5.12: Rectus Abdominis Free Tissue Transfer Flap
- Page ID
- 53283
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
RECTUS ABDOMINIS FLAP FOR HEAD & NECK RECONSTRUCTION
Patrik Pipkorn, Brian Nussenbaum
The rectus abdominis flap is based on the deep inferior epigastric artery. It is a composite flap and comprises muscle, overlying fascia and skin. It is versatile and provides a large volume of soft tissue and is technically straightforward to raise. Many variations based on the inferior epigastric artery, including perforator flaps, have been described.
In the head and neck it is typically used to reconstruct large oral defects, skull base defects, maxillectomy defects or whenever a large volume of soft tissue is required. In the head and neck it has more recently been largely supplanted by the anterolateral thigh free flap.
Benefits of the rectus flap include
- Technically straightforward and quick to harvest
- Constant anatomy with anatomic variations being rare
- Harvesting in a supine position makes a two-team approach feasible
- Provides the largest volume of soft tissue based on a single pedicle
- Long pedicle and 2-4 mm diameter artery
- Reliable perforators that do not need to be dissected or visualized
- Low donor site morbidity
Caveats include
- Obesity makes for a very bulky skin flap and might preclude its use
- Take care to look for previous abdominal surgery that might have disrupted the vascular supply. Most abdominal surgery is done through a midline incision and does not interfere with vascularity. Prior surgery might also make harvesting more difficult due to scarring and increase the risk of entering the peritoneal cavity
Surgical anatomy
Rectus sheath (Figures 1-5)
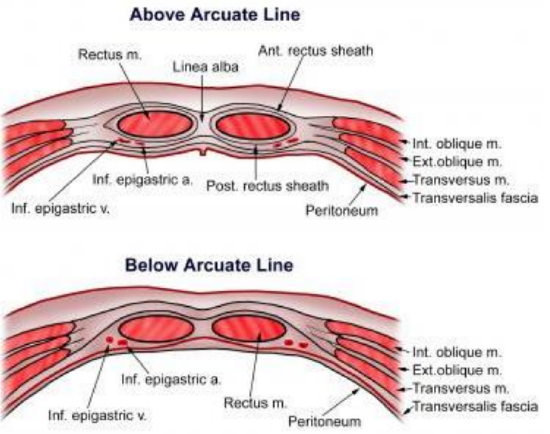
Figure 1: Anterior abdominal wall cross sectional anatomy and arcuate line
The rectus sheath is an aponeurosis arising from the external oblique, internal oblique and transversus abdominis muscles (Figure 1). It encircles the paired rectus muscles. The anterior and posterior rectus sheaths merge in the midline to form the linea alba that separates the paired rectus muscles (Figure 1).
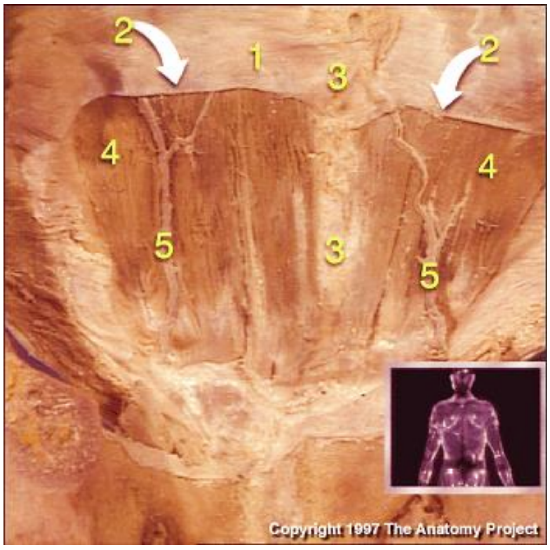
Figure 2: Posterior wall of rectus sheath (1); Arcuate line (2); Linea alba (3); Rectus abdominis (4); Inferior epigastric vessels (5)
When harvesting a rectus flap, the anterior rectus sheath is incised vertically over the midportion of the rectus muscle, whereas the posterior sheath is preserved. The arcuate line (Figures 1, 2) is located a few centimeters below the umbilicus or at the level of the anterior superior iliac spine and demarcates the lower limit of the posterior layer of the rectus sheath. Above the arcuate line the internal oblique aponeurosis splits and contributes to both the anterior and posterior rectus sheaths. Below the arcuate line, the internal oblique and transversus abdominis aponeuroses contribute only to the anterior rectus sheath (Figure 1, 2, 5); the posterior rectus sheath here consists of the transversalis fascia and is considerably weaker. This is an important surgical consideration as the anterior rectus sheath should not be excised below the arcuate line as the abdominal wall will be considerably weaker and be more prone to herniation.
Rectus abdominis muscle
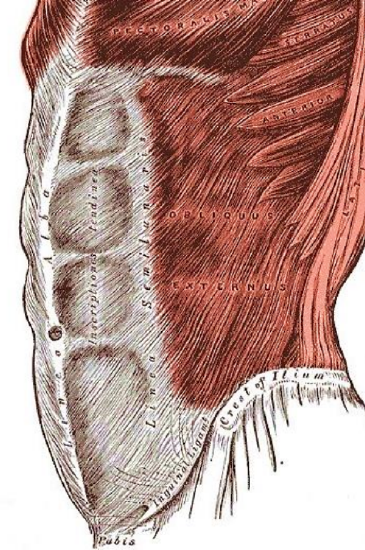
Figure 3: External oblique inserts into linea semilunaris; linea alba in midline
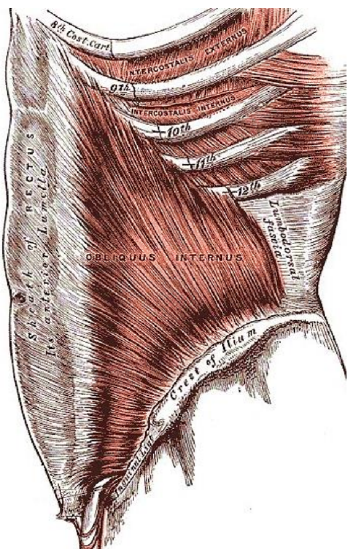
Figure 4: Internal oblique aponeurosis splits around rectus muscle to contribute to whole anterior layer of rectus sheath (above), but is absent posteriorly below arcuate line
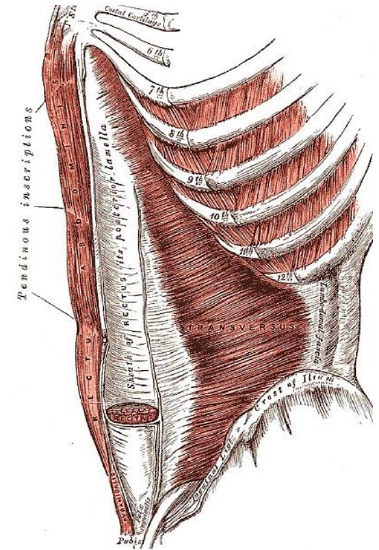
Figure 5: Transversus abdominis aponeurosis contributes to posterior layer of rectus sheath, but is absent posteriorly below the arcuate line
The rectus abdominis muscles are paramedian, paired, vertically oriented muscles in the anterior abdominal wall (Figures 1-5). Each muscle arises from the pubic tubercle and inserts into the xiphoid process and the 5th - 7th ribs of the anterior chest wall. Its primary function is to flex the trunk. Three bands of connective tissue named tendinous inscriptions (Figure 5) traverse the muscle to create three to four separate muscle bellies, giving the appearance of a “six pack” in well-trained people.
Vascular supply
The rectus abdominis has a rich blood supply. It is primarily supplied by the inferior and superior epigastric vessels. The rectus muscle also receives blood supply laterally from small contributions from the lower six intercostal arteries.
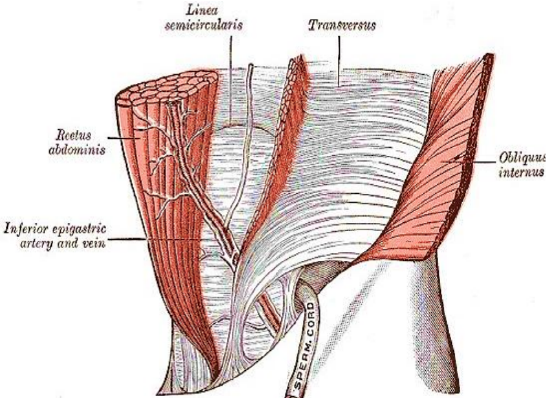
Figure 6: Arcuate line (linea semilunaris) and inferior epigastric vessels
The flap is based on the inferior epigastric artery. The inferior epigastric artery arises from the external iliac artery and courses superiorly in an extraperitoneal plane (Figures 2, 6).
It crosses the lateral border of the rectus muscle and pierces the transversalis fascia about 3-4 cm inferior to the arcuate line (Figures 2, 6). It then continues superiorly on the posterior aspect of the muscle between the muscle and the posterior rectus sheath. Superiorly it anastomoses with the superior epigastric artery. It gives off musculocutaneous perforators along its superior course. The highest density of perforators is located in the periumbilical area.
The superior epigastric artery arises from the internal thoracic (internal mammary) artery. It travels inferiorly on the posterior aspect of the sternum along the sternocostal junctions giving off perforators. These perforators also supply the deltopectoral flap and may be encountered when raising a pectoralis flap when the muscle is divided medially.
Innervation
The muscle has segmental innervation from thoracoabdominal nerves T7-T11
Surgical steps
Informed consent
A preoperative discussion should include the risk of seroma or haematoma formation, of developing unsightly scars and of an abdominal hernia. Patients must be counselled about the risks of flap failure and postoperative paralytic ileus. The strength of the abdominal wall will also be affected which can affect one’s ability for athletic and other strenuous activities.
Prepping and draping (Figure 7)
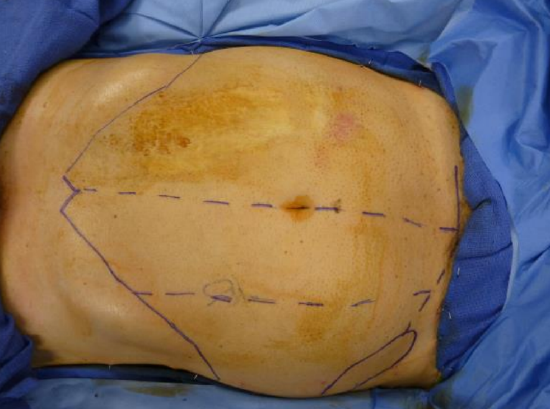
Figure 7: Prepping and draping
The abdomen is prepped and draped in a standard sterile fashion from just above the xiphoid, laterally along the midaxillary line and inferiorly along the inguinal ligament to permit harvesting of the whole muscle if needed and dissection of the pedicle (Figure 7).
Skin paddle
- Design the flap only after resecting the tumor and inspecting the defect
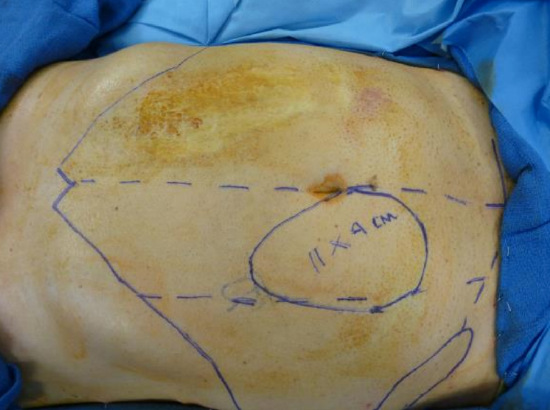
Figure 8: Skin paddle includes periumbilical area
- Draw the skin paddle (Figure 8)
- Perforators supply a large area of skin via the subdermal plexus
- Generally, 8-10 cm of skin can be harvested with primary closure of the donor site
- A simple pinch test will give assurance that there is enough laxity for primary closure of the donor site
- Although skin paddles can be harvested in different orientations, it should include the periumbilical area as the largest and most reliable perforators are located within a few centimeters of this area
- A variety of fasciocutaneous flaps with muscle sparing techniques requiring perforator dissection have also been described
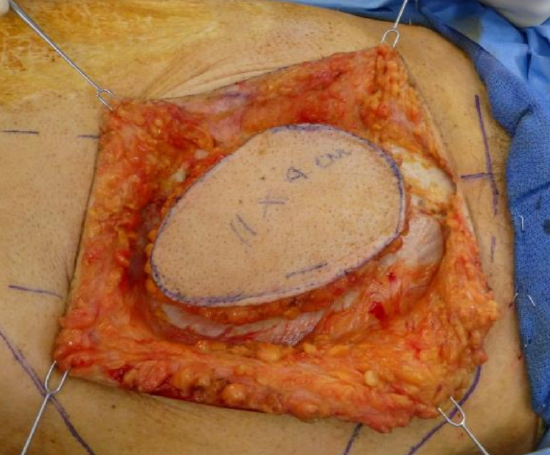
Figure 9: Circumferential exposure of rectus sheath
- Circumferentially incise the skin and subcutaneus tissue through adipose tissue, Scarpa’s fascia and down to the rectus sheath (Figure 9)
Raise flaps circumferentially to expose the linea alba in the midline and linea semilunaris laterally which marks the transition between rectus abdominis and external oblique. There is nothing to hurt in this area as the vascular pedicle runs deep to muscle
Incising the anterior rectus fascia
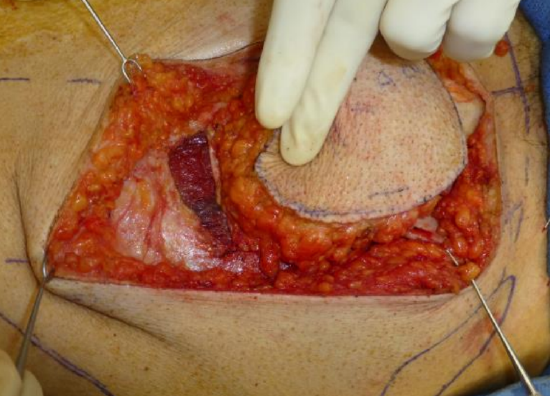
Figure 10: Incising rectus sheath superiorly to expose the rectus muscle
- Start superiorly (Figure 10)
- Using careful blunt dissection medial to the linea semilunaris in a lateral-to-medial fashion, the surgeon can often identify the first set of perforators (This step is not essential)
- Incise the fascia lateral to these perforators, leaving a cuff of rectus sheath laterally to facilitate later closure of the sheath
- If skin from the contralateral side is to be incorporated, then this skin is dissected towards the flap until linea alba is encountered
- Incise the anterior rectus sheath 1 cm lateral to the linea alba to leave a cuff for later closure
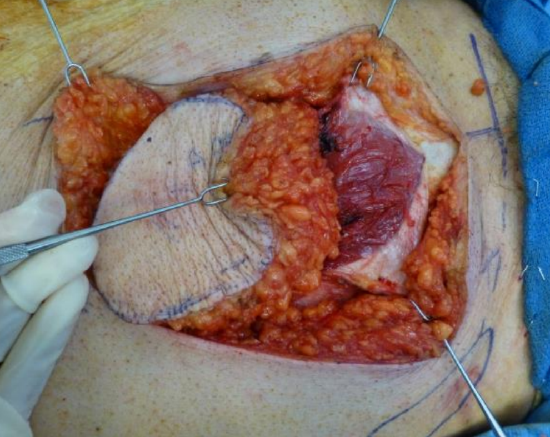
Figure 11: Incising rectus sheath inferiorly
- Next incise the skin inferiorly over the rectus muscle, gently curving inferolaterally to later facilitate easier dissection of the inferior epigastric pedicle (Figure 11)
- Expose the entire anterior rectus sheath inferior to the skin paddle down to the inguinal region
- Incise the anterior rectus sheath vertically over the midportion of the rectus muscle
Rectus muscle
- The whole muscle or portions thereof can be used
- The flap will shrink and lose bulk with time due to significant muscle atrophy, especially if postoperative radiation is employed
- A good rule of thumb is to harvest about 20-30% more tissue than the size of the defect
- To minimize muscle atrophy, segmental nerves can be anastomosed to motor nerves in the neck
- Transect the muscle superiorly at a suitable level
- Reflect the muscle from lateral-to-medial
- This exposes the segmental nerves which are transected
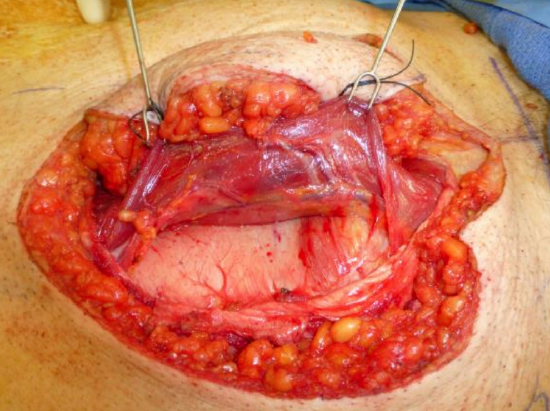
Figure 12: Inferior epigastric vessels exposed following division of segmental nerves
- Further reflection exposes the undersurface of the rectus muscle and the inferior epigastric vessels (Figure 12)
Vessel dissection
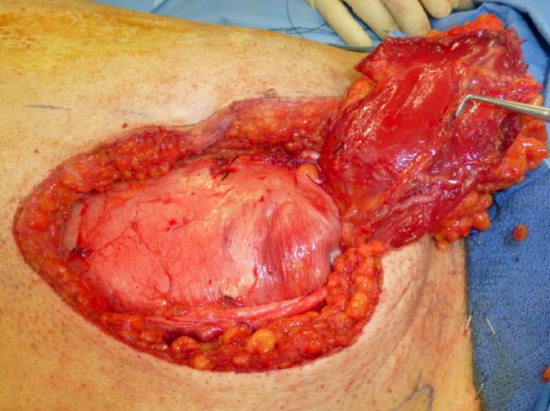
Figure 13: Inferior epigastric vessels exposed after ligating the vessels superiorly and reflecting the muscle inferiorly
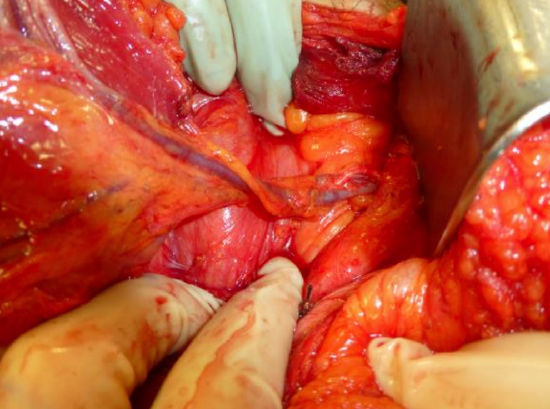
Figure 14: Inferior epigastric vessels being dissected towards the external iliacs

Figure 15: Rectus flap with its vascular pedicle
- Using large retractors, dissect the pedicle proximally (Figures 13, 14)
- Divide and ligate the pedicle proximally (Figure 15)
- Even if a long pedicle is not required, it is often useful to dissect the pedicle all the way to its origin from the external iliac vessels, as the inferior epigastric veins often merge at a variable distance from the external iliac vein
Closure

Figure 16: Preparing to suture the cut edges of the rectus sheath
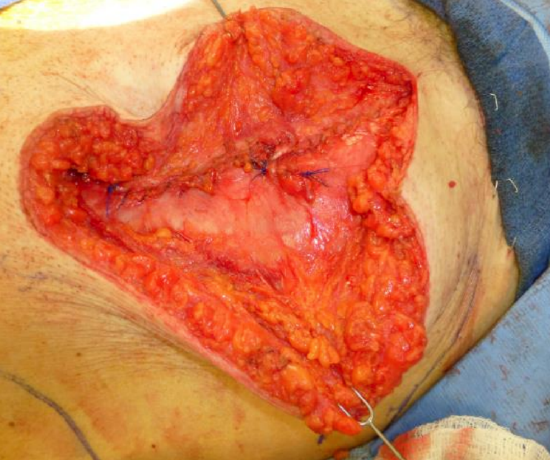
Figure 17: Sutured rectus sheath
- Reapproximate the anterior rectus sheath with large nonabsorbable sutures e.g. 0-Prolene (Figures 16, 17)
- Although the posterior rectus sheath superior to the arcuate line is probably strong enough, the remnants of the anterior rectus sheath at the level of flap are also reapproximated with nonabsorbable sutures taking great care not to inadvertently incorporate any peritoneum with the suture
- If direct suturing is not possible, consider using a mesh to strengthen the abdominal wall

Figure 18: Sutured skin and suction drain
- Close the skin; undermining the skin may be required to ensure a tension free closure, and insert a suction drain (Figure 18)
Postoperative care
- Postoperative paralytic ileus as a consequence of retracting the abdominal cavity contents while dissecting the pedicle is not uncommon; withhold feeds until this resolves
- Mobilize the patient early
- Exercises that involve the abdomen may be resumed about six weeks following surgery
Rectus flap for total glossectomy defect (Figures 19a-c)
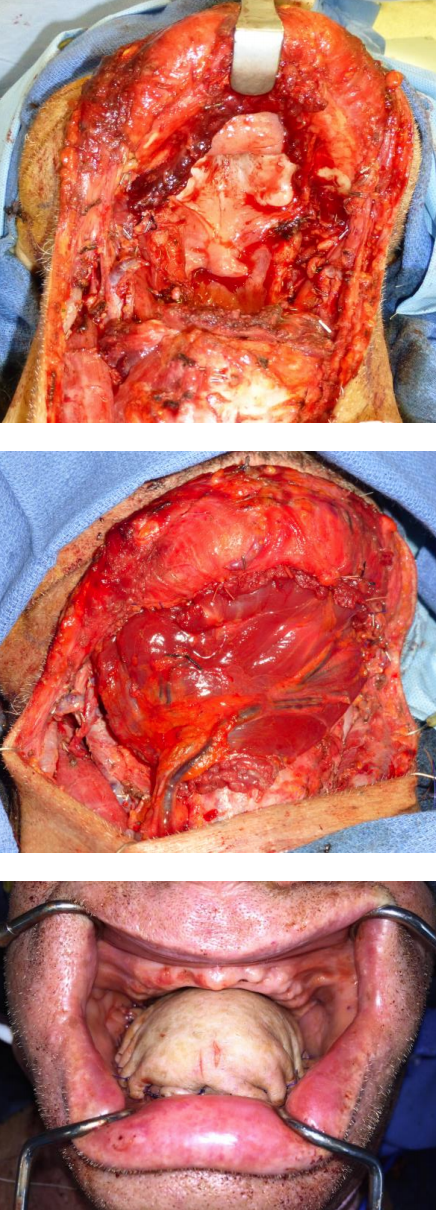
Figures 19a-c
Other flaps described in The Open Access Atlas of Otolaryngology Head & Neck Operative Surgery
- Pectoralis major flap
- Buccinator myomucosal flap
- Buccal fat pad flap
- Nasolabial flap
- Temporalis muscle flap
- Deltopectoral flap
- Paramedian forehead flap
- Upper and lower trapezius flaps
- Cervicofacial flaps
- Submental artery island flap
- Supraclavicular flap
- Latissimus dorsi flap
- Local flaps for facial reconstruction
- Radial free forearm flap
- Free fibula flap
- Anterolateral free thigh flap
- Thoracodorsal artery scapular tip (TDAST) flap
- Principles and technique of microvascular anastomosis for free tissue transfer flaps in head and neck reconstructive surgery
Authors
Patrik Pipkorn MD, Fellow, Head & Neck & Microvascular Reconstruction
Washington University
St Louis, MO, USA
patrikpipkorn@hotmail.com
Brian Nussenbaum, MD
Christy J. & Richard S. Hawes III Professor
Otolaryngology - Head & Neck Surgery Director, Head & Neck Surgical Oncology
Vice Chair of Clinical Affairs
Washington University
St Louis, MO, USA
Nussenbaumb@ent.wustl.edu
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


