscle with skin hooks, release the medial edge of the brachioradialis muscle off the (poorly defined) underlying lateral intermuscular septum using sharp dissection (Figure 16)
- Sharply dissect and elevate the tendon superiorly up to its musculotendinous junction; the radial artery generally lies immediately below the tendon; therefore, the angle of the scalpel blade is changed to a horizontal plane to cut along the under surface of the brachioradialis tendon (Figure 16)

Figure 17: Perforators within the septum are vulnerable to injury where they hook around the medial edge of brachioradialis tendon
- Distally, the perforators commonly hook around the medial edge of the brachioradialis tendon where they are vulnerable to injury, especially when incising perpendicularly past the medial edge of the tendon (Figure 17)
Figures 18a, b: Medial edge of brachioradialis tendon and muscle (retracted) and incising muscle fascia lateral to vascular pedicle
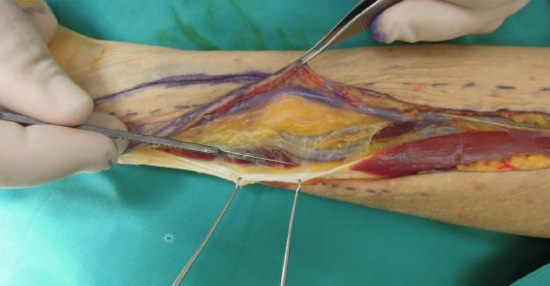
Figure 19: Brachioradialis muscle mobilized to expose full length of radial artery

Figure 20: Dividing muscle perforators
- Incise the fascia overlying the muscle lateral to the vascular pedicle (Figure 18)
- Once the brachioradialis muscle has been mobilized, the full length of the radial artery is visible and the likelihood of injuring the perforators is much less (Figure 19)
- Ligate and divide larger muscle perforators with Liga clips and coagulate small ones with bipolar forceps (Figure 20)
- Next elevate the medial side of the flap by cutting the epimysium covering the wrist flexor muscles with a scalpel
- Elevate the deep fascia over the tendons, but preserve the epitenon covering the tendons
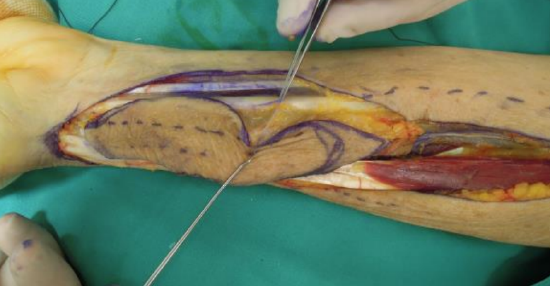
Figure 21: Elevate the deep fascia over the tendons, preserving epitenon
- Elevate beyond the flexor carpi radialis and incise the deeper muscle fascia over the flexor digitorum superficialis muscle (Figure 21)

Figure 22: Radial artery
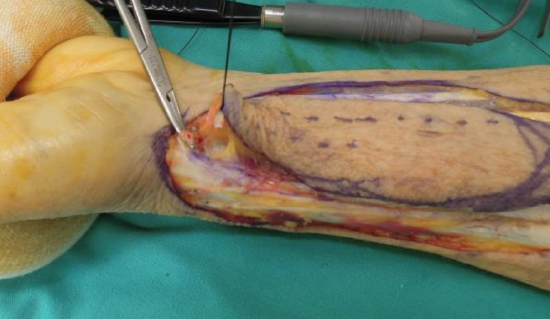
Figure 23: Radial artery divided

Figure 24: Distal-to-proximal dissection
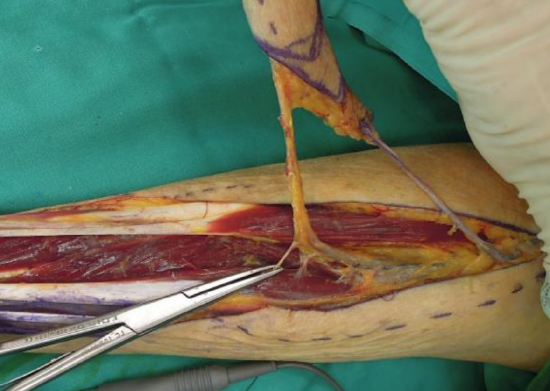
Figure 25: Applying Liga clips and dividing side branches of the radial artery; note the cephalic vein
- Incise the fascia over the radial artery and isolate, ligate and transect the artery and venae comitantes (Figures 22, 23)
- Dissection now proceeds from distalto-proximal (Figure 24)
- Meticulously divide the side-branches along the artery until enough vessel length is achieved to reach the recipient vessels in the neck; this permits drainage of both the superficial and deep venous systems via a single venous anastomosis (Figure 25)
- Selecting a vein as drainage vessel
- The cephalic vein may be divided at any point along its course
- The cephalic vein may be dissected into the cubital fossa where connections may exist between one (or both) branches of the venae comitantes of the radial artery and, more commonly to the median cubital or the cephalic veins
- More rarely the deep and superficial systems are anastomosed separately, utilizing the cephalic and one of the large cubital veins
- Occasionally a very large dominant median vein of the forearm can be used
- Avoid using venae comitantes for anastomoses if at all possible, due to their small size
- Deflate the tourniquet
- While awaiting reperfusion of the flap vasculature, the surgeon prepares the recipient vessels in the neck
- Control bleeding side-branches on the pedicle and on the flap with bipolar coagulation and/or Liga clips before disconnecting the flap from its blood supply
Reconstruction site
Check the reconstruction site for bleeding. Inspect the neck dissection for bleeding and ask the anesthetist to perform a Valsalva maneuver to demonstrate bleeders or lymphatic leaks.
Recipient vessels and nerves
The recipient vessels are selected and prepared for anastomosis. The distance between the recipient artery and vein must allow the donor vessels to reach both vessels comfortably, although this is not a problem when the cephalic vein is used as it is totally separate from the main vascular pedicle.
The recipient artery is selected according to size; access; and position to avoid kinking or excessive tension. The facial artery is most commonly used, although a more inferiorly placed artery such as the superior thyroid artery or even the transverse cervical artery may in some cases be a better choice.
The author's preference for venous anastomosis is the internal jugular vein, followed by the common facial vein and external jugular vein.
If sensory innervation of the flap is planned using the lateral antebrachial nerve, the surgeon should identify and mark e.g. the lingual nerve with a suture at the time of tumor resection, as the nerve may be difficult to identify later.
Transfer and inset of flap
- Only after the recipient area and recipient vessels have been fully prepared are the flap vessels divided
- Prepare the vessels for anastomotic suturing
- Ensure that there is no bleeding from the flap before transferring it to the neck
- Refer to chapter: Principles and technique of microvascular anastomosis for free tissue transfer flaps in head and neck reconstructive surgery
Suprafascial RFFF elevation technique
The main reason for elevating the RFFF suprafascially is to reduce the failure rate of the skin graft by maintaining a fascial covering over the exposed tendons. It does also allow the flap to be thinned in patients with very thick subcutaneous fat layers (Extreme care should be taken if the latter is attempted).
Only the most lateral and medial parts of the flap may be partially thinned of deep fat. More extensive thinning of the flap may interrupt critical blood supply by the perforators.
- Elevate the flap laterally, including the cephalic vein, which lies superficial to the fascia
- Maintain a superficial dissection plane up to the medial edge of the brachioradialis tendon
- Incise the deep fascia at the medial edge of the tendon, but not beyond
- Perform the brachioradialis tendon and muscle elevation and mobilization as described previously
- Incise the deep fascia on the pronator quadratus, flexor pollicis longus and flexor digitorum superficialis lateral to the vascular pedicle
- Suprafascially elevate the medial extent of the flap up to the lateral edge of the flexor carpi radialis tendon and muscle
- Incise the deep fascia beyond this point down to the deeper muscles (flexor pollicis longus and flexor digitorum superficialis)
- Complete the flap elevation as previously described
- Following complete elevation of the flap, it is often possible to approximate the two edges of the cut deep fascia to achieve complete fascial closure (Figure 26). If not, at least the tendons have a more reliable cover to avoid loss of the skin graft, exposed tendons and infection

Figure 26: Edges of deep fascia approximated to achieve complete fascial closure
Composite flaps
The palmaris longus muscle and tendon are commonly used for tendon transfers and as grafts for tendon or ligament reconstruction. In the head and neck the tendon is mainly used in total or near-total lower lip reconstruction to suspend the lower lip to the facial muscles at the oral commissure or to the maxilla. Harvesting the tendon or muscle does not cause significant loss of hand function. The palmaris longus tendon is identified preoperatively and easily incorporated in the flap by incising the deep fascia medial to the tendon down to the deeper muscles when medially elevating the flap, and including the tendon in the flap. The palmaris longus muscle and tendon may be absent in up to 15% of individuals. In such situations the flexor carpi radialis tendon may be incorporated in the flap with minimal functional deficit of hand and wrist flexion.
Osteocutaneous RFFF
Addition of radius bone to a RFFF has some major benefits including having a composite flap with a long pedicle and thin, pliable skin for soft tissue reconstruction; vascularized bone which is not bulky; and the ability to use the flap for structural bone and soft tissue reconstruction without reverting to the use of two flaps, such as a forearm flap in combination with a fibula flap (although the latter combination may still be required).
The osteocutaneous RFFF is used especially in midface and periorbital reconstruction, but also as an "onlay" vascularized bone flap following marginal mandibulectomy and may occasionally be used for segmental defects of the ascending ramus of the mandible. It may also be use in total nasal reconstruction to provide an “L” strut and internal nasal lining (See clinical examples at end of chapter).
Disadvantages compared to a free fibula flap include lack of bone stock for osseointegrated implants, inadequate bone strength for reconstruction of areas subjected to greater force and torque e.g. the symphysis, parasymphysis and body of the mandible; limited bone length; and the risk of subsequent forearm fracture.
The available bone lies between the insertion of the pronator teres muscle on a small area on the mid-lateral radius, and the insertion of brachioradialis laterally at the base of the radial styloid. Up to 40% of the circumference may be harvested. To avoid a subsequent fracture, prophylactic plating is done after the bone has been harvested.
- It is preferable to place the flap more medially on the forearm so that the area of harvesting and the plate are covered with intact skin
- This might preclude the use of the cephalic vein and the lateral antebrachial nerve, as they may lie too far laterally
- Periosteal and musculoperiosteal perforators provide the blood supply to the bone. Great care should be taken to elevate the brachioradialis tendon by cutting horizontally underneath the tendon with a No.15 blade to avoid injury to the perforators exiting the radial artery laterally that supply the bone and flexor pollicis longus and pronator quadratus muscles
- Extend the dissection deep to brachioradialis more laterally by widely retracting the tendon and muscle and dissecting beneath the superficial radial nerve

Figure 27: Perforators to the bone are identified and protected
- Identify and protect the perforators to the bone (Figure 27)
- Elevate the medial part of the flap Incise the deep fascia over the pronator quadratus, flexor pollicis longus and flexor digitorum superficialis muscles
- Retract the flap and vascular pedicle laterally (distal pedicle not yet divided)

Figure 28: Muscle perforators entering the muscle
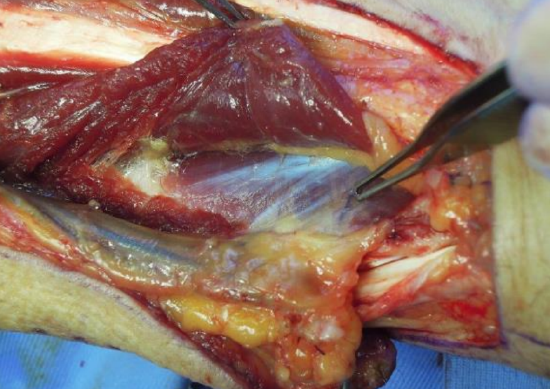
Figure 29: Flexor digitorum superficialis partially released to expose the flexor pollicis longus muscle and the lateral intermuscular septum and vascular pedicle
- Flexor carpi radialis may need to be retracted medially to expose the flexor digitorum superficialis muscle (radial head). Muscle perforators enter the muscle (Figure 28)
- Partially release the flexor digitorum superficialis from inferior to superior, enough to expose the flexor pollicis longus muscle and its origin from the anterior surface of the radius (Figure 29)
- Retract the cut flexor digitorum superficialis medially while gently retracting the lateral intermuscular septum and vascular pedicle laterally (Figure 29) The thickness of the radial bone is determined proximally during the dissection and a longitudinal cut is made through the flexor pollicis longus and periosteum on the medial surface of the radius with a No. 15 scalpel blade
- Mark the length of bone required starting 2.5 cm proximal to the radial styloid to permit distal fixation of the plate, and mark the proximal end
- A maximum length of about 12 cm can be harvested, but even more can be used if the insertion of pronator teres is detached from the radius and later reattached to the bone or plate
- A high-speed oscillating saw, directed from the medial/ulnar side, is used to divide the radius along its length, starting proximally where the radius has a smaller circumference; do not start cutting distally, as one may end up with too little bone stock proximally
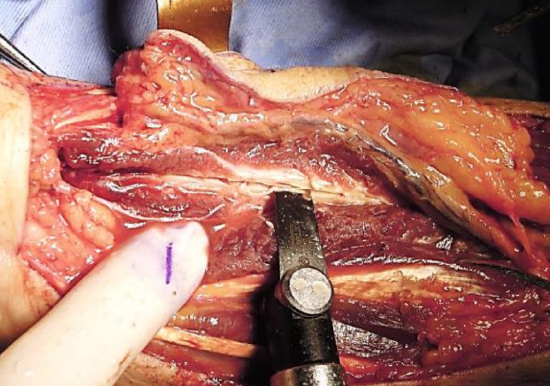
Figure 30: Cutting cortices longitudinally while protecting radial nerve and laterally placed tendons with a metal (copper) plate
- Divide both cortices longitudinally; use a metal plate held on the dorsolateral side to protect the radial nerve and the laterally placed tendons (Figure 30)
- The volar-lateral segment is used in the flap
- Make the cut so that approximately 60% of the dorsomedial circumference remains

Figure 31: Beveled ends of bone
- Bevel the proximal and distal osteotomies at an angle of about 50o to avoid a weak (stress) point (which would occur if it was to be cut at 90o) (Figure 31)
- To avoid cutting too deep when doing the two osteotomies, insert a ruler in the longitudinal cut to act as a stopper 2
- Elevate the flap from distal to proximal

Figure 32: Plating of radius
- Avoid fracturing the remaining radius (disastrous and very difficult to manage) by prophylactically doing a plate fixation with an appropriate thickness plate (Figure 32)
- To insert the plate, firm retraction of the abductor pollicis longus and the long extensors of the thumb are required distally and proximally for exposure
- The supinator muscle may need to be partially detached to place the plate
- It is probably better not to bend the plate to the contour of the bony defect, but to bridge the gap which may allow more bone formation beneath the plate
- At least 2 bicortical screws are placed distally and 3 bicortical screws proximally
- Mobilize skin over the lateral forearm to cover the plate
- The soft tissue is covered with a skin graft
- A volar splint is worn for 2 weeks
Innervated sensate RFFF
The lateral antebrachial cutaneous nerve runs alongside the cephalic vein and is well suited for simple, rapid inclusion of the nerve with a RFFF (Figure 1). Its cutaneous supply closely matches most RFFF designs. When designing a more medially placed RFFF as with an osteocutaneous flap, the medial antebrachial nerve may be a better choice (Figure 1). The nerve is connected to an appropriate sensory nerve in the area to be reconstructed e.g. mental, inferior alveolar or lingual.
Achieving additional bulk
Additional soft tissue bulk may be required e.g. when reconstructing the orbit following orbital exenteration. This can be achieved by de-epithelializing part of the RFFF and folding the fascial component of the RFFF into the cavity.
Optimizing cosmetic result of forearm donor site
- Attempt to advance skin to cover the exposed tendons
- Skin grafts
- Maintain epitenon over tendons
- Bury tendons by oversewing with deeper muscles
- Always fix and immobilize skin graft with sutures and appropriate dressings
- Use volar splint to restrict movement of flexor tendons beneath skin graft
- Negative pressure wound therapy (NPWT) of the donor site for 1 week may improve the graft bed by improving the bed vascularity, achieving granulation tissue cover over exposed tendons and a smoother graft bed. A drawback is that a 2nd surgical procedure is required for skin grafting
- Suprafascial flap elevation (Author’s preferred method)
- Flap reconstruction of smaller round or more horizontally orientated defects. This may be achieved with an ulnar based V-Y rotation-advancement flap which is based on perforators from the ulnar artery
- Avoid using meshed skin grafts on the forearm. They leave an unsightly, permanent "patterned" scar
Clinical examples of RFFFs

Figure 33: Soft palate and tonsil fossa

Figure 34: Hemiglossectomy

Figure 35: Lower lip reconstruction (Courtesy of CR Leemans)
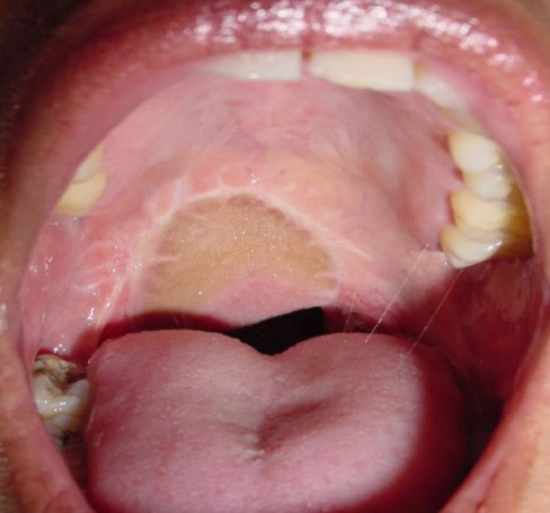
Figure 36: Soft palate reconstruction

Figure 37: Buccal reconstruction
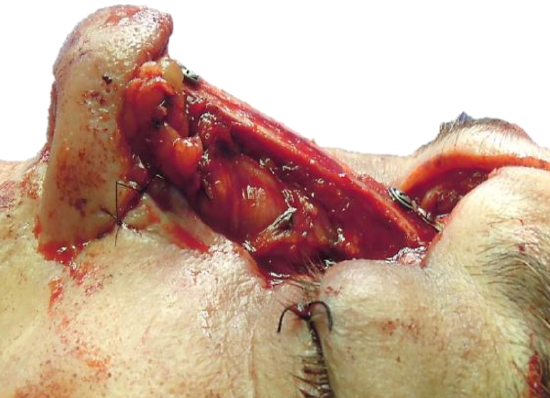
Figure 38: Total nasal reconstruction with osteocutaneous RFFF providing “L” strut and internal nasal lining, with forehead flap for external skin
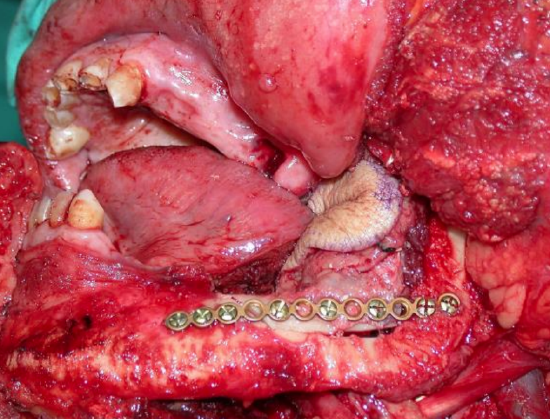
Figure 39: Onlay osteocutaneous RFFF
References
- Saint-Cyr M, Mujadzic M, Wong C, Hatef D, Lajoie A, Rorich R. The radial artery pedicle perforator flap: Vascular analysis and clinical implications. Plast Reconstr Surg. 2010 125: 1469-78
- Shnayder Y, Tsue TT, Toby EB, Werle AH, Girod DA. Safe Osteocutaneous Radial Forearm Flap Harvest with Prophylactic Internal Fixation. Craniomaxillofacial Trauma & Reconstruction. 2011;4(3):129-36
Other flaps described in The Open Access Atlas of Otolaryngology Head & Neck Operative Surgery
- Pectoralis major flap
- Buccinator myomucosal flap
- Buccal fat pad flap
- Nasolabial flap
- Temporalis muscle flap
- Deltopectoral flap
- Paramedian forehead flap
- Upper and lower trapezius flaps
- Cervicofacial flaps
- Submental artery island flap
- Supraclavicular flap
- Latissimus dorsi flap
- Local flaps for facial reconstruction
- Free fibula flap
- Rectus abdominis flap
- Anterolateral free thigh flap
- Thoracodorsal artery scapular tip (TDAST) flap
- Principles and technique of microvascular anastomosis for free tissue transfer flaps in head and neck reconstructive surgery
Author
JE (Ottie) Van Zyl MBChB, FCS
Plastic & Reconstructive Surgeon
Groote Schuur Hospital
Cape Town, South Africa
ottie@mweb.co.za
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


