26.6B: Ovarian Cycle
- Page ID
- 8261
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The menstrual cycle is the physiological process that fertile women undergo for the purposes of reproduction and fertilization.
- Differentiate among the phases of the menstrual cycle
Key Points
- The ovarian cycle refers to the series of changes in the ovary during which the follicle matures, the ovum is shed, and the corpus luteum develops.
- The follicular phase describes the development of the follicle in response to follicle stimulation hormone ( FSH ). As luteinizing hormone ( LH ) and FSH levels increase they stimulate ovulation, or the release of a mature oocyte into the fallopian tubes.
- In the luteal phase, the corpus luteum forms on the ovary and secretes many hormones, most significantly progesterone, which makes the endometrium of the uterus ready for implantation of an embryo.
- If implantation does not occur, the corpus luteum will be degraded, resulting in menstruation.
- If implantation occurs the corpus luteum is maintained.
Key Terms
- ischemic phase: The final part of the secretory phase. The endometrium becomes
pale and arteries constrict due to lower hormone release by the disintegrating corpus
luteum. - granulosa cells: These cells produce
hormones and growth factors that interact with the oocyte during its
development. - menstrual cycle: The recurring cycle of physiological changes in the females of some animal species that is associated with reproductive fertility.
- luteal phase: The latter part of the menstrual cycle that occurs after ovulation, in which the corpus luteum secretes progesterone to prepare the endometrium for the implantation of an embryo.
- follicular phase: The phase of the estrous cycle that involves follicular maturation within the ovary and, controlled by the hormone estradiol.
The menstrual cycle is the scientific term for the physiological changes that occur in fertile women for the purpose of sexual reproduction.The menstrual cycle is controlled by the endocrine system and commonly divided into three phases: the follicular phase, ovulation, and the luteal phase. However, some sources define these phases as menstruation, proliferative phase, and secretory phase. Menstrual cycles are counted from the first day of menstrual bleeding.
The Follicular Phase
The follicular phase (or proliferative phase) is the phase of the menstrual cycle in humans and great apes during which follicles in the ovary mature, ending with ovulation. The main hormone controlling this stage is estradiol. During the follicular phase, follicle-stimulating hormone (FSH) is secreted by the anterior pituitary gland. FSH levels begin to rise in the last few days of the previous menstrual cycle and peak during the first week of the follicular phase. The rise in FSH levels recruits five to seven tertiary-stage ovarian follicles (also known as Graafian or antral follicles) for entry into the menstrual cycle. These follicles compete with each other for dominance.
FSH induces the proliferation of granulosa cells in the developing follicles and the expression of luteinizing hormone (LH) receptors on these granulosa cells. Two or three days before LH levels begin to increase, usually by day seven of the cycle, one or occasionally two of the recruited follicles emerges as dominant. Many endocrinologists believe that estrogen secretion of the dominant follicle increases to a level that indirectly lowers the levels of LH and FSH. This slowdown in LH and FSH production leads to the atresia (death) of most of the recruited follicles, though the dominant follicle continues to mature.
These high estrogen levels initiate the formation of a new layer of endometrium in the uterus. Crypts in the cervix are also stimulated to produce fertile cervical mucus that reduces the acidity of the vagina, creating a more hospitable environment for sperm. In addition, basal body temperature may lower slightly under the influence of high estrogen levels. Ovulation normally occurs 30 (± 2) hours after the beginning of the LH surge (when LH is first detectable in urine).
Ovulation
Ovulation is the phase in which a mature ovarian follicle ruptures and discharges an ovum (also known as an oocyte, female gamete, or egg). Ovulation also occurs in the estrous cycle of other female mammals, which differs in many fundamental ways from the menstrual cycle. The time immediately surrounding ovulation is referred to as the ovulatory phase or the periovulatory period.
The Luteal Phase
The luteal phase (or secretory phase) is the latter part of the menstrual or estrous cycle. It begins with the formation of the corpus luteum and ends in either pregnancy or luteolysis. The main hormone associated with this stage is progesterone, which is significantly higher during the luteal phase than in other phases of the cycle. Some sources define the end of the luteal phase as a distinct ischemic phase.
After ovulation, the pituitary hormones FSH and LH cause the remaining parts of the dominant follicle to transform into the corpus luteum. It continues to grow for some time after ovulation and produces significant amounts of hormones, particularly progesterone, and to a lesser extent, estrogen. Progesterone plays a vital role in making the endometrium receptive to implantation of the blastocyst and supportive of the early pregnancy. It also raises the woman’s basal body temperature. The hormones produced by the corpus luteum suppress production of the FSH and LH, causing the corpus luteum will atrophy. The death of the corpus luteum results in falling levels of progesterone and estrogen. This in turn causes increased levels of FSH, leading to recruitment of follicles for the next cycle. Continued drops in estrogen and progesterone levels trigger the end of the luteal phase, menstruation, and the beginning of the next cycle.
The loss of the corpus luteum can be prevented by implantation of an embryo. After implantation, human embryos produce human chorionic gonadotropin (hCG), which is structurally similar to LH and can preserve the corpus luteum. Because the hormone is unique to the embryo, most pregnancy tests look for the presence of hCG. If implantation occurs, the corpus luteum will continue to produce progesterone (and maintain high basal body temperatures) for eight to twelve weeks, after which the placenta takes over this function.
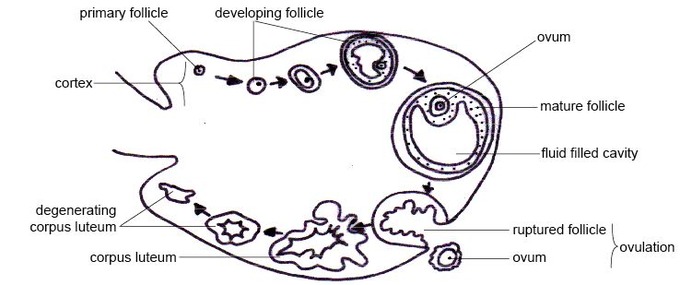
The ovarian cycle: The ovarian cycle is the series of changes that occur in the ovary during the menstrual cycle that cause maturation of a follicle, ovulation, and development of the corpus luteum.

