14.3: Autonomic Synapses, Effects and Reflexes
- Page ID
- 22349
By the end of this section, you will be able to:
- Describe the synapses, signaling molecules and receptors involved in communication within the two divisions of the autonomic nervous system
- Determine the effect of the autonomic nervous system on the regulation of the various organ systems
- Explain autonomic tone and dual innervation
- Compare the structure of somatic and autonomic reflexes and differentiate between short and long reflexes
Autonomic Synapses
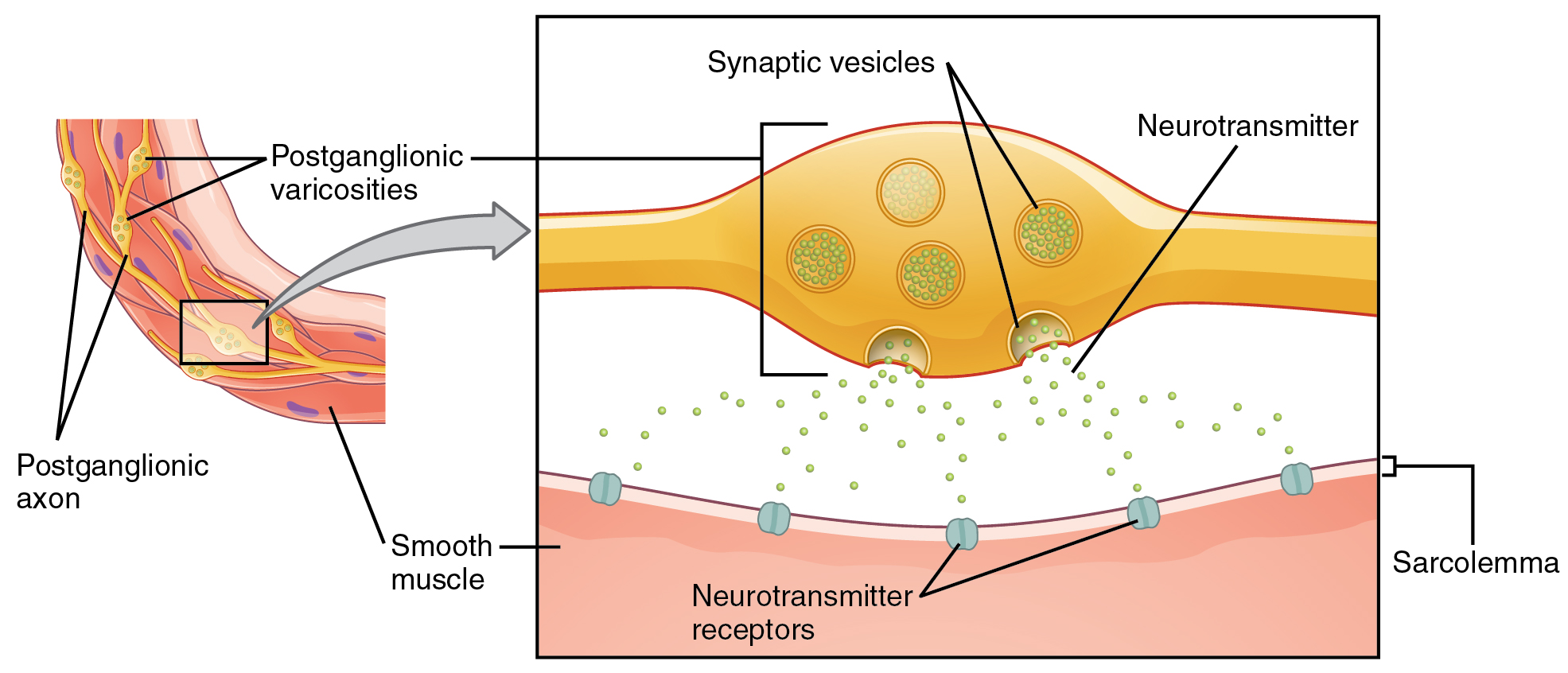
Where an autonomic neuron connects with a target, there is a synapse. What are referred to here as synapses may not fit the strictest definition of synapse. The structure of postganglionic connections are not the typical synaptic end bulb that is found at the neuromuscular junction, but rather are chains of swellings along the length of a postganglionic fiber. This place of connection is called a varicosity and is typical of the autonomic nervous system (ANS) (Figure \(\PageIndex{1}\)). Each postganglionic axon has a high number of these endings resembling a string of beads. At each varicosity, synaptic vesicles containing neurotransmitters are present and ready to merge with the plasma membrane of the axon to release the neurotransmitters. On the target organ (smooth muscle, cardiac muscle or glands) neurotransmitter receptors are present.
Autonomic Neurotransmitters
Signaling molecules can belong to two broad groups. Neurotransmitters are released at synapses, whereas hormones are released into the bloodstream. However, the same molecule (for example epinephrine) can be released by neurons within the brain as a neurotransmitter or by the adrenal medulla into the bloodstream as a hormone, blurring the lines between these definitions. The main signaling molecules of the autonomic nervous system are acetylcholine (ACh) and norepinephrine (NE, also called noradrenaline). The adrenal medulla which is a modified sympathetic ganglion releases epinephrine (or adrenaline). These molecules will bind to specific receptors on the target cells. Cells that release acetylcholine are called cholinergic, while cells that release norepinephrine or epinephrine are called adrenergic. Acetylcholine can bind to both nicotinic receptors and muscarinic receptors. Norepinephrine and epinephrine can bind to adrenergic receptors. For each of these classes of receptors, there are multiple subtypes (which we will not discuss in this book) that make the cells respond differently to the binding of the same molecule. Depending on the receptor type and subtype, the molecules released will cause either stimulation or inhibition. Thus, the effects of the autonomic divisions depend on the type of signaling molecule and receptor involved.
All preganglionic fibers, both sympathetic and parasympathetic, are cholinergic and release ACh (Table \(\PageIndex{1}\)). All ganglionic neurons (the targets of these preganglionic fibers) have nicotinic receptors in their cell membranes, which leads to the stimulation and firing of an action potential from the ganglionic fibers in both sympathetic and parasympathetic divisions. Most sympathetic postganglionic fibers are adrenergic and release norepinephrine. The adrenal medulla which is part of the sympathetic division is also adrenergic and releases epinephrine. However, parasympathetic postganglionic fibers are cholinergic and release ACh. This pattern assures that effector organs under the control of both sympathetic and parasympathetic systems can respond differently. Target cells can contain various types and subtypes of receptors and their response will vary depending on the type of receptor and on the neurotransmitter released on them.
There is one exception to this pattern in the sympathetic system. The sympathetic postganglionic fibers that contact the blood vessels within skeletal muscle and sweat glands in the integument release ACh instead of norepinephrine. This does not create any problem because there is no parasympathetic input to these organs. Blood vessels of skeletal muscles and sweat glands have muscarinic receptors and vasodilate (increase diameter size) and produce and secrete sweat, respectively, in response to ACh.
At most of the other autonomic targets that are innervate by both divisions of the autonomic system, the effector response is based on which neurotransmitter is released and what receptor is present. For example, regions of the heart that establish heart rate are contacted by postganglionic fibers from both systems. If norepinephrine is released, it binds to an adrenergic receptor which causes the heart rate to increase. If ACh is released, it binds to a muscarinic receptor that causes the heart rate to slow. Without this parasympathetic input, the heart would work at a rate of approximately 100 beats per minute (bpm). The sympathetic system speeds that up, as it would during exercise, to 120–140 bpm, for example. The parasympathetic system slows it down to the resting heart rate of 60–80 bpm.
| Sympathetic Division | Parasympathetic Division | |
|---|---|---|
| Preganglionic axons | release ACh (cholinergic) | release ACh (cholinergic) |
| Ganglionic neurons | contain nicotinic (ACh) receptors | contain nicotinic (ACh) receptors |
| Postganglionic axons |
release NE (adrenergic); release ACh (cholinergic) only in blood vessels of skeletal muscle and sweat glands |
release ACh (cholinergic) |
| Adrenal medulla | contain muscarinic (ACh) receptors; releases epinephrine (adrenergic) |
Autonomic Effects
Organ systems are balanced between the input from the sympathetic and parasympathetic divisions. When something upsets that balance, the homeostatic mechanisms strive to return it to its regular state. For each organ system, there may be more of a sympathetic or parasympathetic tendency to the resting state, which is known as the autonomic tone of the system. For example, the resting heart rate is the result of the parasympathetic system slowing the heart down from its intrinsic rate of 100 bpm, consequently the heart can be said to be in parasympathetic tone.
Many effector organs of the autonomic nervous system have dual innervation, meaning that they receive competing inputs from the sympathetic and parasympathetic divisions. These divisions each play a role in effecting change, usually in competing directions. At the level of the target effector, the signal of which system is sending the message is strictly chemical and depending on the division involved and neurotransmitter released, the effects would be diverse. For example, the heart and the eye are examples of organs with dual innervation. The sympathetic system increases heart rate, whereas the parasympathetic system decreases heart rate. The sympathetic system dilates the pupil of the eye, whereas the parasympathetic system constricts the pupil.
In some organs, opposing effects are achieved without dual innervation. For example, the arrector pili muscles, sweat glands, and blood vessels to skeletal muscles and skin are primarily under sympathetic control. Blood pressure is partially determined by the contraction of smooth muscle in the walls of blood vessels. The parasympathetic system has no significant input to the systemic blood vessels, so the sympathetic system determines their tone. The sympathetic system causes vasoconstriction of blood vessels. However, the increasing metabolic activity of muscles causes (paracrine) vasodilation. This allows for blood flow to increase for those skeletal muscles that will be active in the fight-or-flight response.
Not always the sympathetic and parasympathetic divisions have opposite effects and, in a few cases, the two systems cooperate. The best example of cooperative effects occurs in the male sexual function. In reproductive organs, blood vessels of erectile tissues are innervate with parasympathetic projection, making them an exception. Acetylcholine released by these postganglionic parasympathetic fibers cause the vessels to dilate, leading to the engorgement of the erectile tissue and penile erection. At the same time, the sympathetic nervous system stimulates ejaculation by causing the contractions of the seminal vesicle and prostate gland. This synergistic effect facilitates reproduction.
Table \(\PageIndex{2}\) summarizes the effects on different organs of the sympathetic and parasympathetic divisions.
| Target Effector | Sympathetic Effect | Parasympathetic Effect |
|---|---|---|
| Arrector pili muscles | Contraction to cause hair erection | None |
| Sweat glands | Secretion | None |
| Salivary glands | Inhibits | Stimulates |
| Pupils | Dilation | Constriction |
| Ciliary muscle | None | Contraction for near vision |
| Heart | Increases heart rate | Decreases heart rate |
| Blood vessels of the heart (coronary) | Vasoconstriction or vasodilation | Vasodilation |
| Blood vessels to skeletal muscles | Vasodilation | None |
| Blood vessels to skin and other organs | Vasoconstriction to increase blood pressure | None |
| Blood vessels to gastrointestinal (GI) tract | Vasoconstriction | Vasodilation |
| Bronchi of lungs | Dilation | Constriction |
| Gastrointestinal (GI) tract gland secretion | Inhibits | Stimulates |
| Gallbladder | Inhibits | Stimulates |
| Peristalsis (motility) | Inhibits | Stimulates |
| Sphincters | Contraction (close) | Relaxation (open) |
| Urinary bladder | Relaxation | Contraction |
| Internal urethral sphincter | Contraction (close) | Relaxation (open) |
| Penis | Stimulates ejaculation | Stimulates erection |
| Clitoris | None | Stimulates erection |
Autonomic Reflexes
The autonomic nervous system regulates organ systems through circuits that resemble the reflexes described in the somatic nervous system. A somatic reflex, such as the withdrawal reflex, involves a . An autonomic reflex, also called visceral reflex, consists of contractions of smooth or cardiac muscle, or secretion by glands that are mediated by a reflex arc in response to a stimulus. Examples of autonomic reflexes are the initial release of urine (micturition), alteration of heart rate or blood pressure, regulation of digestion and modification of the pupil size. Somatic and visceral reflexes present similarities and differences.
One similarity between a somatic reflex and a visceral reflex is the afferent branch, that brings information towards the CNS. Sensory neurons receiving input from the periphery—with cell bodies in the sensory ganglia, either of a cranial nerve or a dorsal root ganglion adjacent to the spinal cord—project into the CNS to initiate the reflex.
Many of the inputs to visceral reflexes are from special or somatic senses, but particular senses are associated with the viscera that are not part of the conscious perception of the environment through the somatic nervous system. For example, there is a specific type of mechanoreceptor, called a baroreceptor, in the walls of the aorta and carotid sinuses that senses the stretch of those organs when blood volume or pressure increases. You do not have a conscious perception of having high blood pressure, but that is an important afferent branch of the cardiovascular and, particularly, vasomotor reflexes. The sensory neuron is essentially the same as any other general sensory neuron, a unipolar neuron that has a cell body in a sensory ganglion. The baroreceptors from the carotid arteries have axons in the glossopharyngeal nerve, and those from the aorta have axons in the vagus nerve.
Though visceral senses are not primarily a part of conscious perception, those sensations sometimes make it to conscious awareness. If a visceral sense is strong enough, it will be perceived. The sensory homunculus—the representation of the body in the primary somatosensory cortex—only has a small region allotted for the perception of internal stimuli. If you swallow a large bolus of food, for instance, you will probably feel the lump of that food as it pushes through your esophagus, or even if your stomach is distended after a large meal. If you inhale especially cold air, you can feel it as it enters your larynx and trachea. These sensations are not the same as feeling high blood pressure or blood sugar levels.
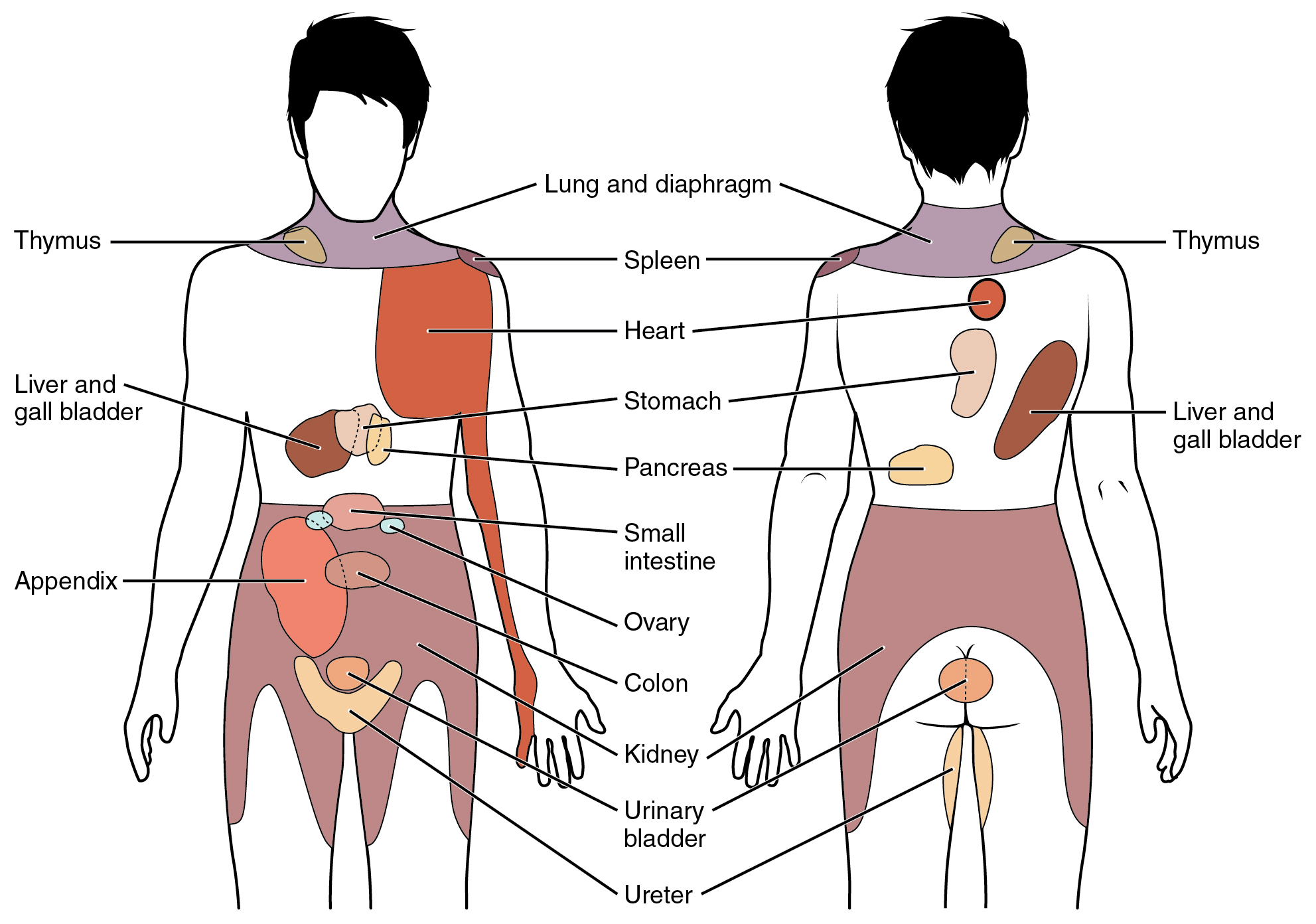
When particularly strong visceral sensations rise to the level of conscious perception, the sensations are often felt in unexpected places. For example, strong visceral sensations of the heart will be felt as pain in the left shoulder and left arm. This irregular pattern of projection of conscious perception of visceral sensations is called referred pain. Depending on the organ system affected, the referred pain will project to different areas of the body (Figure \(\PageIndex{2}\)). The location of referred pain is not random, but a definitive explanation of the mechanism has not been established. The most broadly accepted theory for this phenomenon is that the visceral sensory fibers enter into the same level of the spinal cord as the somatosensory fibers of the referred pain location. By this explanation, the visceral sensory fibers from the mediastinal region, where the heart is located, would enter the spinal cord at the same level as the spinal nerves from the shoulder and arm, so the brain misinterprets the sensations from the mediastinal region as being from the axillary and brachial regions.
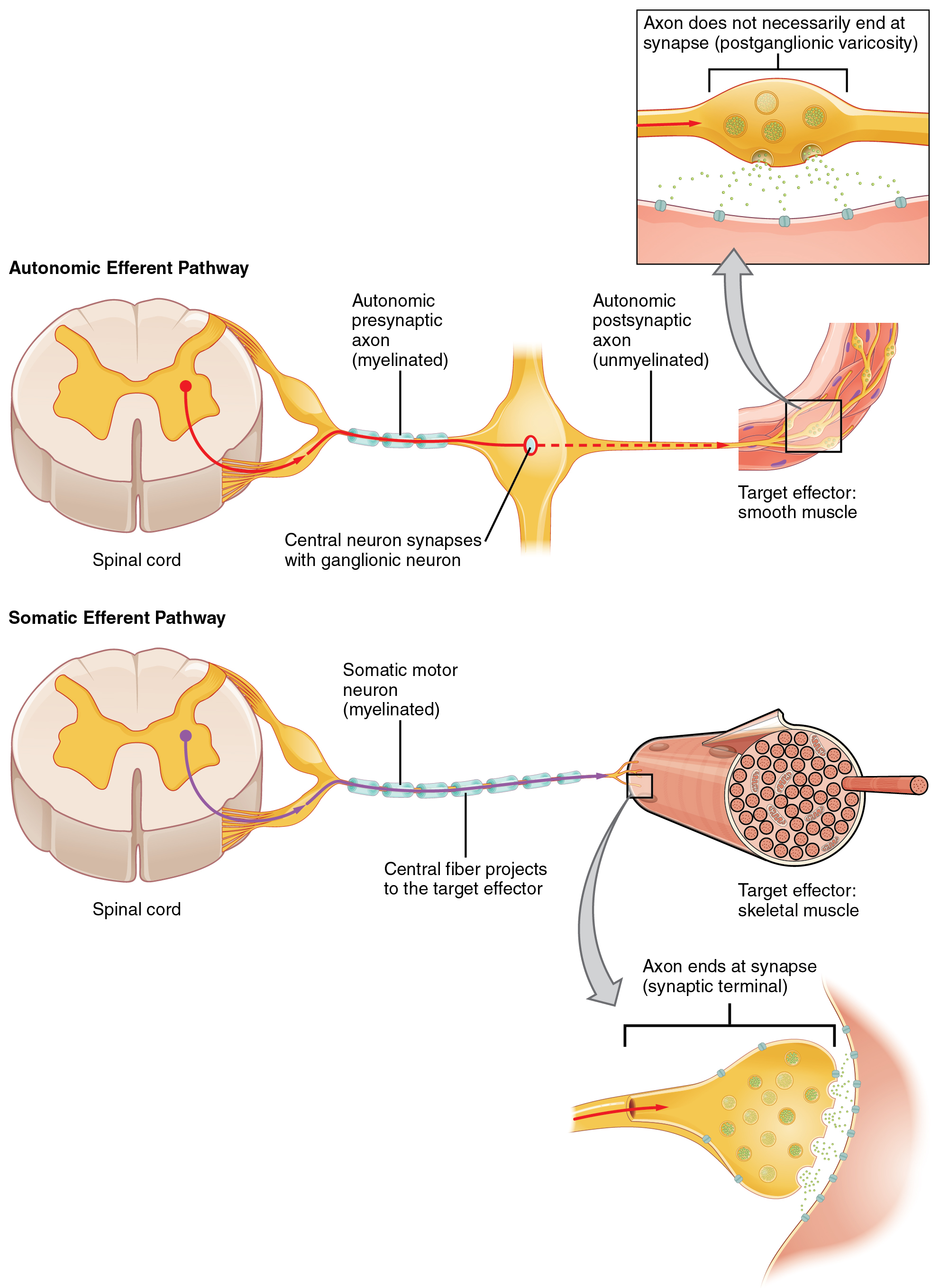
One difference between a somatic and visceral reflex is in the efferent branch. The output of a somatic reflex is the lower motor neuron in the ventral horn of the spinal cord that projects directly to a skeletal muscle to cause its contraction. The output of a visceral reflex is a two-step pathway starting with the preganglionic fiber emerging from a lateral horn neuron in the spinal cord, or a cranial nucleus neuron in the brainstem, to a ganglion—followed by the postganglionic fiber projecting to a target effector (Figure \(\PageIndex{3}\)).
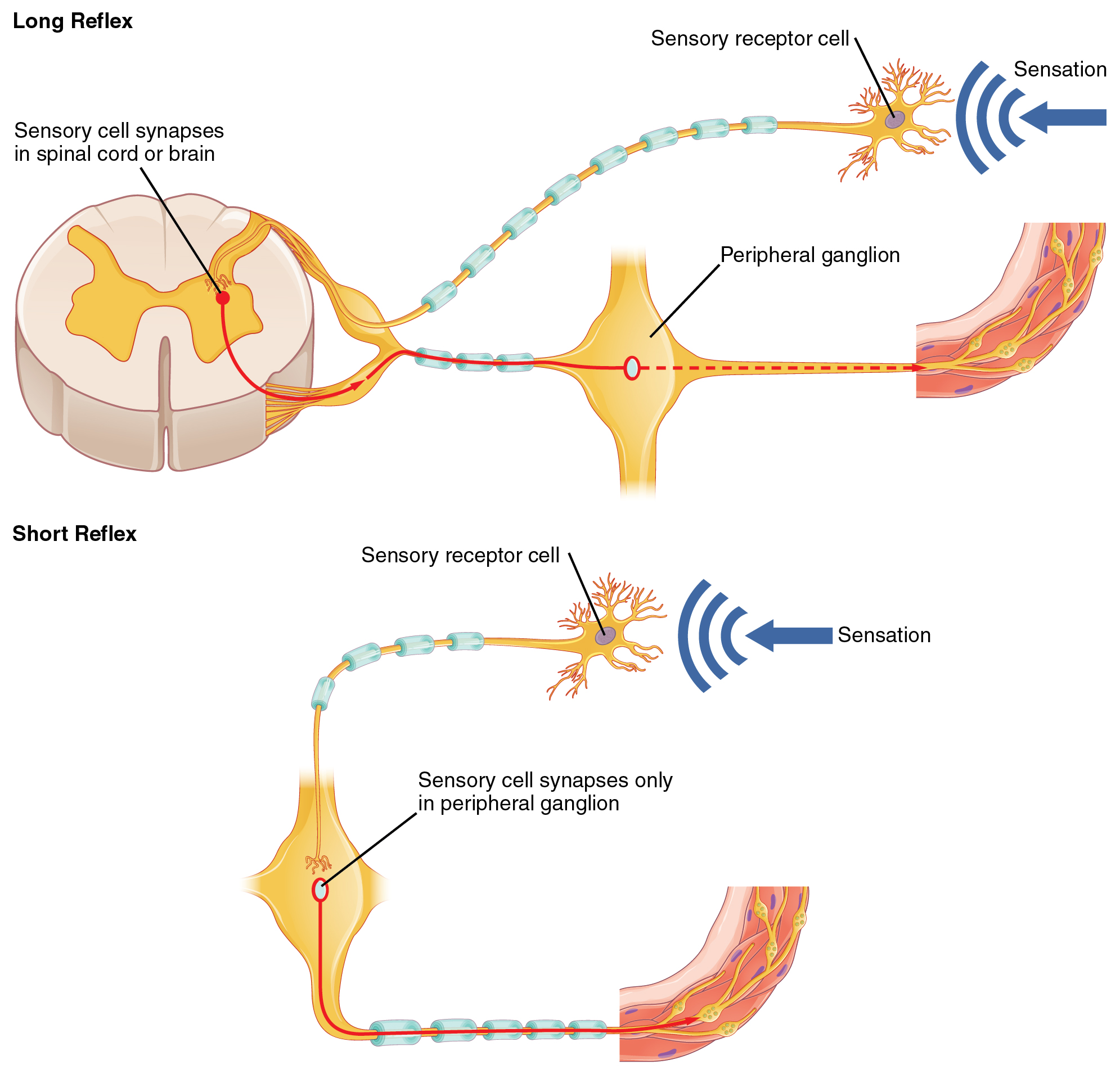
Short and Long Reflexes
Somatic reflexes involve sensory neurons that connect sensory receptors to the central nervous system (CNS) and motor neurons that project back out to the skeletal muscles. Visceral reflexes that involve the sympathetic or parasympathetic systems share similar connections. However, there are reflexes that do not need to involve any CNS components. A long reflex has afferent branches that enter the spinal cord or brain and involve the efferent branches. A short reflex is completely peripheral with sensory neurons synapsing with motor neurons in autonomic ganglia; the CNS is not involved (Figure \(\PageIndex{4}\)).
A division of the nervous system that is related to the autonomic nervous system is the enteric nervous system. The word enteric refers to the digestive organs, so this represents the nervous tissue that is part of the digestive system. There are a few myenteric plexuses in which the nervous tissue in the wall of the digestive tract organs can directly influence digestive function. If stretch receptors in the stomach are activated by the filling and distension of the stomach, a short reflex will directly activate the smooth muscle fibers of the stomach wall to increase motility to digest the excessive food in the stomach. No CNS involvement is needed because the stretch receptor is directly activating a neuron in the wall of the stomach that causes the smooth muscle to contract. That neuron, connected to the smooth muscle, is a ganglionic parasympathetic neuron that can be controlled by a fiber found in the vagus nerve.
DISORDERS OF THE...
Nervous System: Kehr’s Sign
Kehr’s sign is the presentation of pain in the left shoulder, chest, and neck regions following rupture of the spleen. The spleen is in the upper-left abdominopelvic quadrant, but the pain is more in the shoulder and neck. How can this be? The sympathetic fibers connected to the spleen are from the celiac ganglion, which would be from the mid-thoracic to lower thoracic region whereas parasympathetic fibers are found in the vagus nerve, which connects in the medulla of the brainstem. However, the neck and shoulder would connect to the spinal cord at the mid-cervical level of the spinal cord. These connections do not fit with the expected correspondence of visceral and somatosensory fibers entering at the same level of the spinal cord.
The incorrect assumption would be that the visceral sensations are coming from the spleen directly. In fact, the visceral fibers are coming from the diaphragm. The nerve connecting to the diaphragm takes a special route. The phrenic nerve is connected to the spinal cord at cervical levels 3 to 5. The motor fibers that make up this nerve are responsible for the muscle contractions that drive ventilation. These fibers have left the spinal cord to enter the phrenic nerve, meaning that spinal cord damage below the mid-cervical level is not fatal by making ventilation impossible. Therefore, the visceral fibers from the diaphragm enter the spinal cord at the same level as the somatosensory fibers from the neck and shoulder.
The diaphragm plays a role in Kehr’s sign because the spleen is just inferior to the diaphragm in the upper-left quadrant of the abdominopelvic cavity. When the spleen ruptures, blood spills into this region. The accumulating hemorrhage then puts pressure on the diaphragm. The visceral sensation is actually in the diaphragm, so the referred pain is in a region of the body that corresponds to the diaphragm, not the spleen
Concept Review
The synapses in the autonomic system are not always the typical type of connection first described in the neuromuscular junction. Instead of having synaptic end bulbs at the very end of an axonal fiber, they may have swellings called varicosities along the length of a fiber so that it makes a network of connections within the target tissue. All preganglionic fibers are cholinergic and release acetylcholine (ACh). All ganglionic neurons (the targets of these preganglionic fibers) have nicotinic receptors in their cell membranes. Most sympathetic postganglionic fibers are adrenergic and release norepinephrine. The adrenal medulla which is part of the sympathetic division is also adrenergic and releases epinephrine. Parasympathetic postganglionic fibers are cholinergic and release ACh. Target cells can contain various types and subtypes of receptors and their response will vary depending on the type of receptor and on the neurotransmitter released on them. The sympathetic postganglionic fibers that contact the blood vessels within skeletal muscle and sweat glands in the integument release ACh instead of norepinephrine. This does not create any problem because there is no parasympathetic input to these organs.
For each organ system, there may be more of a sympathetic or parasympathetic tendency to the resting state, which is known as the autonomic tone of the system. Many effector organs of the autonomic nervous system have dual innervation, meaning that they receive competing inputs from the sympathetic and parasympathetic divisions. The sympathetic system increases heart rate, whereas the parasympathetic system decreases heart rate. The sympathetic system dilates the pupil of the eye, whereas the parasympathetic system constricts the pupil. The competing inputs can contribute to the resting tone of the organ system. Heart rate is normally under parasympathetic tone, whereas blood pressure is normally under sympathetic tone. The heart rate is slowed by the autonomic system at rest, whereas blood vessels retain a slight constriction at rest. In a few systems of the body, the competing input from the two divisions is not the norm. The sympathetic tone of blood vessels is caused by the lack of parasympathetic input to the systemic circulatory system. Only certain regions receive parasympathetic input that relaxes the smooth muscle wall of the blood vessels. Sweat glands are another example of organs that only receive input from the sympathetic system. Not always the sympathetic and parasympathetic divisions have opposite effects and, in a few cases, the two systems cooperate.
Autonomic nervous system function is based on the visceral reflex, which is similar to the somatic reflex. Like the somatic reflex, the afferent branch is composed of sensory neurons receiving input from the periphery project into the CNS to initiate the reflex. The cell bodies of these sensory neurons are located in the sensory ganglia, either of a cranial nerve or a dorsal root ganglion adjacent to the spinal cord. However, the efferent branch of a visceral reflex is composed of two neurons. The central neuron projects from the spinal cord or brainstem to synapse on the ganglionic neuron that projects to the effector. The afferent branch of the somatic and visceral reflexes is very similar, as many somatic and special senses activate autonomic responses. However, there are visceral senses that do not form part of conscious perception. If a visceral sensation, such as cardiac pain, is strong enough, it will rise to the level of consciousness. However, the sensory homunculus does not provide a representation of the internal structures to the same degree as the surface of the body, so visceral sensations are often experienced as referred pain, such as feelings of pain in the left shoulder and arm in connection with a heart attack.
Review Questions
Q. Which of the following represents a sensory input that is not part of both the somatic and autonomic systems?
A. vision
B. taste
C. baroreception
D. proprioception
- Answer
-
C
Q. What is the term for a reflex that does not include a CNS component?
A. long reflex
B. visceral reflex
C. somatic reflex
D. short reflex
- Answer
-
D
Critical Thinking Questions
Q. A target effector, such as the heart, receives input from the sympathetic and parasympathetic systems. What is the actual difference between the sympathetic and parasympathetic divisions at the level of those connections (i.e., at the synapse)?
A. The postganglionic sympathetic fiber releases norepinephrine, whereas the postganglionic parasympathetic fiber releases acetylcholine. Specific locations in the heart have adrenergic receptors and muscarinic receptors. Which receptors are bound is the signal that determines how the heart responds.
Q. Damage to internal organs will present as pain associated with a particular surface area of the body. Why would something like irritation to the diaphragm, which is between the thoracic and abdominal cavities, feel like pain in the shoulder or neck?
A. The nerves that carry sensory information from the diaphragm enter the spinal cord in the cervical region where somatic sensory fibers from the shoulder and neck would enter. The brain superimposes this experience onto the sensory homunculus where the somatic nerves are connected.
Glossary
- acetylcholine
- neurotransmitter that binds at a motor end-plate to trigger contraction
- adrenergic
- cells that release norepinephrine or epinephrine, which bind to adrenergic receptors
- adrenergic receptor
- receptors to which epinephrine and norepinephrine bind
- afferent branch
- component of a reflex arc that represents the input from a sensory neuron, for either a special or general sense
- autonomic reflex
- reflex involving an internal organ as the effector, under the control of the autonomic nervous system; also known as visceral reflex
- autonomic tone
- tendency of an organ system to be governed by one division of the autonomic nervous system over the other, such as heart rate being lowered by parasympathetic input at rest
- baroreceptor
- mechanoreceptor that senses the stretch of blood vessels to indicate changes in blood pressure
- cholinergic
- cells that release acetylcholine, which binds to muscarinic or nicotinic receptors
- dual innervation
- innervation of a target organ by both sympathetic and parasympathetic divisions
- efferent branch
- component of a reflex arc that represents the output, with the target being an effector, such as muscle or glandular tissue
- epinephrine
- signaling molecule released from the adrenal medulla into the bloodstream as part of the sympathetic response
- long reflex
- reflex arc that includes the central nervous system
- muscarinic receptor
- type of acetylcholine receptor protein that is characterized by also binding to muscarine
- neurotransmitter
- chemical signal that is released from the synaptic end bulb or varicosities of a neuron to cause a change in the target cell
- neurotransmitter receptor
- receptor specific for a neurotransmitter
- nicotinic receptor
- type of acetylcholine receptor protein that is characterized by also binding to nicotine
- norepinephrine
- signaling molecule released as a neurotransmitter by most postganglionic sympathetic fibers as part of the sympathetic response, or as a hormone into the bloodstream from the adrenal medulla
- referred pain
- the conscious perception of visceral sensation projected to a different region of the body, such as the left shoulder and arm pain as a sign for a heart attack
- reflex arc
- circuit of a reflex that involves a sensory input and motor output, or an afferent branch and an efferent branch, and an integrating center to connect the two branches
- short reflex
- reflex arc that does not include any components of the central nervous system
- somatic reflex
- reflex involving skeletal muscle as the effector, under the control of the somatic nervous system
- varicosity
- enlargement of neurons that release neurotransmitters into synaptic clefts
- visceral reflex
- reflex involving an internal organ as the effector, under the control of the autonomic nervous system; also known as autonomic reflex
Contributors and Attributions
OpenStax Anatomy & Physiology (CC BY 4.0). Access for free at https://openstax.org/books/anatomy-and-physiology


