10.2: Comfort Basic Concepts
- Last updated
- Save as PDF
- Page ID
- 76836

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
Definitions of Pain
Pain has been defined as, “Whatever the patient says it is, experienced whenever they say they are experiencing it.”[1] In 2020 the International Association for the Study of Pain (IASP) released a revised definition of pain as, “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage,” along with these additional notes:
- Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
- Individuals learn the concept of pain throughout all stages of their life.
- A person’s report of an experience as pain should be respected.
- Although pain usually serves an adaptive role, it can have adverse effects on function, socialization, and psychological well-being.
- Verbal description is only one of several behaviors that express pain. The inability to communicate does not negate the possibility that a person is experiencing pain.[2]
Pain motivates the individual to withdraw from dangerous stimuli, to protect a damaged body part while it heals, and to avoid similar experiences in the future. Most pain resolves after the painful stimulus is removed and the body has healed, but sometimes pain persists despite removal of the stimulus and apparent healing of the body. Additionally, pain can occur in the absence of any detectable stimulus, damage, or disease.[3]
Physiology of Pain
Let’s begin by reviewing the physiological processes of pain. A nociceptor is a type of sensory receptor that responds to potentially damaging stimuli by sending nerve signals to the spinal cord and brain in a process called nociception. There are several types and functions of nociceptors:
- Thermal nociceptors are activated by noxious heat or cold, such as a hot pan.
- Mechanical nociceptors are activated by excess pressure or mechanical deformation, such as a finger getting caught in a car door. They also respond to incisions that break the skin surface.
- Chemical nociceptors are activated by a wide variety of spices commonly used in cooking. For example, capsaicin is a compound in chili peppers that causes a burning sensation of the mucus membranes. It is also used in common over-the-counter creams for pain relief because when it is applied to the skin, it blocks the transmission of pain impulses.[4]
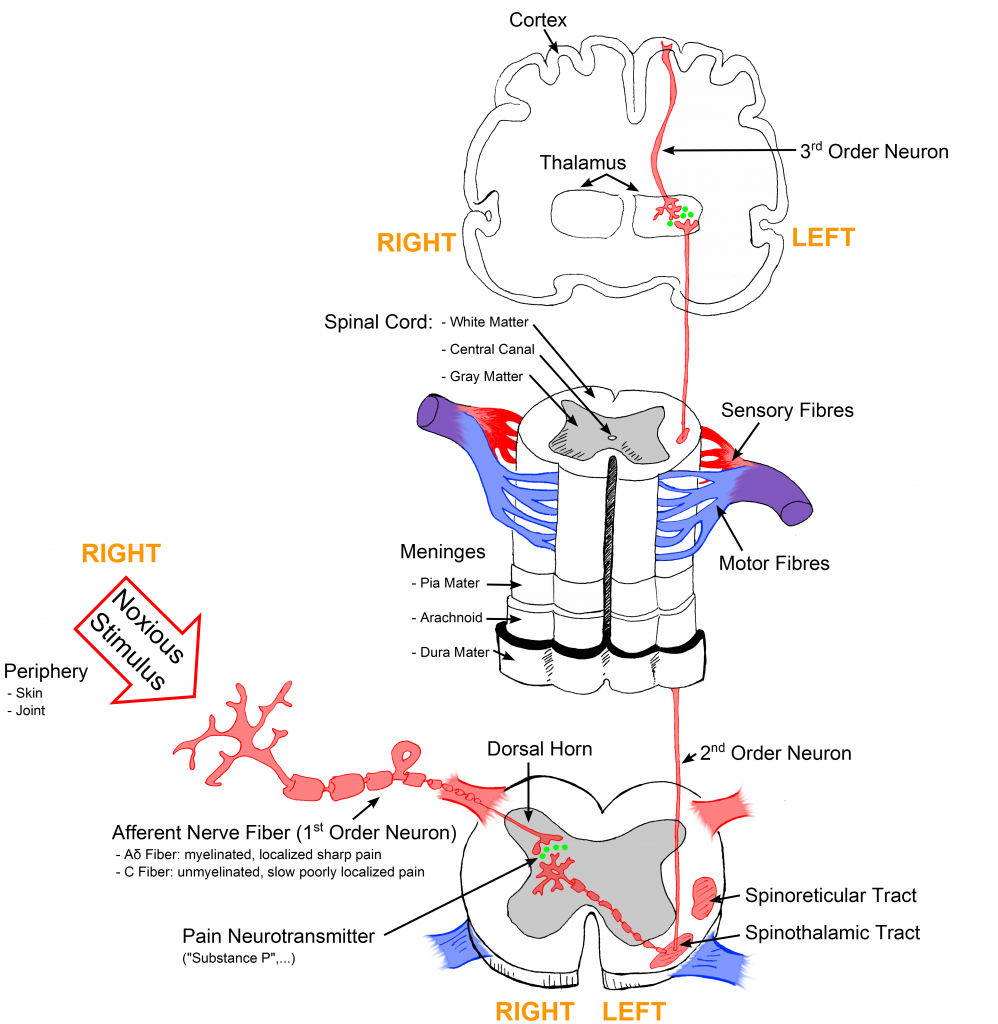
Noxious stimuli are detected by nociceptors and transduced into electrical energy. An action potential is created and transmitted along nociceptor fibers. There are two types of nociceptor fibers, A-Delta and C. A-Delta fibers are fast-conducting fibers and associated with the initial sharp, stinging, or pricking pain sensation. C fibers are slower-conducting fibers and are associated with the secondary sensation of diffuse, dull, burning, and aching pain. The pain impulse is transmitted along these nociceptor fibers to the dorsal horn in the spinal cord and then from the spinal cord to the thalamus, where pain messages are relayed to the cerebral cortex. In the cerebral cortex, pain impulses are perceived and the conscious awareness of pain occurs.[5],[6] See Figure 11.1[7] for an illustration of how the pain signal is transmitted from the nociceptors to the spinal cord and then to the brain.
Note
View supplementary videos on pain:
- Karen D. Davis: How does your brain respond to pain? | TED Talk
- A one-minute review of how pain receptors work: Feeling Pain
Types of Pain
Pain can be divided into visceral, deep somatic, superficial, and neuropathic pain.
- Visceral structures are highly sensitive to stretch, ischemia, and inflammation. Visceral pain is diffuse, difficult to locate, and often referred to a distant, usually superficial, structure. It may be accompanied by nausea and vomiting and may be described as sickening, deep, squeezing, and dull.[8]
- Deep somatic pain is initiated by stimulation of nociceptors in ligaments, tendons, bones, blood vessels, fascia, and muscles and is a dull, aching, poorly localized pain. Examples include sprains and broken bones.[9]
- Superficial pain is initiated by the activation of nociceptors in the skin or other superficial tissue and is sharp, well-defined, and clearly located. Examples of injuries that produce superficial somatic pain include minor wounds and minor (first-degree) burns.[10]
- Neuropathic pain is defined by the International Association for the Study of Pain (IASP) as pain caused by a lesion or disease of the somatosensory nervous system. It is typically described by patients as “burning” or “like pins and needles.” Neuropathic pain can be caused by several disease processes, such as diabetes mellitus, strokes, and HIV, and is generally undertreated because it typically does not respond to analgesics. Medications such as tricyclic antidepressants and gabapentin are typically used to manage this type of pain.[11]
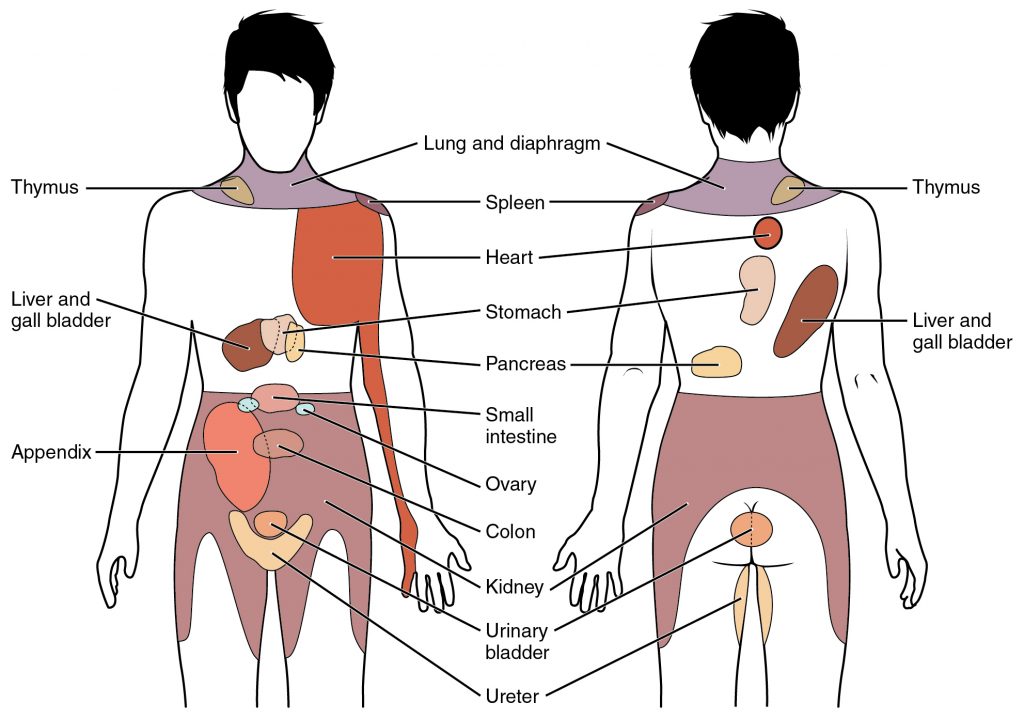
Pain can radiate from one area to another. For example, back pain caused by a herniated disk can cause pain to radiate down an individual’s leg. Referred pain is different from radiating pain because it is perceived at a location other than the site of the painful stimulus. For example, pain from retained gas in the colon can cause pain to be perceived in the shoulder. See Figure 11.2[12] for an illustration of common sites of referred pain.
Factors Affecting the Pain Experience
There are many biological, psychological, and social factors that affect the perception of pain, making it a unique, individual experience. See Table 11.2a for a list of these factors.[13] Nurses must consider these factors while assessing and providing holistic nursing care for patients experiencing pain.
Table 11.2a Biological, Psychological, and Social Factors Affecting Pain
| Biological Factors | Psychological Factors | Social Factors |
|---|---|---|
|
|
|
Acute vs. Chronic Pain
Pain is differentiated between acute pain and chronic pain. Acute pain has limited duration and is associated with a specific cause. It usually causes a physiological response resulting in increased pulse, respirations, and blood pressure. Diaphoresis (sweating, especially to an unusual degree) may also occur. Examples of acute pain include postoperative pain; burns; acute musculoskeletal conditions like strains, sprains, and fractures; labor and delivery; and traumatic injury.
Chronic pain is ongoing and persistent for longer than six months. It typically does not cause a change in vital signs or diaphoresis. It may be diffuse and not confined to a specific area of the body. Chronic pain often affects an individual’s psychological, social, and behavioral responses that can influence daily functioning. Chronic medical problems, such as osteoarthritis, spinal conditions, fibromyalgia, and peripheral neuropathy, are common causes of chronic pain. Chronic pain can continue even after the original injury or illness that caused it has healed or resolved. Some people suffer chronic pain even when there is no past injury or apparent body damage.
People who have chronic pain often have physical effects that are stressful on the body. These effects include tense muscles, limited ability to move around, lack of energy, and appetite changes. Emotional effects of chronic pain include depression, anger, anxiety, and fear of reinjury. These effects can limit a person’s ability to return to their regular work or leisure activities.[14] It is estimated that chronic pain affects 50 million U.S. adults, and 19.6 million of those adults experience high-impact chronic pain that interferes with daily life or work activities.[15] See Figure 11.3[16] for an illustration of low back pain, an example of both acute and chronic pain that often affects daily functioning.

Note
Read additional information about pain using the following hyperlinks:
Life Span and Cultural Considerations
The pain experience varies across the life span. Newborns and infants can feel pain but are unable to verbalize it. Repetitive and prolonged pain may be associated with altered pain sensitivity and pain processing later in life. Toddlers and preschoolers often have difficulty describing, identifying, and locating pain. Instead, pain may be demonstrated behaviorally with crying, anger, physical resistance, or withdrawal. School-age children and adolescents may try to be “brave” and rationalize the pain; they are more responsive to explanations about pain.
Older adults are at increased risk for undertreatment of pain. It is estimated that up to 70% of older adults in the community and up to 85% living in long-term care centers have significant pain due to chronic conditions such as osteoarthritis and peripheral neuropathy. Pain is often underassessed in older adults because they are less likely to report it and also because it can present atypically with confusion and agitation.[17]
Other special populations who are at increased risk for the undertreatment of pain include the following:
- Patients with a history of addictive disease
- Nonverbal, cognitively impaired, or unconscious patients
- Patients who endure pain without complaining due to cultural or religious beliefs
- Non-English speaking patients where communicating is a barrier
- Uninsured or underinsured patients where cost of medications is a barrier[18]
Nurses must be especially vigilant of nonverbal signs of pain in these at-risk groups and implement appropriate assessment tools and interventions. Read an example of a patient with untreated pain in the following box.
A True Story of Undertreated Pain
A teenage boy from the Amish community was admitted to the hospital after he sustained several fractures when his buggy was hit by a motor vehicle. His parents stayed at his bedside throughout his hospital stay. The nurses noticed that although he denied pain, he grimaced and guarded the body parts that were injured. He moaned when repositioned and declined to get out of bed to begin physical therapy when it was prescribed for rehabilitation. However, despite these nonverbal indicators of pain, he continued to deny the existence of pain and refused all pain medication. One day, when his parents left the room briefly to get coffee, the nurse said to the patient, “Most people in your situation experience severe pain. I can see that you are hurting by your expressions when you move. Can you help me to understand why you don’t want any pain medication?” A tear began to fall down the boy’s cheek. He explained that his community does not believe in complaining about pain and to be a man, he must learn how to tolerate suffering. The nurse explained, “It is important for you to attend physical therapy so that you can heal and go home. Can we bring you pain pills every day before physical therapy so that you can participate in the exercises, recover quickly, and go home?” The boy agreed to this plan. The nurse documented her findings and made notes in the care plan to administer the prescribed PRN pain medications one hour before physical therapy was scheduled. She also communicated her findings during the nurse handoff report. The boy was able to satisfactorily complete the prescribed physical therapy and was discharged home the following week.
Note
Use the following hyperlinks to read more information about treating pain:
- Treating pain in Special Populations
- The National Institute on Aging provides a wide range of information for older adults: Pain: You Can Get Help.
- Health in Aging offers additional information on pain management at Pain Management | Aging & Health AZ | American Geriatrics Society.
Trends in Pain Management, Substance Abuse, and Addiction
Several well-known agencies have recently published materials focused on the importance of optimal pain management. For example, in 2017 The Joint Commission published new and revised standards of pain assessment and pain management that apply to all Joint Commission-accredited hospitals.[19] The American Nurses Association published a position statement in 2018 on the ethical responsibility of nurses to properly manage pain.[20] In 2019 the U.S. Department of Health and Human Services published Pain Management Best Practices.[21] Why is there continued emphasis on optimal pain management? Let’s review some trends related to pain management over the past few decades.
Pain assessment and pain management began to undergo significant changes in the 1990s when pain experts recognized that inadequate assessment and treatment of pain had become a public health issue. Recommendations for improving the quality of pain care were followed by initiatives that recognized patients’ reported pain as “the 5th vital sign.” Hospital administrators and regulators began to focus on pain scores, encouraging and incentivizing providers to aggressively treat pain to lower pain scores. These trends led to liberal prescribing of opioid pain medications for both acute and chronic pain.
Unfortunately, this increase in prescription of opioid pain medication led to an associated rise in the number of deaths from overdose. Organizations began to urge caution about the use of opioids for pain, including guidelines published in 2016 by the Centers for Disease Control (CDC) on prescribing opioids for pain.[22] The 2016 CDC guideline led to limited prescriptions of opioids and unintended consequences, such as forced tapering of medications for established patients requiring chronic pain control and the transition of some patients desperate for pain control to using illicit drugs, such as heroin.
In this manner, pain management and the opioid crisis have influenced one another as each continues to evolve. It is imperative for nurses to ensure that patients with painful conditions can work with their health care providers to develop pain treatment plans that balance pain control, optimize function, and enhance quality of life while also minimizing risks for opioid misuse and harm.[23]
Associated Definitions
When discussing the use and abuse of drugs used to treat pain, it is important to distinguish between tolerance, physical dependence, misuse, substance abuse disorder, and addiction.
- Tolerance is a reduced response to pain medication when the same dose of a drug has been given repeatedly, requiring a higher dose of the drug to achieve the same level of response.[24] For example, when a patient receives morphine for palliative care, the dosage often needs to be increased over time because the patient develops a tolerance to the effects of the medication.
- Physical dependence refers to withdrawal symptoms that occur when a chronic pain medication is suddenly reduced or stopped because of physiological adaptations that occur to chronic exposure to the medication.[25] For example, if a patient who receives hydromorphone daily suddenly has their prescription stopped, they will likely experience symptoms of withdrawal, such as sweating, goose bumps, vomiting, anxiety, insomnia, and muscle pain.
- Misuse refers to a person taking prescription pain medications in a manner or dose other than prescribed; taking someone else’s prescription, even if for a medical complaint such as pain; or taking a medication to feel euphoria (i.e., to get high).[26]
- Substance abuse disorder is a significant impairment or distress from a pattern of substance use (i.e., alcohol, drugs, or prescription medication) with at least two of the symptoms listed below in a given year:
- The use of more of a substance than planned or using a substance for a longer interval than desired
- The inability to cut down despite desire to do so
- Spending a substantial amount of the day obtaining, using, or recovering from substance use
- Cravings or intense urge to use a substance
- Repeated usage causing an inability to meet important social or professional obligations
- Persistent usage despite user’s knowledge that it is causing frequent problems at work, school, or home
- Giving up or cutting back on important social, professional, or leisure activities because of use
- Usage in physically hazardous situations, such as driving, or usage despite it causing physical or mental harm
- Persistent use despite the user’s awareness that the substance is causing, or at least worsening, a physical or mental problem[27]
- Addiction is a chronic disease of the brain’s reward, motivation, memory, and related circuitry reflected in an individual pathologically pursuing reward and/or relief by substance use. Addiction is characterized by several symptoms, such as the inability to consistently abstain from a substance, impaired behavioral control, craving, diminished recognition of significant problems with one’s behaviors and interpersonal relationships, and a dysfunctional emotional response. Like other chronic diseases, addiction often involves cycles of relapse and remission. Without treatment or engagement in recovery activities, addiction is progressive and can result in disability or premature death.[28]
Substance Abuse Among Nurses and Nursing Students
Substance abuse and addiction can occur in anyone, including nurses and nursing students. The American Nursing Association released the following statements in 2016:
- Health care facilities should provide education to nurses and other employees regarding alcohol and other drug use and establish policies, procedures, and practices to promote safe, supportive, drug-free workplaces.
- Health care facilities and schools of nursing should adopt alternative-to-discipline approaches to treating nurses and nursing students with substance use disorders, with stated goals of retention, rehabilitation, and reentry into safe, professional practice.
- Drug diversion, in the context of personal use, is viewed primarily as a symptom of a serious and treatable disease, and not exclusively as a crime.
- Nurses and nursing students are aware of the risks associated with substance use, impaired practice, and drug diversion and have the responsibility and means to report suspected or actual concerns.[29]
Note
Read the American Nurses Association (ANA) statement on Substance Use Among Nurses and Nursing Students.
Read the NCSBN brochure on Substance Use Disorder in Nursing. Many states offer assistance to nurses with substance use disorders to maintain their nursing license and employment status. See Wisconsin’s Professional Assistance Procedure (PAP) or New York’s Statewide Peer Assistance for Nurses program.
Read more details about substance abuse disorder in the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Standards of Care
Pain assessment and management standards were recently revised and published in 2018 by The Joint Commission. The revised standards require hospitals to identify pain assessment and pain management, including safe opioid prescribing, as an organizational priority. Nurses are expected to implement these best practices. See Table 11.2b for a summary of associated requirements that must be incorporated into nursing care.[30] If these components are not included when providing nursing care, the hospital may be cited by The Joint Commission and potentially lose Medicare funding.
Table 11.2b. The Joint Commission’s Pain Assessment and Management Requirements[31]
| Requirement | Rationale |
|---|---|
| Patients are screened for pain during emergency department visits and at the time of admission. | The misidentification and undertreatment of pain continues to occur in hospitals.
When a patient presents to the hospital for other medical issues, pain may be overlooked or missed. Screening patients for pain or the risk of pain at the time of admission and while taking vital signs helps to improve pain identification and treatment. |
| Criteria to screen, assess, and reassess pain are used that are consistent with the patient’s age, condition, and ability to understand. | An accurate screening and assessment are required for satisfactory pain management, and the hospital is responsible for ensuring that appropriate screening and assessment tools are readily available and used appropriately. |
| Patients are involved in the pain management treatment planning process by:
– Collaboratively developing realistic expectations and measurable goals for the degree, duration, and reduction of pain – Discussing the criteria used to evaluate treatment progress (for example, relief of pain and improved physical and psychosocial function) – Receiving education on pain management, treatment options, and safe use of opioid and nonopioid medications when they are prescribed |
Patient involvement in planning pain management involves information sharing and collaboration between the patient and provider to arrive at realistic expectations and clear goals. Numerous patient factors may cause undertreatment or overtreatment of pain, such as pain expectations, knowledge of pain and its treatment, and underreporting of pain. Patient involvement in the pain management planning process allows the provider to clarify the objectives of the process and guides patients in a manner that increases the likelihood of treatment adherence. |
| Patient’s pain is treated or they are referred for treatment.
Treatment strategies for pain may include nonpharmacologic, pharmacologic, or a combination of approaches. |
Referrals may be required for patients who present with complex pain management needs, such as the opioid-addicted patient, the patient who is at high risk for adverse events but requires treatment with opioids, or a patient whose pain management needs exceed the expertise of the patient’s provider. |
| Nonpharmacologic pain treatment modalities are promoted. | Nonpharmacologic modalities should be promoted by ensuring that patient preferences are discussed and some nonpharmacologic treatment options provided. Nonpharmacologic strategies include, but are not limited to, physical modalities (e.g., acupuncture therapy, chiropractic therapy, osteopathic manipulative treatment, massage therapy, and physical therapy), relaxation therapy, and cognitive behavioral therapy. |
| Patients identified as being high risk for adverse outcomes related to opioid treatment are monitored. | The most dangerous adverse effect of opioid analgesics is respiratory depression.
Equipment must be available to monitor patients deemed highest risk (e.g., patients with sleep apnea, those receiving continuous intravenous opioids, or those on supplemental oxygen). |
| Patients experiencing opioid substance abuse are referred to opioid treatment programs. | When clinicians encounter patients who are addicted to opioids, the patients should be referred for treatment. The U.S. Substance Abuse and Mental Health Services Administration provides a directory of opioid treatment programs. |
| The hospital facilitates access to the Prescription Drug Monitoring Program databases. | Prescription Drug Monitoring Programs (PDMP) aggregate prescribing and dispensing data submitted by pharmacies and health care providers. They are an effective tool for reducing prescription drug abuse and diversion. Read more about PDMP in the “Legal/Ethical” chapter of the Open RN Nursing Pharmacology textbook. |
| Patient’s pain is reassessed and responded to through the following:
Evaluation and documentation of: – Response to pain intervention(s) – Progress toward pain management goals including functional ability (for example, the ability to take a deep breath, turn in bed, walk with improved pain control) – Side effects of treatment |
Reassessment should be completed in a timely manner to determine if the intervention is working or if the patient is experiencing adverse effects. Only using numerical pain scales to monitor patients’ pain is inadequate.
The Joint Commission’s technical advisory panel stressed the importance of assessing how pain affects function and the ability to make progress towards treatment goals. For example, immediately after major abdominal surgery, the goal of pain control may be the patient’s ability to take a breath without excessive pain. Over the next few days, the goal of pain control may be the ability to sit up in bed or walk to the bathroom without limitation due to pain. |
| Patients and their family members are educated on discharge plans related to pain management including the following:
– Pain management plan of care – Side effects of pain management treatment – Activities of daily living, including the home environment that might exacerbate pain or reduce effectiveness of the pain management plan of care, as well as strategies to address these issues – Safe use, storage, and disposal of opioids when prescribed |
During the discharge process, patients and families need education on the importance of how to manage the patient’s pain at home. Unmanaged pain may cause a patient to regress in their recovery process or have uncontrolled pain at home leading to a readmission to the hospital. It is necessary to have a discussion with patients and their families regarding their home environment and activities of daily living that may increase the need for pain management. When a patient is being discharged with an opioid medication, education on safe use, including when and how much medication to take, should be included in the discharge plan. Opioid disposal education is also critical to both reduce diversion and decrease the risk of accidental exposure to someone other than the person for whom the opioid was prescribed. |
Note
Read The Joint Commission’s Pain Assessment and Management Standards for Hospitals.
Read Pain Management Best Practices from the United States Department of Health & Human Services.
- Pasero, C., & MacCaffery, M. (2010). Pain assessment and pharmacological management (1st ed.). Mosby. ↵
- International Association for the Study of Pain. (2017, December 14). IASP terminology. https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- NursingTimes. (2008, September 18). Anatomy and physiology of pain. https://www.nursingtimes.net/clinical-archive/pain-management/anatomy-and-physiology-of-pain-18-09-2008/#:~:text=The%20transmission%20process%20occurs%20in,higher%20levels%20of%20the%20brain↵
- "Sketch colored final.png" by Bettina Guebeli is licensed under CC BY-SA 4.0) ↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- This work is a derivative of Anatomy and Physiology by Boundless and is licensed under CC BY-SA 4.0↵
- Murnion, B. P. (2018). Neuropathic pain: Current definition and review of drug treatment. Australian Prescriber, 41(3), 60–63. https://doi.org/10.18773/austprescr.2018.022↵
- “1506_Referred_Pain_Chart.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://cnx.org/contents/C650g-ah@2/Autonomic-Reflexes-and-Homeostasis↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- Cleveland Clinic. (2020, December 8). Acute v. chronic pain. https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf ↵
- “Lower_back_pain.jpg” by Injurymap is licensed under CC BY 4.0↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care (ELNEC). https://www.aacnnursing.org/ELNEC↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care (ELNEC). https://www.aacnnursing.org/ELNEC↵
- The Joint Commission. (2017, August 29). R3 report | Requirements, rationale, reference.https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/r3_report_issue_11_pain_assessment_8_25_17_final.pdf?db=web&hash=938C24A464A5B8B5646C8E297C8936C1↵
- ANA Center for Ethics and Human Rights. (2018). Position statement: The ethical responsibility to manage pain and the suffering it causes. American Nurses Association. https://www.nursingworld.org/~495e9b/globalassets/docs/ana/ethics/theethicalresponsibilitytomanagepainandthesufferingitcauses2018.pdf↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- Cleveland Clinic. (2020, December 8). Acute v. chronic pain.https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf/↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596↵
- Pain Management Best Practices Inter-Agency Task Force. (2019, May 9). Pain management best practices. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf↵
- American Nurses Association. (2016, October). Substance use among nurses and nursing students.https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/substance-use-among-nurses-and-nursing-students↵
- The Joint Commission. (2017, August 29). R3 report | Requirements, rationale, reference. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/r3_report_issue_11_pain_assessment_8_25_17_final.pdf?db=web&hash=938C24A464A5B8B5646C8E297C8936C1↵
- The Joint Commission. (2017, August 29). R3 report | Requirements, rationale, reference. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/r3_report_issue_11_pain_assessment_8_25_17_final.pdf?db=web&hash=938C24A464A5B8B5646C8E297C8936C1↵

