2.3: The PQRSTU Assessment
- Page ID
- 19800
There are many tools to help you further explore a client’s symptoms or signs. A common one follows the mnemonic PQRSTU as illustrated in Figure 2.2, which offers a systematic approach to asking assessment questions without leaving out any details.

| PQRSTU | Questions Related to Pain | Questions Related to Other Symptoms |
|---|---|---|
| Provocative |
|
|
| Palliative |
|
|
| Quality |
Note: If the client struggles to answer this question, you can provide suggestions such as “aching,” “stabbing,” “burning.” |
|
| Quantity |
|
|
| Region |
|
|
| Radiation |
|
|
| Severity (severity scale) |
Note: The severity scale is an important assessment of pain and when used can provide evaluation of a treatment’s effectiveness. After eliciting a baseline, you may provide some sort of pain control intervention and then reassess the pain to see if it was effective. |
|
| Timing |
|
|
| Treatment |
|
|
| Understanding |
|
|
The order of questions you ask will often depend on the symptom or sign and the flow of the conversation with the client. You will also want to be aware of responses that don’t seem to align. For example, if a client responds to the question about quantity of pain by saying “the pain isn’t too bad,” but then rates the severity of their pain as being 8/10, you should probe further. It is okay to say to the client, “I noticed you rated your pain fairly high, at 8/10, but you said it isn’t too bad. Can you tell me more about that?”
When using the PQRSTU mnemonic for assessment, be sure to apply it comprehensively so that you elicit a full understanding of a particular sign or symptom. See Film Clip 2.2 for effective demonstration of using the PQRSTU mnemonic, and Film Clip 2.3 for ineffective demonstration of using the PQRSTU mnemonic.
Film Clip 2.2: Effective use of the PQRSTU mnemonic
Developmental and Cultural Considerations
Younger children or clients with developmental delays or disabilities, or cognitive impairments, may not be able to answer the types of questions shown in Table 2.3. The care partner might be able to help answer some of these questions, and in that case, you should explore “why” and “how” questions. For example, if the care partner indicates that the infant’s pain started two weeks ago, you should ask “Why or how do you know that it started then?” Or if you are working with a young child, you will need to modify your language to be more understandable (e.g., “Where does it hurt?” “Where is your owie?”).
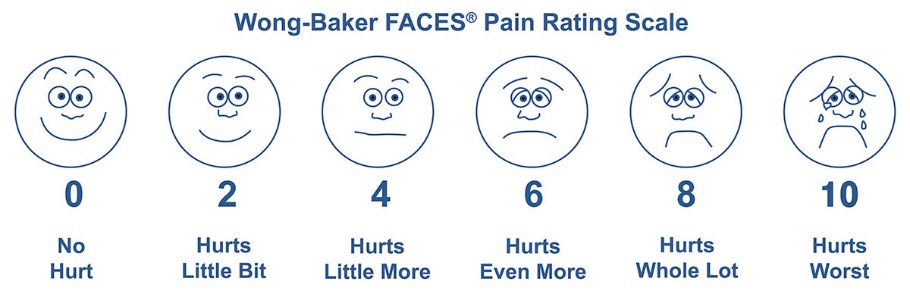
You can also assess pain in young children using the Wong-Baker FACES Pain Rating Scale (see Figure 2.3). When using this scale, ask the client to choose the face that best depicts the pain they are experiencing. You may need to explain what the faces mean: Face 0 doesn’t hurt at all, Face 2 hurts just a little bit, Face 4 hurts a little bit more, Face 6 hurts even more, Face 8 hurts a whole lot, and Face 10 hurts as much as you can imagine.
Test Yourself
Query \(\PageIndex{1}\)

