1.3: Integumentary System
- Page ID
- 64952
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the integumentary system
- Identify meanings of key word components of the integumentary system
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the integumentary system
- Use terms related to the integumentary system
- Use terms related to the diseases and disorders of the integumentary system
Integumentary System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Integumentary System.
Introduction to the Integumentary System
The integumentary system refers to the skin and its accessory structures. In the adult human body, the skin makes up about 16 percent of body weight and covers an area of 16-21 ft2.
In fact, the skin and accessory structures are the largest organ system in the human body. The skin protects your inner organs and it is in need of daily care and protection to maintain its health.
Watch this video:
Media 3.1. The science of skin – Emma Bryce [Video]. Copyright 2018 by Ted-Ed.
Practice integumentary system medical terms.
Anatomy (Structures) of the Integumentary System
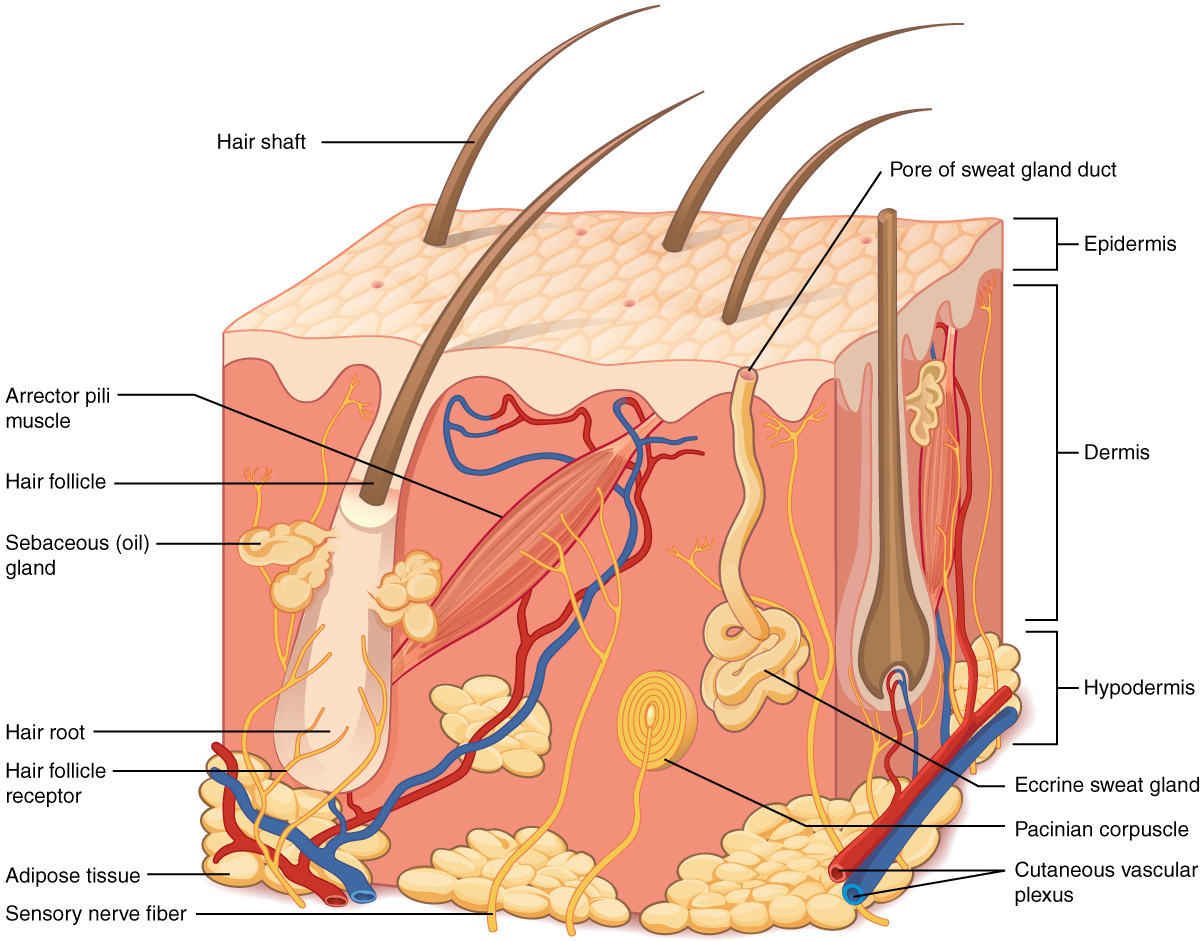
The skin and its accessory structures make up the integumentary system, which provides the body with overall protection. The skin is made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue. The deeper layer of skin is well vascularized. It also has numerous sensory, and autonomic and sympathetic nerve fibers ensuring communication to and from the brain.
The skin is composed of two main layers:
- The epidermis
- The dermis
- Beneath the dermis lies the hypodermis
Concept Check
- On the diagram above find the two layers of the skin; epidermis and dermis.
- The literal breakdown for hypodermis is below the dermis. On the diagram above where can you locate it?
- Can you find a hair follicle, hair root and hair shaft?
- Keep reading to find out what the arrector pilli muscle does when you are frightened.
Epidermis
The epidermis is composed of keratinized, stratified squamous epithelium. It is made of four or five layers of epithelial cells, depending on its location in the body. It is avascular.
The cells in all of the layers except the stratum basale are called keratinocytes. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers.
Dermis
The dermis contains blood and lymph vessels, nerves, and other structures, such as hair follicles and sweat glands. The dermis is made of two layers (papillary layer and reticular layer) of connective tissue that compose an interconnected mesh of elastin and collagenous fibers, produced by fibroblasts (see Figure 3.2).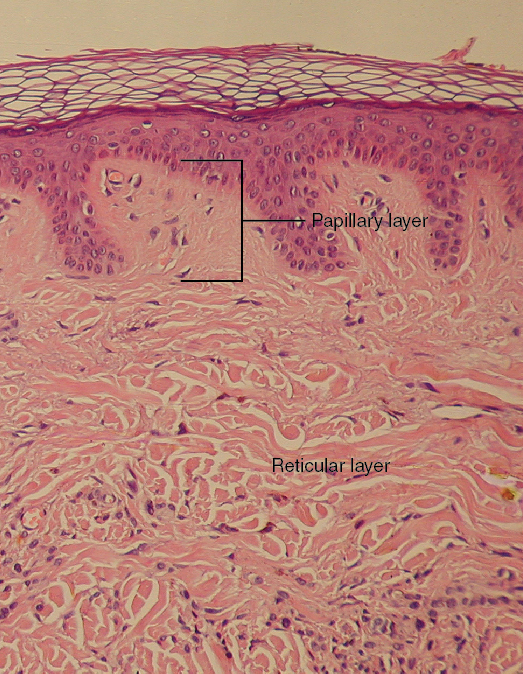
Papillary Layer
The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibers of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae (see Figure 3.2). Within the papillary layer are fibroblasts, a small number adipocytes, and an abundance of small blood vessels. In addition, the papillary layer contains phagocytes, that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibers, and Meissner corpuscles.
Reticular Layer
Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularized and has a rich sensory and sympathetic nerve supply. The reticular layer appears reticulated due to a tight meshwork of fibers. Elastin fibers provide some elasticity to the skin, enabling movement. Collagen fibers provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. In addition, collagen binds water to keep the skin hydrated. Collagen injections and Retin-A creams help restore skin turgor by either introducing collagen externally or stimulating blood flow and repair of the dermis, respectively.
Hypodermis
The hypodermis serves to connect the skin to the underlying fascia of the bones and muscles. It is not strictly a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and [pb_glossary id="1697"]adipose[/pb_glossary] tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
Practice labeling the layers of the skin.
Physiology (Function) of the Integumentary System
The skin and accessory structures perform a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing vitamin D. The underlying hypodermis has important roles in storing fats, forming a “cushion” over underlying structures, and providing insulation from cold temperatures.
Protection
The skin protects the body from wind, water, and UV sunlight. It acts as a protective barrier against water loss and it also is the first line of defense against abrasive activity such as grit, microbes, or harmful chemicals. Sweat excreted from sweat glands deters microbes from over-colonizing the skin surface.
Sensory Function
The skin acts as a sense organ because the epidermis, dermis, and the hypodermis contain specialized sensory nerve structures that detect touch, surface temperature, and pain. These receptors are more concentrated on the tips of the fingers, which are most sensitive to touch, especially the Meissner corpuscle, which responds to light touch, and the Pacinian corpuscle , which responds to vibration. Merkel cells, seen scattered in the stratum basale, are also touch receptors. In addition to these specialized receptors, there are sensory nerves connected to each hair follicle, pain and temperature receptors scattered throughout the skin, and motor nerves innervate the arrector pili muscles and glands. This rich innervation helps us sense our environment and react accordingly,
Thermoregulation
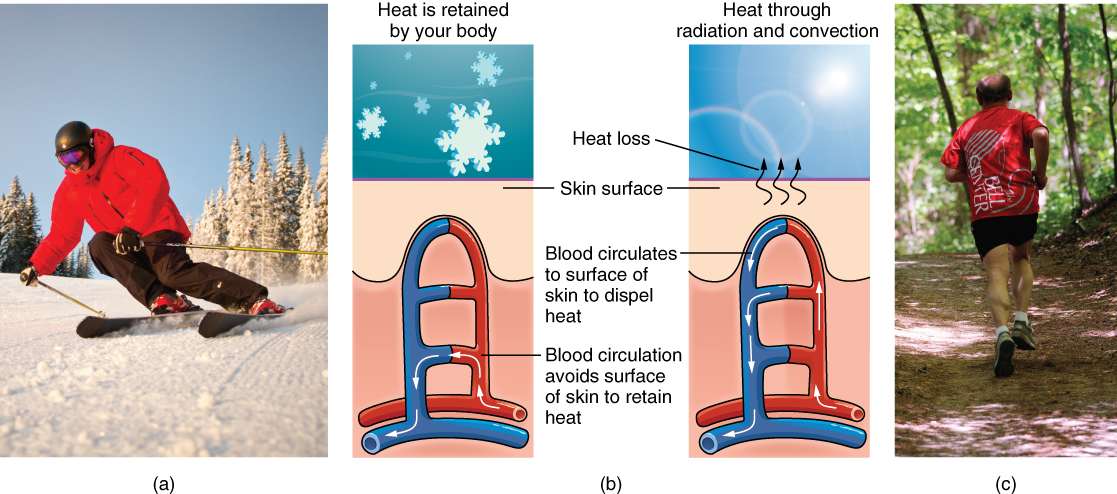
The integumentary system helps regulate body temperature through its tight association with the sympathetic nervous system. The sympathetic nervous system is continuously monitoring body temperature and initiating appropriate motor responses.
- When the body becomes warm sweat glands, accessory structures to the skin, secrete water, salt, and other substances to cool the body.
- Even when the body does not appear to be noticeably sweating, approximately 500 mL of sweat are secreted a day.
- If the body becomes excessively warm due to high temperatures, vigorous activity, or a combination of the two, sweat glands will be stimulated by the sympathetic nervous system to produce large amounts of sweat.
- When the sweat evaporates from the skin surface, the body is cooled as body heat is dissipated.
- In addition to sweating, arterioles in the dermis dilate so that excess heat carried by the blood can dissipate through the skin and into the surrounding environment.
- This accounts for the skin redness that many people experience when exercising.
- When body temperatures drop, the arterioles constrict to minimize heat loss, particularly in the ends of the digits and tip of the nose.
- This reduced circulation can result in the skin taking on a whitish hue.
- Although the temperature of the skin drops as a result, passive heat loss is prevented, and internal organs and structures remain warm.
- If the temperature of the skin drops too much (such as environmental temperatures below freezing), the conservation of body core heat can result frostbite .
Concept Check
Can you describe the thermoregulation process between the integumentary system and the sympathetic system?
- When body temperature is too warm.
- When body temperature is too cold.
Vitamin D Synthesis
The epidermal layer of human skin synthesizes Vitamin D when exposed to UV radiation. In the presence of sunlight, a form of Vitamin D3 called cholecalciferol is synthesized from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys.
- Vitamin D is essential for normal absorption of calcium and phosphorous, which are required for healthy bones.
- The absence of sun exposure can lead to a lack of vitamin D in the body, in children this can cause rickets. Vitamin D deficiency in elderly individuals may lead to osteomalacia.
- In present day society, Vitamin D is added as a supplement to many foods, including milk and orange juice, compensating for the need for sun exposure. In addition to its essential role in bone health, Vitamin D is essential for general immunity against bacterial, viral, and fungal infections.
Watch this video:
Media 3.2. The Integumentary System, Part 2 – Skin Deeper: Crash Course A&P #7 [Online video]. Copyright 2015 by CrashCourse.Media 3.2. The Integumentary System, Part 2 – Skin Deeper: Crash Course A&P #7 [Online video]. Copyright 2015 by CrashCourse.
Accessory Structures
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. These structures embryologically originate from the epidermis and can extend down through the dermis into the hypodermis.
Hair
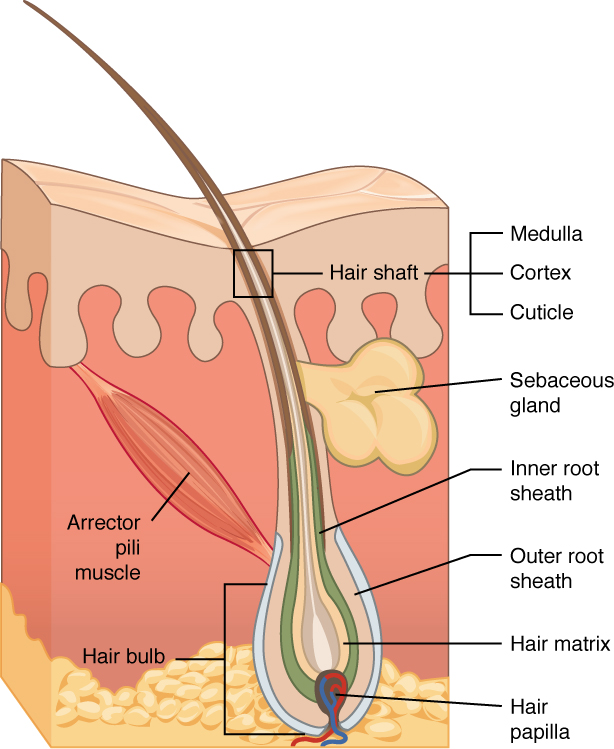
Hair is a keratinous filament growing out of the epidermis. It is primarily made of dead, keratinized cells. Strands of hair originate in an epidermal penetration of the dermis called the hair follicle. The hair shaft is the part of the hair not anchored to the follicle, and much of this is exposed at the skin’s surface. The rest of the hair, which is anchored in the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the hair bulb, and includes a layer of mitotically active basal cells called the hair matrix. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis (see Figure 3.4).
Hair Function
Hair serves a variety of functions, including protection, sensory input, thermoregulation, and communication. For example:
- Hair on the head protects the skull from the sun.
- Hair in the nose and ears, and around the eyes (eyelashes) defends the body by trapping and excluding dust particles that may contain allergens and microbes.
- Hair of the eyebrows prevents sweat and other particles from dripping into and bothering the eyes.
Hair also has a sensory function due to sensory innervation by a hair root plexus surrounding the base of each hair follicle. Hair is extremely sensitive to air movement or other disturbances in the environment, much more so than the skin surface. This feature is also useful for the detection of the presence of insects or other potentially damaging substances on the skin surface.
Each hair root is connected to a smooth muscle called the arrector pili that contracts in response to nerve signals from the sympathetic nervous system, making the external hair shaft “stand up.” The primary purpose for this is to trap a layer of air to add insulation. This is visible in humans as goose bumps and even more obvious in animals, such as when a frightened cat raises its fur. Of course, this is much more obvious in organisms with a heavier coat than most humans, such as dogs and cats.
Hair Growth, Loss and Color
Hair grows and is eventually shed and replaced by new hair. Hair typically grows at the rate of 0.3 mm per day. On average, 50 hairs are lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced and can happen due to hormonal or dietary changes. Hair loss can also result from the aging process, or the influence of hormones. Similar to the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair papilla. Different hair color results from differences in the type of melanin. As a person ages, the melanin production decreases, and hair tends to lose its color and becomes gray and/or white.
Nails
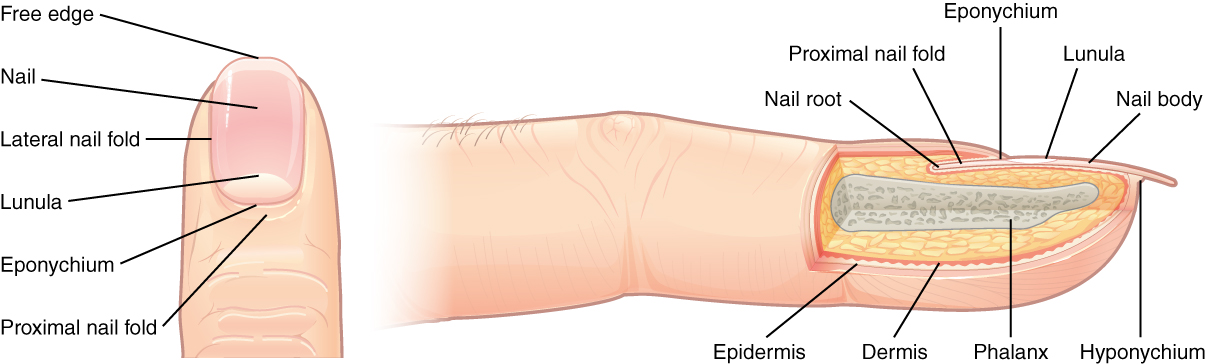
The nail bed is a specialized structure of the epidermis that is found at the tips of our fingers and toes. The nail body is formed on the nail bed, and protects the tips of our fingers and toes as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress (see Figure 3.5). The nail body forms a back-support for picking up small objects with the fingers. The nail body is composed of densely packed dead keratinocytes.
The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root, which has a matrix of proliferating cells from the stratum basale that enables the nail to grow continuously. The lateral nail fold overlaps the nail on the sides, helping to anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium.
The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the lunula (the “little moon”). The area beneath the free edge of the nail, furthest from the cuticle, is called the hyponychium. It consists of a thickened layer of stratum corneum.
Sweat Glands
Sudoriferous Glands
When the body becomes warm, sudoriferous glands produce sweat to cool the body. Sweat glands develop from epidermal projections into the dermis and are classified as merocrine glands; that is, the secretions are excreted by exocytosis through a duct without affecting the cells of the gland. There are two types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is type of gland that produces a hypotonic sweat for thermoregulation as described previously. These glands are found all over the skin’s surface, but are especially abundant on the palms of the hand, the soles of the feet, and the forehead (Figure 3.6). They are coiled glands lying deep in the dermis, with the duct rising up to a pore on the skin surface, where the sweat is released. This type of sweat, released by exocytosis, is hypotonic and composed mostly of water, with some salt, antibodies, traces of metabolic waste, and dermicidin, an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis .
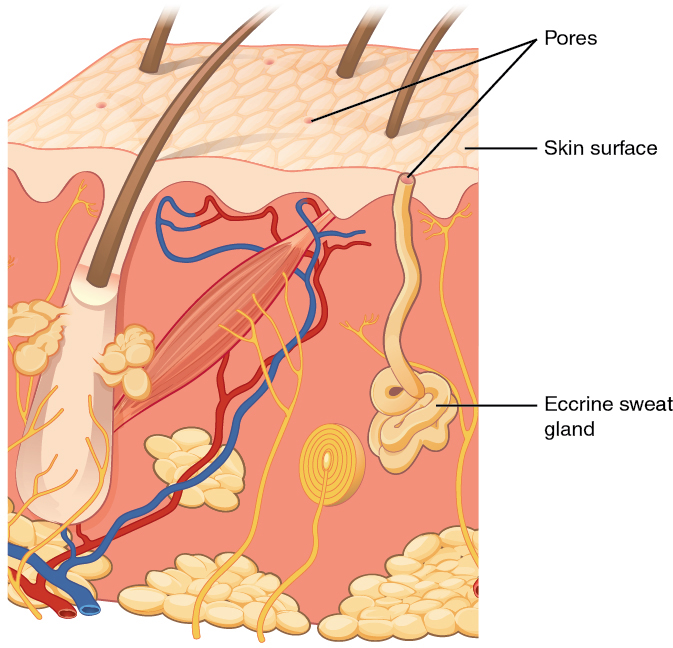
An apocrine sweat gland is usually associated with hair follicles in densely hairy areas, such as armpits and genital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and subject to bacterial decomposition and subsequent smell. The release of this sweat is under both nervous and hormonal control, and plays a role in the poorly understood human pheromone response. Most commercial antiperspirants use an aluminum-based compound as their primary active ingredient to stop sweat. When the antiperspirant enters the sweat gland duct, the aluminum-based compounds precipitate due to a change in pH and form a physical block in the duct, which prevents sweat from coming out of the pore.
Sebaceous Glands
A sebaceous gland is a type of oil gland that is found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles. They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties, and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Words not Easily Broken into Word Parts
Common Integumentary System Abbreviations
Many terms and phrases related to the integumentary system are abbreviated. Learn these common abbreviations by expanding the list below.
Changes Due to Aging
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength (see Figure 3.7). In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the elasticity and resilience of the skin, exhibits a reduced ability to regenerate, which leads to slower wound healing. The hypodermis, with its fat stores, loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin.

The accessory structures also have lowered activity, generating thinner hair and nails, and reduced amounts of sebum and sweat. A reduced sweating ability can cause some elderly to be intolerant to extreme heat. Other cells in the skin, such as melanocytes and dendritic cells, also become less active, leading to a paler skin tone and lowered immunity. Wrinkling of the skin occurs due to breakdown of its structure, which results from decreased collagen and elastin production in the dermis, weakening of muscles lying under the skin, and the inability of the skin to retain adequate moisture.
Disease and Disorders
The integumentary system is susceptible to a variety of diseases, disorders, and injuries. These range from annoying but relatively benign bacterial or fungal infections that are categorized as disorders, to skin cancer and severe burns, which can be fatal. In this section, you will learn several of the most common skin conditions.
One of the most talked about diseases is skin cancer. Most cancers are identified by the organ or tissue in which the cancer originates. One common form of cancer is skin cancer.
In general, cancers result from an accumulation of DNA mutations. These mutations can result in cell populations that do not die when they should and uncontrolled cell proliferation that leads to tumors. Although many tumors are benign, some metastasize. Cancers are characterized by their ability to metastasize.
Sun Damage
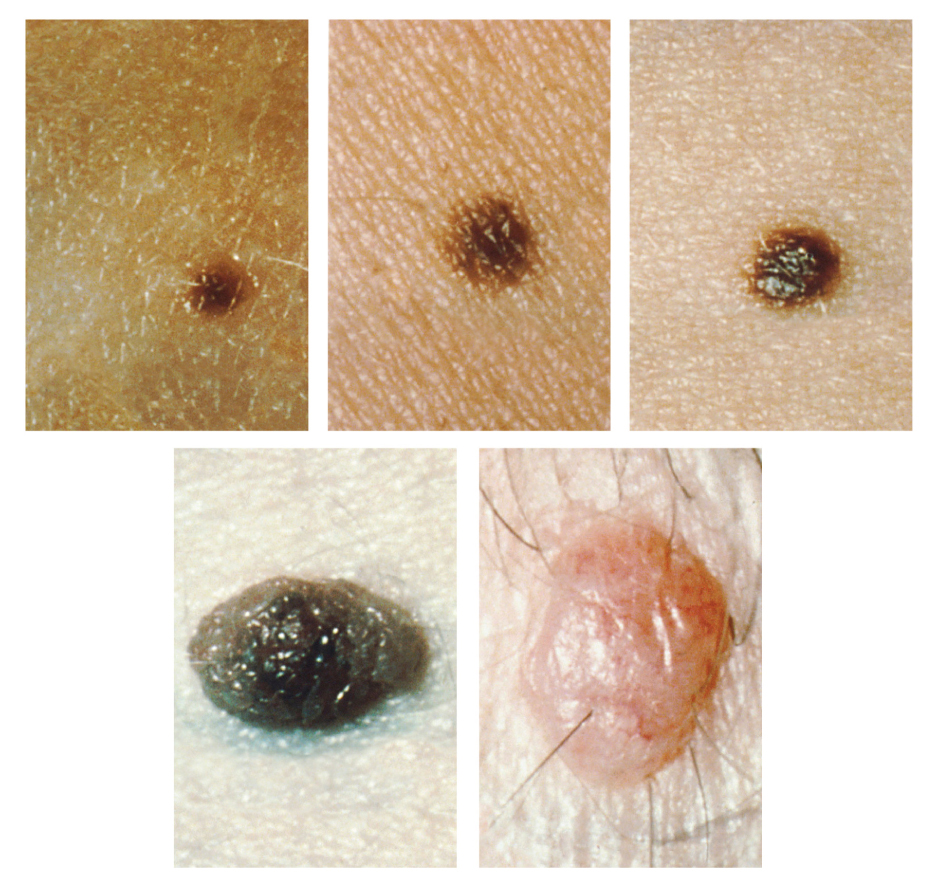
It requires about 10 days after initial sun exposure for melanin synthesis to peak, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Dark-skinned individuals can also get sunburns, but are more protected than are pale-skinned individuals. Too much sun exposure can eventually lead to wrinkling due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer. When there is an irregular accumulation of melanocytes in the skin, freckles appear. Moles are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (see Figure 3.8).
Basal Cell Carcinoma (BCC)
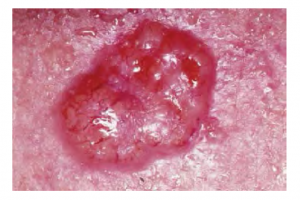
Basal cell carcinoma is a form of cancer that affects the mitotically active stem cells in the stratum basale of the epidermis. It is the most common of all cancers that occur in the United States and is frequently found on the head, neck, arms, and back, which are are as that are most susceptible to long-term sun exposure. Although UV rays are the main culprit, exposure to other agents, such as radiation and arsenic, can also lead to this type of cancer. Wounds on the skin due to open sores, tattoos, burns, etc. may be predisposing factors. Basal cell carcinomas start in the stratum basale and usually spread along this boundary. At some point, they begin to grow toward the surface and become an uneven patch, bump, growth, or scar on the skin surface (see Figure 3.9). Like most cancers, basal cell carcinomas respond best to treatment when caught early. Treatment options include surgery, freezing (cryosurgery), and topical ointments.
Squamous Cell Carcinoma (SCC)

Squamous cell carcinoma is a cancer that affects the keratinocytes of the stratum spinosum and presents as lesions commonly found on the scalp, ears, and hands (see Figure 3.10). It is the second most common skin cancer. The American Cancer Society reports that two of 10 skin cancers are squamous cell carcinomas, and it is more aggressive than basal cell carcinoma. If not removed, these carcinomas can metastasize. Surgery and radiation are used to cure squamous cell carcinoma.
Melanoma
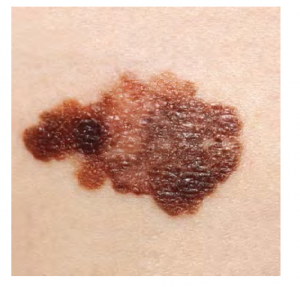
A melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the pigment-producing cells in the epidermis. Typically, a melanoma develops from a mole. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface (see Figure 3.11). Treatment typically involves surgical excision and immunotherapy.
ABCDE for Early Diagnosis
Doctors often give their patients the following ABCDE mnemonic to help with the diagnosis of early-stage melanoma (see Fig 3.12). If you observe a mole on your body displaying these signs, consult a doctor.
- Asymmetry – the two sides are not symmetrical
- Borders – the edges are irregular in shape
- Color – the color is varied shades of brown or black
- Diameter – it is larger than a pencil eraser
- Evolving – its shape has changed
 Fig 3.12 The ABC’s of early diagnosis. Example of abnormal moles. (credit: the National Cancer Institute, moles C&D, n.d.). Mole A from Betts, et al., 2021. Licensed under CC BY 4.0.
Fig 3.12 The ABC’s of early diagnosis. Example of abnormal moles. (credit: the National Cancer Institute, moles C&D, n.d.). Mole A from Betts, et al., 2021. Licensed under CC BY 4.0.Some specialists cite the following additional signs for the most serious form, nodular melanoma:
Elevated – it is raised on the skin surface
Firm – it feels hard to the touch
Growing – it is getting larger
Albinism
Albinism is a genetic disorder that affects (completely or partially) the coloring of skin, hair, and eyes. This is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Recall that melanin helps protect the skin from the harmful effects of UV radiation. Individuals with albinism tend to need more protection from UV radiation, as they are more prone to sunburns and skin cancer. They also tend to be more sensitive to light and have vision problems due to the lack of pigmentation on the retinal wall (Betts, et al., 2021)
Treatment of this disorder usually involves addressing the symptoms, such as limiting UV light exposure to the skin and eyes. In vitiligo, the melanocytes in certain areas lose their ability to produce melanin, possibly due to an autoimmune reaction. This leads to a loss of color in patches (see Figure 3.13). Neither albinism nor vitiligo directly affects the lifespan of an individual (Betts, et al., 2021)

Changes in Skin Coloration
Other changes in the appearance of skin coloration can be indicative of diseases associated with other body systems.
- Liver disease or liver cancer can cause the accumulation of bile and the yellow pigment bilirubin, leading to xanthoderma or jaundice.
- Tumors of the pituitary gland can result in the secretion of large amounts of melanocyte-stimulating hormone (MSH), which results in a darkening of the skin.
- Addison’s disease can stimulate the release of excess amounts of adrenocorticotropic hormone (ACTH), which can give the skin a deep bronze color
- A sudden drop in oxygenation can affect skin color, causing the skin to initially turn ashen (white).
- A prolonged reduction in oxygen levels, dark red deoxyhemoglobin becomes dominant in the blood, making the skin appear blue, a condition referred to as cyanosis. This happens when the oxygen supply is restricted, as when someone is experiencing difficulty in breathing because of asthma or a heart attack. However, in these cases the effect on skin color has nothing do with the skin’s pigmentation (Betts, et al., 2021)
Skin Disorders
Two common skin disorders are eczema and acne. Eczema is an inflammatory condition and occurs in individuals of all ages. Acne involves the clogging of pores, which can lead to infection and inflammation, and is often seen in adolescents. Other disorders, include seborrheic dermatitis (on the scalp), psoriasis, fungal infections, cold sores, impetigo, scabies, hives, and warts (Betts, et al., 2021).
Eczema

Eczema is an allergic reaction that manifests as dry, itchy patches of skin that resemble rashes (see Figure 3.14). It may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. Symptoms are usually managed with moisturizers, corticosteroid creams, and immunosuppressants (Betts, et al., 2021).
Acne
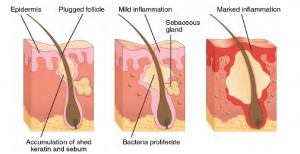
Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands (face and back). It is most common along with the onset of puberty due to associated hormonal changes, but can also occur in infants and continue into adulthood. Hormones, such as androgens, stimulate the release of sebum. An overproduction and accumulation of sebum along with keratin can block hair follicles. This plug is initially white. The sebum, when oxidized by exposure to air, turns black. Acne results from infection by acne-causing bacteria (Propionibacterium and Staphylococcus), which can lead to redness and potential scarring due to the natural wound healing process (see Figure 3.15) (Betts, et al., 2021).
Ringworm
Tinea or dermatophytosis is often referred to as ringworm. Ringworm presents as a circular rash that is itchy and red and can be found on various parts of the body. It is referred to by the location that it is found:
-
- Tinea Pedis – feet or commonly referred to as athlete’s feet
- Tinea Capitis – scalp
- Tinea barbae – beard
- Tinea manuum – hands
- Tinea unguium – Toenails and fingernails also called onychomycosis
- Tinea corporis – Body parts such as arms and legs (Center for Disease Control and Prevention, 2018a)
To learn more about ringworm, visit the Center for Disease Control and Prevention’s web page on fungal infections.
Psoriasis
Psoriasis is a chronic autoimmune disorder that results in patches of thick red skin with the appearance of silvery scales. These patches can be found on elbows, knees, scalp, low back, face, feet, fingernails, toenails and even the mouth. Psoriasis can be confused with other skin disease so a dermatologist is the best physician to diagnosis psoriasis. Treatments may include creams, ointments, ultraviolet light therapy and medication (Center for Disease Control and Prevention, 2018). To learn more, visit the Center for Disease Control and Prevention’s web page on psoriasis.
Injuries
Because the skin is the part of our bodies that meets the world most directly, it is especially vulnerable to injury. Injuries include burns, wounds, as well as scars and calluses. They can be caused by sharp objects, heat, or excessive pressure or friction to the skin (Betts, et al., 2021).Skin injuries set off a healing process that occurs in several overlapping stages.
- The first step to repairing damaged skin is the formation of a blood clot that helps stop the flow of blood and scabs over with time. Many different types of cells are involved in wound repair, especially if the surface area that needs repair is extensive.
- Before the basal stem cells of the stratum basale can recreate the epidermis, fibroblasts mobilize and divide rapidly to repair the damaged tissue by collagen deposition, forming granulation tissue.
- Blood capillaries follow the fibroblasts and help increase blood circulation and oxygen supply to the area.
- Immune cells, such as macrophages, roam the area and engulf any foreign matter to reduce the chance of infection (Betts, et al., 2021).
Burns
A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can lead to a massive loss of fluid. Dehydration, electrolyte imbalance, and renal and circulatory failure follow, which can be fatal. Burn patients are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to the lives of burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of skin (Betts, et al., 2021).
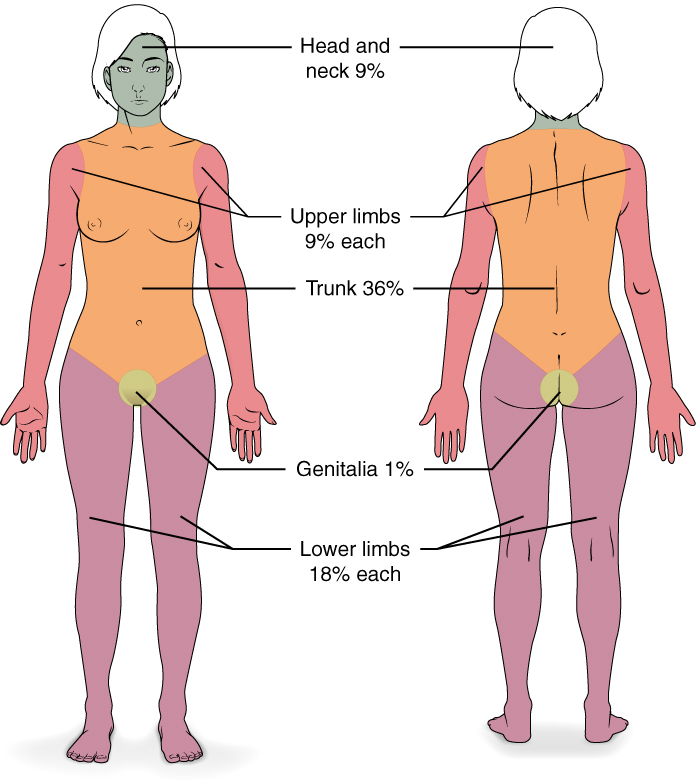
Burn Classification
Burns are sometimes measured in terms of the size of the total surface area affected. This is referred to as the rule of nines, which associates specific anatomical areas with a percentage that is a factor of nine (see Figure 3.16) (Betts, et al., 2021).
Burns are also classified by the degree of their severity.
- A first-degree burn is a superficial burn that affects only the epidermis. Although the skin may be painful and swollen, these burns typically heal on their own within a few days. Mild sunburn fits into the category of a first-degree burn.
- A second-degree burn goes deeper and affects both the epidermis and a portion of the dermis. These burns result in swelling and a painful blistering of the skin. It is important to keep the burn site clean and sterile to prevent infection. If this is done, the burn will heal within several weeks.
- A third-degree burn fully extends into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns that may appear white, red, or black; they require medical attention and will heal slowly without it.
- A fourth-degree burn is even more severe, affecting the underlying muscle and bone.
Oddly, third and fourth-degree burns are usually not as painful because the nerve endings themselves are damaged. Full-thickness burns cannot be repaired by the body, because the local tissues used for repair are damaged and require debridement, or amputation in severe cases, followed by grafting of the skin from an unaffected part of the body, or from skin grown in tissue culture for grafting purposes. Skin grafts are required when the damage from trauma or infection cannot be closed with sutures or staples (Betts et al., 2021).
Scars and Keloids
Most cuts or wounds, with the exception of ones that only scratch the epidermis, lead to scar formation. Scarring occurs in cases in which there is repair of skin damage, but the skin fails to regenerate the original skin structure. Fibroblasts generate scar tissue in the form of collagen, and the bulk of repair is due to the basket-weave pattern generated by collagen fibers and does not result in regeneration of the typical cellular structure of skin. Instead, the tissue is fibrous in nature and does not allow for the regeneration of accessory structures, such as hair follicles, sweat glands, or sebaceous glands (Betts, et al., 2021).
Sometimes, there is an overproduction of scar tissue, because the process of collagen formation does not stop when the wound is healed; this results in a keloid (see Figure 3.17). In contrast, scars that result from acne and chickenpox have a sunken appearance and are called atrophic scars (Betts, et al., 2021).

Scarring of skin after wound healing is a natural process and does not need to be treated further. Application of mineral oil and lotions may reduce the formation of scar tissue. However, modern cosmetic procedures, such as dermabrasion, laser treatments, and filler injections have been invented as remedies for severe scarring. All of these procedures try to reorganize the structure of the epidermis and underlying collagen tissue to make it look more natural (Betts, et al., 2021).
Bedsores and Stretch Marks
Skin and its underlying tissue can be affected by excessive pressure. One example of this is called a bedsore. Bedsores, also called decubitis ulcers, are caused by constant, long-term, unrelieved pressure on certain body parts that are bony, reducing blood flow to the area and leading to necrosis . Bedsores are most common in elderly patients who have debilitating conditions that cause them to be immobile. Most hospitals and long-term care facilities have the practice of turning the patients every few hours to prevent the incidence of bedsores. If left untreated bedsores can be fatal if they become infected (Betts, et al., 2021)
The skin can also be affected by pressure associated with rapid growth. A stretch mark results when the dermis is stretched beyond its limits of elasticity, as the skin stretches to accommodate the excess pressure. Stretch marks usually accompany rapid weight gain during puberty and pregnancy. They initially have a reddish hue, but lighten over time. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen (Betts, et al., 2021). For detailed images of types of bedsores, see Minnesota Hospital Association’s Pressure Ulcer Staging Cards.
Calluses
When you wear shoes that do not fit well and are a constant source of abrasion on your toes, you tend to form a callus at the point of contact. This occurs because the basal stem cells in the stratum basale are triggered to divide more often to increase the thickness of the skin at the point of abrasion to protect the rest of the body from further damage. This is an example of a minor or local injury, and the skin manages to react and treat the problem independent of the rest of the body. Calluses can also form on your fingers if they are subject to constant mechanical stress, such as long periods of writing, playing string instruments, or video games. A corn is a specialized form of callus. Corns form from abrasions on the skin that result from an elliptical-type motion (Betts, et al., 2021).
Medical Terms in Context
Medical Specialties and Procedures Related to the Integumentary System
A dermatologist is a medical doctor with specialized training in treating diseases, disorders and injuries related to the integumentary system and its accessory structures. There are many dermatologic subspecialties such as cosmetic dermatology, dermatopathology and pediatric dermatology. To learn more visit the ‘What is a Dermatologist?’ page of the American Academy of Dermatology Association website.
Dermatologists can be specially trained to perform a procedure called Mohs surgery. Mohs surgery excises skin cancers in thin layers until all cancer is removed from the tissue (Mayo Clinic Staff, 2017). For more details about each step of the process visit the Skin Cancer Foundation’s site on Mohs Surgery.
Test Yourself
References
Centers for Disease Control and Prevention. (2018, October 25). Psoriasis. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/psoriasis/
Centers for Disease Control and Prevention. (2018a, August 6). Ringworm. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/fungal/diseases/ringworm/definition.html
CrashCourse. (2015, February 16). The Integumentary system, part 2 – skin deeper: Crash Course A&P #7 [Video]. YouTube. https://youtu.be/EN-x-zXXVwQ
Mayo Clinic Staff. (2017, September 6). Mohs surgery. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/mohs-surgery/about/pac-20385222#:~:text=Mohs%20surgery%20is%20a%20precise,known%20as%20Mohs%20micrographic%20surgery.
Ted-Ed. (2018). The science of skin- Emma Bryce [Video]. https://www.youtube.com/watch?v=OxPlCkTKhzY&t=1s
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.