2.6: Clinical Techniques- The Neurological Assessment
- Page ID
- 41656
The central nervous system (CNS) consists of the brain and the spinal cord. The CNS receives sensory information from other parts of the body or the body’s external environment and transmits motor information to muscles and glands by way of the peripheral nervous system (PNS). The PNS of the human includes 31 pairs of spinal nerves and 12 pairs of cranial nerves. Some nerves contain only motor nerve fibers (efferent fibers); some nerves contain only sensory nerve fibers (afferent fibers); and some nerves contain both sensory and motor nerve fibers (mixed). All spinal nerves are mixed.
Cranial nerves
The I (olfactory), II (optic), and VIII (vestibulocochlear) nerves are entirely sensory. Cranial nerves III (oculomotor), IV (trochlear), VI (abducens), XI (accessory), and XII (hypoglossal) are classified as motor, although they do contain proprioceptive afferent fibers. Cranial nerves V (trigeminal), VII (facial), IX (glossopharyngeal), and X (vagus) are mixed. All cranial nerves except the olfactory nerves are connected to the brain stem (medulla, pons, mesencephalon), and all are distributed in the head and neck except the vagus, which also supplies structures in the thorax and abdomen. Figure 1a (below) shows cranial nerves and their origins and terminations. Figure 1b shows their origins on the brain.
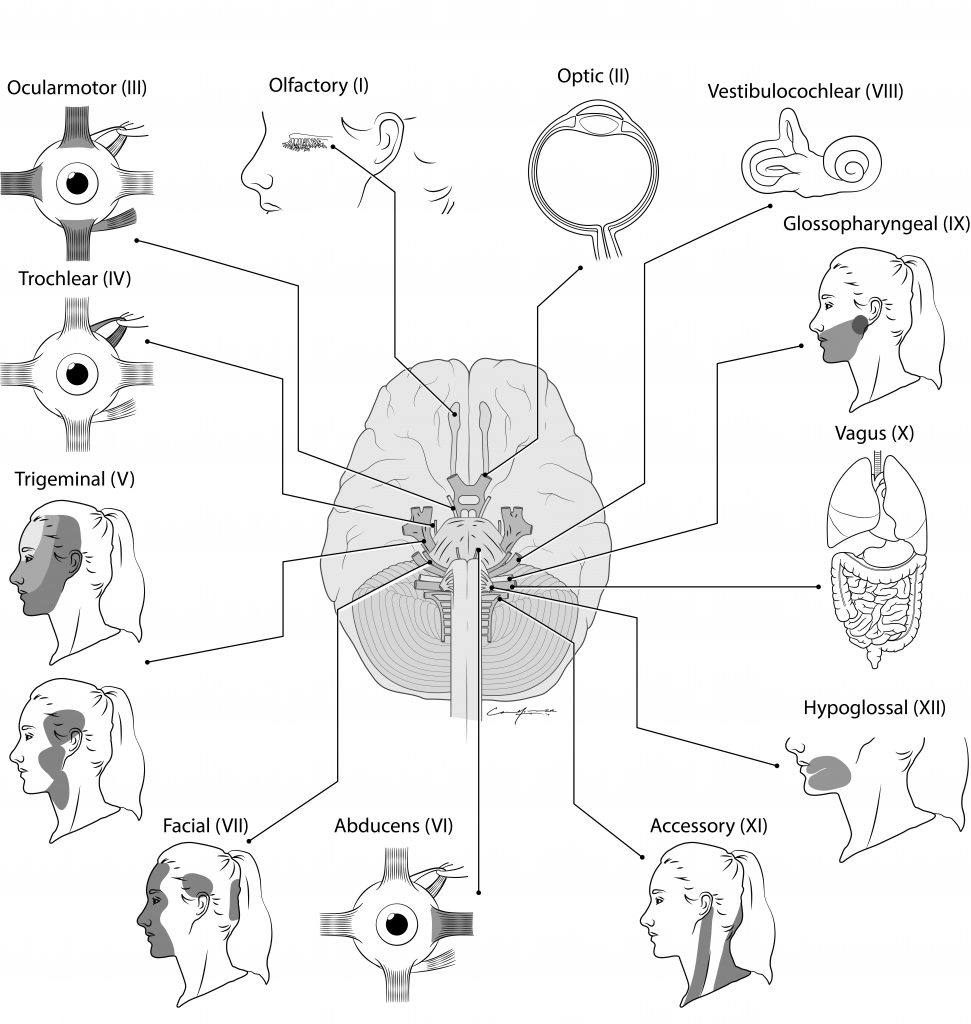
Cranial nerve function is commonly assessed as part of a general physical examination of the head, eyes, ears, nose, throat, and neck by physicians. More comprehensive examination of cranial nerve functions is usually done by specialists such as neurologists, ophthalmologists, optometrists, and audiologists.

Cranial Nerve I. Olfactory Nerve (Sensory)
Olfactory nerve fibers pass from bipolar olfactory neurons in the olfactory epithelium through the cribriform plate of the ethmoid bone and into the olfactory bulb, where they synapse with second-order neurons called Mitral cells. Neurons of the olfactory bulb transmit olfactory information along the olfactory tract to the olfactory cortex of the cerebrum. Damage to the olfactory epithelium, olfactory nerves, olfactory bulbs and tracts, or the olfactory cortex may produce a loss of the ability to smell (anosmia). The most common test for anosmia involves asking a subject to close their eyes and identify a scent.
Usually anosmia is due to damage to the nasal olfactory epithelium from excessive smoking, cocaine use, or inflammation due to infection. Neurologic causes include tumors of the frontal lobe near the olfactory bulbs and tracts and head injuries. As do other special senses (e.g., vision, hearing), the sense of smell diminishes with increasing age.
Clinical notes:Alzheimer’s Disease. Neurodegenerative changes in the olfactory bulb and brain regions that involve smell, including olfactory memory, have been associated with the onset of Alzheimer’s Disease (AD) dementia. A simple sniff test has been used to identify Alzheimer’s versus non-Alzheimer’s patients. In the test, blindfolded patients are asked to smell and identify peanut butter with the right or left nostril 10 cm from the nose. People with Alzheimer’s have trouble smelling the peanut butter, and, additionally, have a harder time smelling with the left nostril than the right. Because the sense of smell is often the first sense to be noticed in cognitive decline (before memory loss) the sniff test could be an effective tool for early intervention.
Cranial Nerve II. Optic Nerve (Sensory)
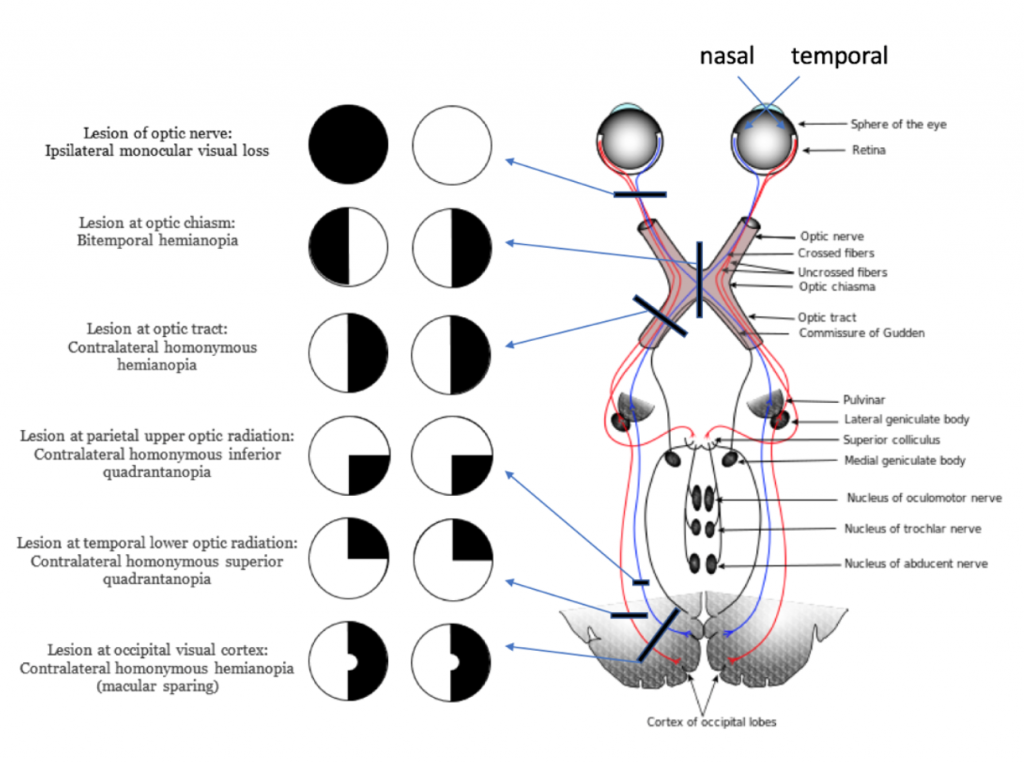
The optic nerve arises from cells in the retina of the eye and conveys visual information to the brain. Fibers from the medial half of each retina cross at the optic chiasma and are distributed to the contralateral brain stem, thalamus, and cerebral visual areas along with fibers from the ipsilateral temporal retina (see figure 2). Thus, both eyes are represented in the occipital cortex of each cerebral hemisphere. In addition to providing sensory information regarding vision, the optic nerve provides the sensory component of visual reflexes such as the pupillary light reflex and accommodation of the lens. Examination of the optic nerve involves determination of visual acuity, peripheral vision, and appearance of the optic fundus with an ophthalmoscope.
Visual acuity is checked with Snellen charts, which display letters of progressively smaller size. “Normal” vision is 20/20. This means that the test subject sees the same line of letters at 20 feet that person with normal vision sees at 20 feet. 20/40 vision means that the test subject sees at 20 feet what a person with normal vision sees at 40 feet. Another way of saying this is that a person with 20/40 vision has vision that is only half as good as normal.
Loss of vision in all or part of the visual field is caused by specific lesions in the visual pathway (figure 2). Blindness (represented by dark color) in one half of each visual field is called hemianopia. Lesions of one optic nerve will cause complete vision loss in the ipsilateral eye. Lesions of the optic tract or optic radiations produce the same hemianopia (homonymous hemianopia) for both eyes. A tumor of the pituitary gland may exert pressure on the optic chiasma causing bilateral loss of the temporal fields of vision.
Cranial Nerves III: Oculomotor, IV Trochlear, VI Abducens
Six extrinsic muscles move the eyeball within the orbit (figure 3). The inferior, superior, and medial recti muscles and the inferior oblique muscle are controlled by the oculomotor nerve. The lateral rectus is controlled by the abducens nerve, and the superior oblique muscle is controlled by the trochlear nerve.
The oculomotor nerve also controls the elevator muscle of the upper eyelid and the involuntary internal muscles of the eye that control pupil diameter and lens thickness. Because the oculomotor, trochlear, and abducens nerves control related functions of the eye, they are tested as a unit.
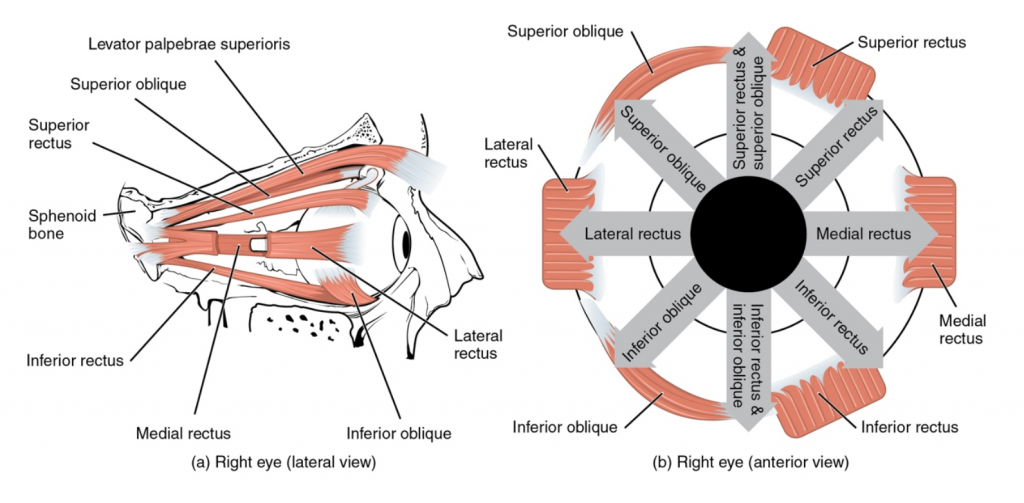
| Muscle | Effect of Contraction | Innervated by (including cranial nerve number): |
|---|---|---|
| Superior rectus | Eye rotates to look up | Oculomotor nerve (III) |
| Medial rectus | Eye rotates to look medially | Oculomotor (III) |
| Inferior rectus | Eye rotates to look down | Oculomotor (III) |
| Lateral rectus | Eye rotates to look laterally | Abducens (VI) |
| Superior oblique | Medial rotation | Trochlear (IV) |
| Inferior oblique | Lateral rotation | Oculomotor (III) |
Tests of these nerves involve looking at the eye structure, eyelid, and eye movement. Damage to the oculomotor nerve causes several unusual eye features, including ptosis, or drooping of an eyelid. Unequal pupils, called anisocoria, may be congenital and have no pathologic significance or may occur as a result of a variety of abnormalities, including syphilis, multiple sclerosis, and sympathetic paralysis. If both pupils are markedly smaller or larger than normal, medication may be the cause. A unilateral dilated pupil often occurs with increased intracranial pressure. The pupil becomes fixed and unresponsive to light on the side of the brain where the pressure has increased.
Extraocular muscles are tested by the H test where the subject is asked to follow a pen or finger tracing the shape of an H with their eyes. The ability to rotate the eyes medially, called convergence, allows the subject to focus on an object that is close to the face. Nystagmus, or involuntary, rapid, rhythmic shaking movement of the eyeball, may occur due to extraocular muscle weakness.
Cranial Nerve V. Trigeminal Nerve (Mixed)
The trigeminal nerve has two roots, one motor and the other sensory, arising from the pons (figure 1b). The motor fibers supply muscles of mastication (chewing), such as the temporalis and the masseter. The sensory fibers convey pain, temperature, touch, and pressure information from the eye, face, nasal and oral mucosa, gums, teeth, and anterior two-thirds of the tongue.
Fibers in the sensory root come from the trigeminal ganglion, which receives input from three divisions of sensory nerves: the ophthalmic (I), the maxillary (II), and the mandibular (III). The facial distribution of these divisions is shown in figure 4. Each division should be tested separately and bilaterally (on both sides).
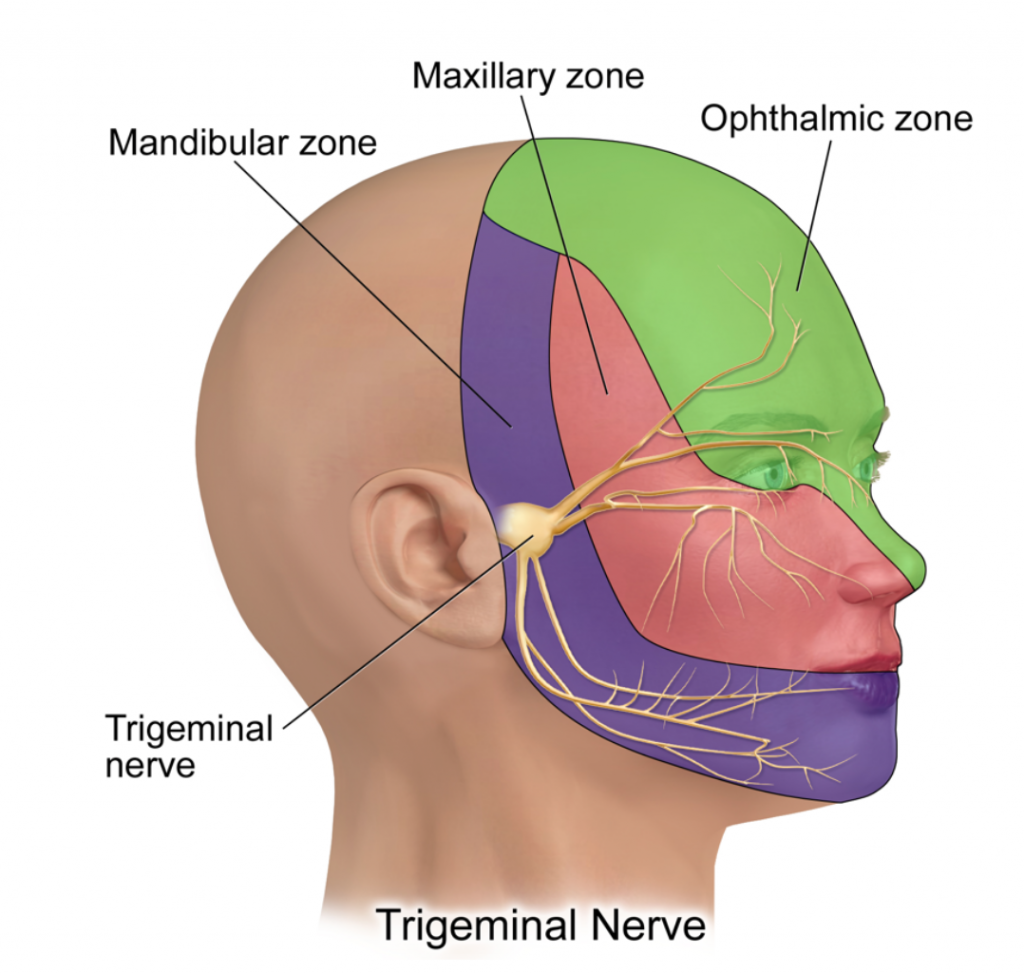
Injury to the sensory components of the trigeminal nerve causes anesthesia in the area of the affected division and, thus, may be tested for by a simple touch test. Tic douloureux (trigeminal neuralgia) is caused by irritation of the trigeminal nerve and is marked by excruciating pain that follows the distribution of the sensory fibers.
Cranial Nerve VII. Facial Nerve (Mixed)
The facial nerve arises from the pons lateral to the abducens nerve (figure 1b) and contains motor and sensory fibers. The motor fibers innervate muscles of facial expression, and parasympathetic fibers stimulate salivary glands. Sensory fibers convey taste information from the anterior two-thirds of the tongue.
One may test for facial nerve function by asking the subject to show teeth and smile, lift the eyebrows, frown, and close the eyes tightly. All facial movements should be equal bilaterally. Note any asymmetry of facial movements and features, but keep in mind that some persons habitually smile more on one side of the mouth than the other and that every face is somewhat asymmetrical.
Disease of the facial nerve results in peripheral facial paralysis (Bell’s palsy) on the side of the lesion. Causes of Bell’s palsy include compression of the nerve by a tumor and infections that inflame the nerve and surrounding tissue. The affected individual will be unable to close the eye on that side, wrinkle his or her forehead, or show teeth. Loss of muscle tone on the side of the lesion causes the corner of the mouth to droop.
Cranial Nerve VIII. Vestibulocochlear Nerve (Sensory)
The eighth cranial nerve contains fibers of the vestibular nerve and the cochlear nerve. The vestibular nerve is sensory from receptors in the inner ear that provide information concerning the movement of the body, balance, and body position in relation to gravitational force. The cochlear nerve is sensory from auditory (hearing) receptors in the cochlea of the inner ear.
The inability to hear some or all of the normally audible sounds could be caused by one or more of several disorders such as blockage of the outer ear canal (with wax, fluid, etc.): damage to the eardrum or ear ossicles: blockage of the internal auditory meatus and inflammation of the middle ear (common in upper respiratory infections); damage to the inner ear, auditory (hair cell) receptors, and auditory (cochlear) nerve; or damage to auditory pathways in the brain.
A useful test of hearing requires a 256-Hz tuning fork vibrating on the mastoid process (to test bone conduction) versus placing the fork directly in front of the ear (testing air conduction). A shortening of hearing time with air conduction coupled with preservation of hearing time with bone conduction suggests interference with sound transmission in the outer ear or the middle ear. If both the hearing time for bone conduction and the hearing time for air conduction are reduced, the hearing loss most likely involves the inner ear receptor hair cells or the auditory nerve (or both).
Cranial Nerve IX. Glossopharyngeal Nerve (Mixed), Cranial Nerve X. Vagus Nerve (Mixed)
The glossopharyngeal nerve supplies motor fibers to the parotid salivary gland and muscles in the pharynx (throat), larynx (voice box), and soft palate. Sensory fibers convey taste information from the posterior one-third of the tongue and information pertaining to blood pressure and blood chemistry from the carotid artery.
The vagus nerve supplies motor fibers to constrictor muscles of the pharynx, intrinsic muscles of the larynx, and involuntary muscles of the bronchi, heart, esophagus, stomach, small intestine, and part of the large intestine. Secretory motor fibers of the vagus supply the pancreas and secretory glands of most of the alimentary canal. The vagus is sensory from the laryngeal mucosa, heart, lungs, esophagus, stomach, small intestine, and part of the large intestine. In addition, vagal sensory fibers convey taste from the throat and epiglottis and blood pressure and chemistry information from the aorta. The ninth and tenth cranial nerves are tested together because their functions overlap.
A common test to determine IX and X function is to ask a subject to open his or her mouth and say “ahh.” The position of the soft palate and uvula at rest and with phonation is noted. Normally, the uvula and palate rise in the midline with phonation. Paralysis of cranial nerves IX or X on one side of the brain will cause the palate and uvula to deviate to the un-paralyzed side during phonation (figure 5).

Additionally, the absence of the gag reflex may result from a lesion of either the glossopharyngeal (sensory component) or vagus nerve (motor component) on the same side as the loss. If an abnormality is suspected, taste is tested on each side of the posterior one-third of the tongue.
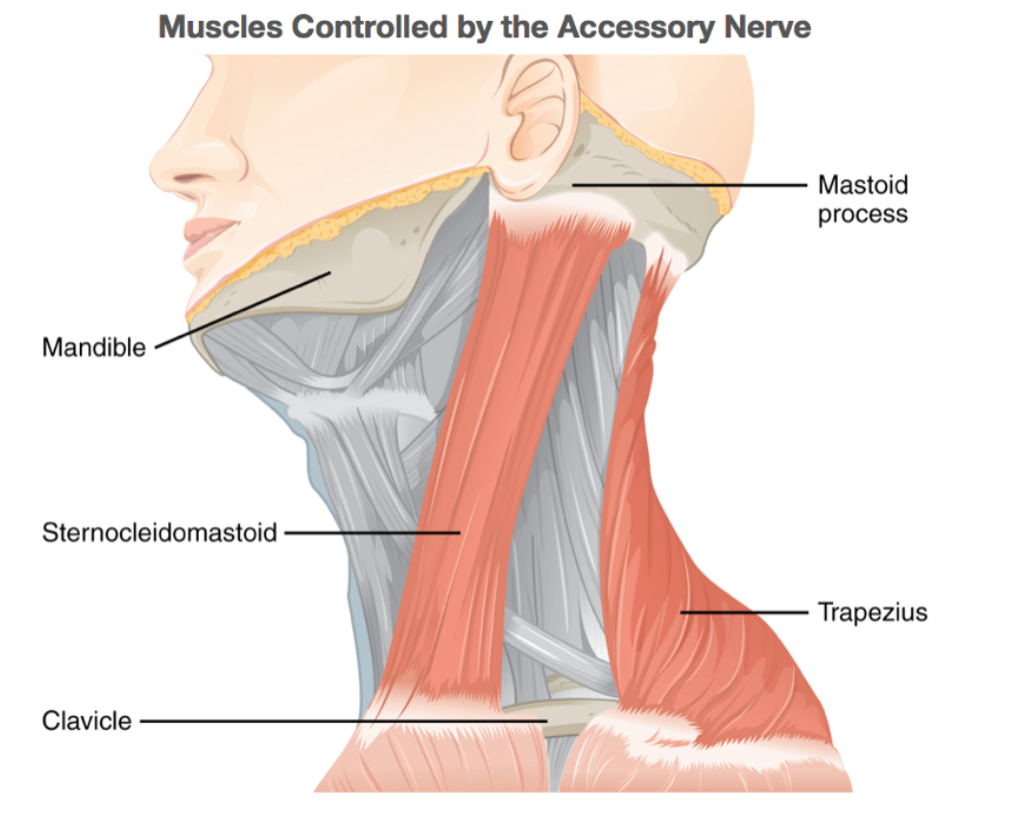
Cranial Nerve XI. Spinal Accessory Nerve (Motor)
The eleventh cranial nerve supplies some motor fibers to the muscles of the larynx and pharynx via the pharyngeal plexus (C.N. IX-X-XI), but its principal distribution is motor to the sternocleidomastoid and trapezius muscles (Fig. 6). The sternocleidomastoid turns the head to the opposite side, and the trapezius muscle elevates the shoulder on the same side. Function of cranial nerve XI is easily determined by checking for bilateral muscle resistance.
Cranial Nerve XII. Hypoglossal Nerve (Motor)
The hypoglossal nerve supplies motor fibers to muscles of the tongue. Muscles in the right half of the tongue are supplied by the right hypoglossal nerve, and muscles in the left half are supplied by the left hypoglossal nerve.
To determine hypoglossal nerve function, one would assess the subject’s speech by asking the subject to read aloud. Movement of the tongue is important in forming the vowel and consonant sounds of speech.
Additionally, a practitioner may ask the subject to protrude his or her tongue in the midline to check for deviation of the tongue tip to the right or left and for atrophy of muscle in the right or left half of the tongue. Normally the tip of the protruded tongue will not deviate from the midline and the tongue will appear symmetrical. A lesion of the hypoglossal nerve will cause the protruded tongue to deviate toward the affected side, and the appearance of the tongue will be asymmetrical owing to atrophy of muscle on the affected side. Often, fasciculations (brief, spontaneous contractions) of the tongue muscle occur on the affected side, indicative of motor neuron damage.
Laboratory Methods
Exercises
This laboratory focuses on the standard clinical techniques for the assessment of the cranial nerves.
IMPORTANT: Have your lab report available during the assessment to keep track of test results.
Olfactory nerve (CN I)
The olfactory nerve is a pure sensory cranial nerve that transmits olfactory information to the brain.
Materials: Vials containing the following: vanilla extract, ground coffee, ammonia, and a small metric ruler
Procedure:
- Have your lab partner close their eyes and block one nostril by occluding it with their finger.
- Place the substance vial approximately 10 centimeters below the unobstructed nostril. Ask them to inhale normally and identify the scent.
- Recap each vial before opening the next scent.
- Record their answer on the lab worksheet.
- Repeat procedure with all vials, alternating the nostril tested until both nostrils have been tested using all scents.
Optic nerve (CN II)
The optic nerve is a sensory cranial nerve, which carries visual information to the brain.
Materials: Snellen eye chart and a pen (or pencil)
Procedure: Examination of the optic nerve involves a determination of visual acuity and peripheral vision.
Visual acuity: Acuity is the sharpness of a visual image. Use the Snellen eye chart located on the lab wall to perform this test. Record your observations on the lab worksheet.
- Have the subject stand 20 feet (6.1 m) away from and facing the chart.
- Have the subject cover one eye and read the letters on the chart you point to for them, starting with the top line and working to the bottom.
- Note the lowest row of letters that can be read accurately.
- Record the number of that row in the worksheet (use the bottom number in the ratio printed to the left of the row of letters). This number is the farthest distance (in feet) that a person with normal acuity can see the letters in that row.
Example
- If a subject has 20-20 vision, that subject can see at 20 feet what a person with normal vision can see at 20 feet. If the subject’s vision is 20-40, the subject sees at 20 feet what a normal subject can see at 40 feet.
- Test both eyes and record the numbers; if the subject wears glasses, you can try the chart with and without glasses (make sure to note in your worksheet whether the subject wore glasses or not during the test).
Peripheral vision
This test assesses peripheral vision:
- Have your lab partner sit directly in front of you at the same eye level height and at a distance of about 2 feet.
- Have them cover their right eye and look directly at you with their left eye. Make sure they continue to stare directly ahead during this procedure.
- To perform stationary testing:
- The examiner closes his or her eye directly opposite the patient’s closed eye and holds up a certain number of fingers peripherally, equidistant between their self and the patient.
- The patient is asked to correctly identify the number of fingers.
- All 4 quadrants (upper and lower, temporal and nasal) should be tested (see figure below).
- Repeat with the other eye.
- Record whether the patient correctly identified the number in each quadrant on the lab worksheet.

Oculomotor (CN III)
Six extrinsic eye muscles are responsible for eyeball movements. Three cranial nerves control these muscles. Four of these six muscles are controlled by the oculomotor nerve, which are the superior, inferior and medial recti and the inferior oblique muscles.
Materials: Each pair of students should have: Penlight, pen or pencil, metric ruler
Procedure to test for motor functions:
- Stand directly in front of the student to be tested.
- Ask them to stare directly ahead.
- Have the student follow with their eyes as you trace the letter H in space.
- Look for smooth coordinated movement with both eyes.
- Record your observations in the lab worksheet.
The oculomotor nerve controls the levator palpebrae superioris muscle that raises the upper eyelid.
- Ask your lab partner to stare directly ahead.
- Check the position of each eyelid. Are they symmetrical?
- Normally about one third of the iris of the eye should be covered by the eyelid.
- Record your observations on the worksheet.
The oculomotor nerve also carries parasympathetic fibers to control the sphincter pupillae. Activation of this smooth muscle causes pupil constriction. The ciliary muscle also receives parasympathetic fibers via the oculomotor nerve. This muscle is responsible for lens accommodation for close vision.
Procedure to test for pupillary constriction:
- As your lab partner is looking directly ahead look to see if both pupils are the same size.
- Are they round or oval?
- Are they facing forward?
- To maximize results from the pupillary constriction test, you may conduct the test in a dark lab, as long as you can still see the pupils of the subject’s eyes.
- Have your lab partner focus on an object in the distance straight ahead.
- Hold the penlight about 20 centimeters to the side of the Right eye and direct the light toward the pupil.
- Did the pupil constrict?
- Repeat shining the light on the Right eye and check to see if this results in the same pupillary response in the Left eye (consensual response).
- Repeat this procedure by shining the light onto the Left eye.
- Record your observations.
Procedure to test for accommodation:
- Have your lab partner stare straight ahead at a distant object.
- Take a pencil and place it about 1 meter in front of your lab partner’s gaze.
- Have your lab partner follow the pencil as you move the pencil to about 3 centimeters in front of their nose.
- Look for convergence of the eyes and pupillary constriction as the subject follows the path of the moving pencil.
- Record your observations.
Trochlear nerve (CN IV)
The trochlear nerve is a pure motor nerve, which supplies one of the six extrinsic eye muscles, the superior oblique. The action of this muscle is to bring the downward and inward.
Procedure to test for motor function:
- Have your lab partner look down at the tip of their nose.
- Observe the movement in both eyes.
- Is the movement symmetrical and smooth?
- Record your observations.
Trigeminal nerve (CN V)
The trigeminal has both motor and sensory components. The motor fibers control the muscles of mastication and the sensory fibers convey the sensations of pain, touch, temperature and pressure from the face, eyes, gums, oral and nasal mucosa, teeth and the anterior two thirds of the tongue. There are three major divisions of the trigeminal nerve: the ophthalmic, maxillary, and mandibular.
Materials: Each student should have: cotton ball (1 per student), tongue depressor (please do not throw away the tongue depressor: each student should keep their own tongue depressor for this and other portions of the clinical exam).
Procedure to test motor functions of the trigeminal nerve:
- Ask your lab partner to clench their teeth several times.
- While your lab partner is clenching their teeth, palpate the temporalis muscle on each side of the head.
- Is the contraction of equal strength on each side?
- Test the strength of masseter muscles using the same technique.
- The masseter can be palpated just above and to the front of the angle of the lower jaw.
- Contractions should be symmetrical and equal.
- Ask your lab partner to bite down on a tongue depressor on the right side.
- Try and pull the tongue depressor out.
- Repeat this procedure on the opposite side
- Record your observations.
Procedure to test sensory functions of trigeminal nerve:
- Three divisions of the trigeminal nerve will be tested for sensory function.
- With your lab partner’s eyes closed take a cotton ball and touch the skin lightly in several different locations.
- To test the ophthalmic division(V1 ) use described procedures on the forehead just above the glabella, slightly to the left and slightly to the right.
- The maxillary division(V2 ) is tested on the skin of the buccal region on the left side and then on the right side.
- The mandibular division (V3 ) is tested on the mental region slightly to the left side then slightly to the right side. See figures below.
- Ask them to indicate if they feel the touch.
- Record your observations.

Abducens nerve (CN VI)
The abducens nerve is a motor nerve, which supplies one of the six extrinsic eye muscles, the lateral rectus. The action of this muscle is to abduct the eye (move it laterally)
Procedure to test for motor function:
- Have your lab partner stare straight ahead
- Then move the eyes to the right and then to the left.
- Observe the movement in both eyes.
- Is the movement symmetrical and smooth?
- Record your observations.
Facial nerve (CN VII)
The facial nerve is a mixed cranial nerve that also has parasympathetic fibers associated with it. The motor component controls the muscles of facial expression. The sensory portion conveys taste information from the taste buds located on the anterior two-thirds of the tongue. Parasympathetic fibers innervate the submandibular and sublingual salivary glands, the lacrimal (tear) glands of the eyes, and nasal and palatine glands.
Procedure to test motor component of the facial nerve:
- Ask you lab partner to:
- smile
- lift their eyebrows
- frown
- close their eyes tightly
- pucker their lips
- wrinkle the forehead
Look for symmetry of the muscles on both sides of the face.
Materials: Each pair of students should have: natural sugar solution, salt solution, 8 disposable pipets, 2 10ml beakers per student
Procedure to test for sensory function of the facial nerve:
Notes: During this procedure, never touch the pipet to the tongue.
Pour 5ml of each solution into a beaker and use a new pipette each time you take solution from the beaker.
- Ask your lab partner to close their eyes and protrude their tongue.
- Ask your partner to raise their hand when they taste a solution.
- Ask your partner what solution they detected.
- Place a few drops of the sugar solution on the anterior half of the tongue on the right side.
- Place a few drops of the sugar solution on the anterior half of the tongue on the left side.
- Place a few drops of the salt solution on the anterior half of the tongue on the right side.
- Place a few drops of the salt solution on the anterior half of the tongue on the left side
- Record your observations.
Vestibulocochlear nerve (CN VIII)
The vestibulocochlear nerve is a sensory nerve that conveys sound information and balance (equilibrium).
Materials: tuning fork
1. Rinne Test.
This test is used to identify impairment in the conduction of sound though the external and middle ear, to the sensory areas of the inner ear. It is done by comparing air conduction with bone conduction.
- Strike a tuning fork against the palm of your hand (never strike the tuning fork against a hard surface)
- Place its handle on the subject’s mastoid process.
- When the subject no longer hears the sound, move the prongs (they should still be vibrating) to the opening of the external auditory meatus (be careful not to touch it). Normally, the hum will be heard again; if not, conduction impairment is suspected.
- Record your results in the worksheet.
- Repeat on the other side of the head.
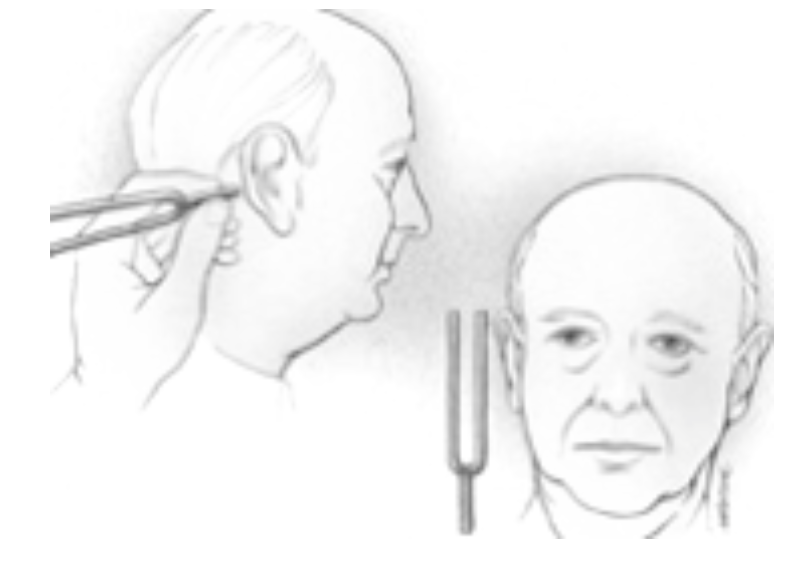
2. Weber Test.
This is another test used to identify defects in conduction. The Weber Test is only useful if there is an asymmetrical hearing loss. If hearing is symmetrical, the patient perceives the sound in the middle of their head.
- Strike a tuning fork against the palm of your hand and place the handle against the middle of the subject’s forehead.
- Ask the subject on which side, if any, the sound seems louder.
- Record your results.

3. Romberg Test.
The Romberg test evaluates a subject’s ability to maintain balance and equilibrium, using proprioceptors and the vestibular apparatus (utricle and saccule) without the aid of vision. Impairment of the dorsal white column of the spinal cord (transmits information from proprioceptors to the brain), the vestibular apparatus, the basal ganglia or the cerebellum can be detected during this test. Note: If equilibrium impairment exists, the subject may topple over. Have at least one person standing by to stabilize the subject if this happens.
Procedure:
- Have the subject stand near the wall with the tape on it.
- Have the student stand so you can see at least one set of lines on each side the subject’s body, parallel to it.
- Have the subject stand in place, feet together, with their eyes open, staring straight ahead for 30 seconds. Note any swaying movements, using the lines on the board as a reference.
- Repeat the test, this time with the subject’s eyes closed. Again, note the degree of side-to-side movement.
- Repeat the test again (steps in bold above) with the subject standing perpendicular to the wall (the left shoulder is near the wall, but not touching it)
4. Auditory Frequency Test.
Determine the subject’s range of hearing by listening to a spectrum of sounds from YouTube. Use the headphones, but please make sure the volume is turned to 30 (right side lower task bar), or higher frequency sounds will be unpleasant.
Use the spectrum to determine the low and high frequency values for your hearing.
Put on the headphones. Open the “Week5_20Hz to 20 kHz” file from the P-drive. Click pause to record when you start hearing and when you stop hearing the sounds.
Glossopharyngeal nerve (CN IX) and Vagus nerve (CN X)
The glossopharyngeal nerve is a mixed nerve that also supplies parasympathetic innervation to the parotid salivary glands in the head. The motor fibers of the glossopharyngeal supply skeletal muscles of the pharynx, larynx, and soft palate. Sensory fibers convey taste information from taste buds on the posterior one third of the tongue. Sensory information concerning blood pressure and blood chemistry is also found in this cranial nerve.
The vagus is a mixed nerve with parasympathetic fibers. The parasympathetic fibers innervate structures in the neck, thorax and into the abdomen. The motor fibers of the vagus supply skeletal muscles of the pharynx and larynx. Some taste buds are found around the epiglottis. Sensory information from these taste buds is conveyed by the vagus nerve.
Many functions of the glossopharyngeal and vagus nerves overlap therefore typically; these two nerves are tested together.
Materials: Tongue depressor, penlight, soy sauce solution, 8 disposable pipets
Procedure:
- Ask your lab partner to open their mouth and say “ahh”.
- Hold down the tongue with the depressor and using the pen light look at the position of the soft palate and uvula before and during the test.
- During phonation (when they are saying “ahh”) the uvula should rise in the midline position.
- Check vocalization by asking them to read a sentence from the lab instructions. Is there any unexplained hoarseness?
- Ask your lab partner to swallow. Do they have any difficulties?
- Record your observations
Glossopharyngeal nerve (CN IX) and Vagus nerve (CN X)
Notes on procedure to test for sensory function of the CN IX & CN X nerve:
During this procedure, never touch the pipet to the tongue
Use a new pipette each time you take solution from the beaker
Pour 5ml soy sauce solution into a beaker.
- Ask your lab partner to close their eyes and protrude their tongue.
- Place a few drops of the soy sauce on the posterior half of the tongue on the right side.
- Place a few drops of the soy sauce on the posterior half of the tongue on the left side.
- Have your lab partner raise their hand when they taste the solution.
- Have them report the taste of the solution that was placed on their tongue.
- Record your observations.
Accessory nerve (CN XI)
The accessory nerve has motor function, and it transmits motor fibers to the sternocleidomastoid and trapezius muscles.
Procedure:
- Have your lab partner stare straight ahead.
- Place your hand on their right cheek.
- Have them turn their head to the right against the resistance of your hand.
- Repeat this procedure on the left side.
- For each side, assess the strength of the muscle contraction using a scale of 1 (very weak) to 4 (very strong).
- Observe whether there are any differences in the strength of the muscle contraction between the two sides.
- Record your observations.
- Have your lab partner sit up straight on the lab stool.
- Place your hands on their shoulders.
- Ask them to shrug their shoulders against resistance.
- Assess the strength of the contraction using the scale mentioned above.
- Compare the strength of the contraction between the two sides
- Record your observations.
Hypoglossal nerve (CN XII)
The hypoglossal nerve is a motor nerve to the intrinsic muscles of the tongue.
Procedure:
- Ask your lab partner to protrude their tongue in the midline.
- Look for any deviations to the right or left.
- The tongue should not deviate from the midline.
- Record your observations.
Online Resources:
- UC San Diego Practical Guide to Clinical Medicine, Cranial Nerves
- The Cranial Nerve Practice Exam, OpenStax
- Cranial Nerves Lab [download doc]
- OpenStax College. (2013). Anatomy & physiology. Houston, TX: OpenStax CNX. Retrieved from http://cnx.org/content/col11496/latest/


