7.3: Intradermal and Subcutaneous Injections
- Page ID
- 10033
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Intradermal injections (ID) are injections administered into the dermis, just below the epidermis. The ID injection route has the longest absorption time of all parenteral routes. These types of injections are used for sensitivity tests, such as TB (see Figure 7.13), allergy, and local anesthesia tests. The advantage of these tests is that the body reaction is easy to visualize, and the degree of reaction can be assessed. The most common sites used are the inner surface of the forearm and the upper back, under the scapula. Choose an injection site that is free from lesions, rashes, moles, or scars, which may alter the visual inspection of the test results (Lynn, 2011).
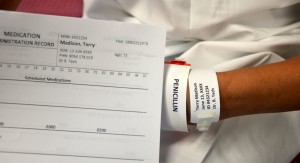
Equipment used for ID injections is a tuberculin syringe calibrated in tenths and hundredths of a millilitre, and a 1/4 to 1/2 in., 26 or 27 gauge needle. The dosage of an ID injection is usually under 0.5 ml. The angle of administration for an ID injection is 5 to 15 degrees. Once the ID injection is completed, a bleb (small blister) should appear under the skin. Checklist 56 outlines the steps to administer an intradermal injection.

Figure 7.13 TB syringe
Checklist 56: Administering an Intradermal (ID) InjectionDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
||||
Safety Considerations:
|
||||
Steps |
Additional Information |
|||
| 1. Prepare medication or solution as per agency policy. Ensure all medication is properly identified. Check physician orders, Parenteral Drug Therapy Manual (PDTM), and MAR to validate medication order and guidelines for administration. | Properly identifying medication decreases risk of inadvertently administering the wrong medication.
Preparing medications ensures patient safety with medication administration. 
Compare physician orders and MAR 
Prepare medication from a vial |
|||
| 2. Perform hand hygiene; gather supplies. | Gather all supplies: medication syringe, non-sterile gloves, alcohol swab and sterile gauze, Band-Aid (if required).

Required supplies |
|||
| 3. Enter room and introduce yourself, explain procedure and the medication, and allow patient time to ask questions. | Explaining rationale increases the patient’s knowledge and reduces their anxiety. | |||
| 4. Close the door or pull the bedside curtains. | This provides patient privacy. | |||
| 5. Compare MAR to patient wristband and verify this is the correct patient using two identifiers. | This ensures accuracy of the medication or solution and prevents errors.
Two patient identifiers are patient name and date of birth. 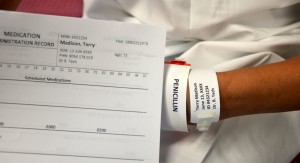
Compare MAR with patient wristband |
|||
| 6. Assess patient for any contraindications to the medications. | Assessment is a prerequisite for every medication given. | |||
| 7. Select appropriate site for administration. Assist the patient to the appropriate position as required. | Site should be free from lesions, rashes, and moles. Selecting the correct site allows for accurate reading of the test site at the appropriate time.

Assess site for ID injection |
|||
| 8. Perform hand hygiene and apply non-sterile gloves. | Gloves help prevent exposure to contaminants.

Apply non-sterile gloves |
|||
| 9. Clean the site with an alcohol swab or antiseptic swab. Use a firm, circular motion. Allow the site to dry. | Pathogens from the skin can be forced into the tissues by the needle. Allowing the skin to dry prevents introducing alcohol into the tissue, which can be irritating and uncomfortable.

Clean injection site |
|||
| 10. Remove needle from cap by pulling it off in a straight motion. | This decreases risk of accidental needle-stick injury.

Remove needle from cap |
|||
| 11. Using non-dominant hand, spread the skin taut over the injection site. | Taut skin provides easy entrance for the needle.

Hold skin taut prior to injection |
|||
| 12. Hold the syringe in the dominant hand between the thumb and forefinger, with the bevel of the needle up. | This allows for easy handling of the syringe.

Hold needle with bevel up |
|||
| 13. Hold syringe at a 5- to 15-degree angle from the site. Place the needle almost flat against the patient’s skin, bevel side up, and insert needle into the skin. Insert the needle only about 1/4 in., with the entire bevel under the skin. | Keeping the bevel side up allows for smooth piercing of the skin and induction of the medication into the dermis.

ID injection |
|||
| 14. Once syringe is in place, slowly inject the solution while watching for a small weal or bleb to appear. | The presence of the weal or bleb indicates that the medication is in the dermis.

Presence of a bleb (white raised circle) |
|||
| 15. Withdraw the needle at the same angle as insertion, engage safety shield or needle guard, and discard in a sharps container.
Do not massage area after injection. |
Withdrawing at the same angle as insertion minimizes discomfort to the patient and damage to the tissue.
Proper needle disposal prevents needle-stick injuries. 
Discard syringe in sharps container Massaging the area may spread the solution to the underlying subcutaneous tissue. Gently pat with sterile gauze if blood is present. |
|||
| 16. If injection is a TB skin test, circle the area around the injection site to allow for easy identification of site in three days. |

Draw circle around injection site |
|||
| 17. Discard remaining supplies, remove gloves, and perform hand hygiene. | This prevents the spread of microorganisms.

Hand hygiene with ABHR |
|||
| 18. Document the procedure and findings according to agency policy. | Proper documentation helps ensure patient safety. Document time, date, location, and type of medication injected. | |||
| 19. Evaluate the patient response to injection within appropriate time frame. | The patient will need to be evaluated for therapeutic and adverse effects of the medication or solution. | |||
| Data source: ATI, 2015a; Berman & Snyder, 2016; Brookside Associates, 2015a; Clayton, Stock, & Cooper, 2010; Perry et al., 2014 | ||||
Subcutaneous Injections
Subcutaneous (SC) injections are administered into the adipose tissue layer just below the epidermis and dermis. This tissue has few blood vessels, so drugs administered by this route have a slow, sustained rate of absorption. Sites for SC injections include the outer aspect of the upper arm, the abdomen (from below the costal margin to the iliac crest) within one inch of the belly button, anterior aspects of the thighs, upper back, and upper ventral gluteal area (Lynn, 2011) (see Figure 7.14).
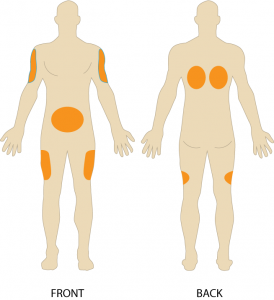
Figure 7.14 SC injection sites
Choose a site that is free of skin lesions and bony prominences. Site rotation prevents the formation of lipohypertrophy or lipoatrophy in the skin. Physical exercise or application of hot or cold compresses influences the rate of drug absorption by altering local blood flow to the tissues. Any condition that impairs that blood flow to the subcutaneous tissue contradicts the use of subcutaneous injections. Examples of subcutaneous medications include insulin, opioids, heparin, epinephrine, and allergy medication (Perry et al., 2014).
To administer an SC injection, a 25 to 30 gauge, 3/8 in. to 5/8 in. needle is used. Some subcutaneous injections come prefilled with the syringe attached. Always confirm that the right-size needle is appropriate for the patient before use. Subcutaneous injections are usually given at a 45- to 90-degree angle. The angle is based on the amount of subcutaneous tissue present. Generally, give shorter needles at a 90-degree angle and longer needles at a 45-degree angle (Lynn, 2011). SC injections do not need to be aspirated as the likelihood of injecting into a blood vessel is small. Usually, no more than 1 ml of medication is given subcutaneously, as larger amounts may cause discomfort to the patient and may not be absorbed appropriately (Lynn, 2011).
There are varying opinions on whether to pinch the skin during administration. Pinching is advised for thinner patients in order to lift the adipose tissue up and away from the underlying muscle and tissue. If pinching is used, release the pinch when the needle is inserted to avoid injecting into compressed tissue. Note, too, that elevating or pinching the skin has been found to increase the risk of injury, as the needle may pierce the opposite side of the skin fold and enter the skin of the health care worker (Black, 2013). The abdomen is the best location for an SC injection if a patient has little peripheral SC tissue. If patient is obese, use a needle that is long enough to insert through the tissue at the base of the skin fold (Perry et al., 2014).
Insulin SC Injections
Insulin is considered a high-risk medication, and special care must be taken to ensure the correct amount of medication and type of insulin is administered at the correct time. As well, safety checks related to a patient receiving SC insulin should be carried out (Ellis & Parush, 2012). Table 7.5 lists specific guidelines for administering insulin (and see Figure 7.15).
| Table 7.5 Guidelines for Administering SC Insulin | |||
|
Insulin |
Additional Information |
||
| Insulin is considered a high-risk medication. | Special care must be taken to ensure the correct amount of medication and type of insulin is administered, at the correct time. It is highly recommended to always get your insulin dosages double-checked by another health care provider. Always follow the standard for medication preparation at your agency. | ||
| Insulin is only administered using an insulin syringe. | Insulin is the only drug with its own type of syringe with a needle attached. Insulin is always ordered and administered in units, based on a blood sugar reading and a diabetic insulin protocol (or sliding scale). Some hospitals have preprinted physician orders, and some hospitals have handwritten orders. Insulin syringes can come in 30-, 50-, or 100-unit measurements. Always read the increments (calibration) carefully. | ||
| There are different types of insulin. | There are rapid-, short-, intermediate-, and long-acting insulins. For each type of insulin, it is important to know how the insulin works and the onset, peak, and duration of the insulin. | ||
| Administering two different types of Insulin. | If a patient is ordered two types of insulin, some insulins may be mixed together in one syringe. Many insulins MAY NOT be mixed together. Do not mix Lantus (Glargine) or Levemir (Determir).If administering cloudy insulin preparations (Humulin – N), gently roll the vial between the palms of your hands to re-suspend the medication. Always draw up the short acting insulin first, to prevent it from being contaminated with the long acting. If too much insulin is drawn up from the second vial, discard syringe and start again. Always check with the PDTM for the most current guidelines regarding insulin administration.Insulin orders may change from day to day. Always ensure the most current physician orders are being followed. |
||
| Know about rotating injection sites. | Injection site rotation is no longer necessary as newer insulins have a lower risk for hypertrophy of the skin. Typically, a patient will pick one anatomic area (e.g., upper arm) and rotate the injection sites within that region to maintain consistent insulin absorption from day to day. Insulin absorption rates vary from site to site. The abdomen absorbs the fastest, followed by the arms, thighs, and buttocks. | ||
| Know when to administer insulin. | The timing of insulin injections is critical to correct insulin administration based on blood sugar levels and when the patient will eat. Knowing the peak action and duration of insulin is critical to proper insulin medication management. If giving insulin, always ensure the patient is not nauseated, is able to eat, and that food is arriving before the insulin starts working. Typically, short- or rapid-acting insulin is given 15 minutes before meals. Intermediate- or long-acting insulin may be given twice daily, at breakfast and dinner. | ||
| Measure blood sugar levels and food intake. | Insulin injections are based on blood sugar values and on when the patient will eat. The timing of an insulin injection is critical to ensure the patient receives insulin correctly. | ||
| Use insulin injection pens. | Injection pens are a new technology used by patients to self-inject insulin using a syringe, needle, and prefilled cartridge of insulin. It is essential that patients be taught how to use injection pens so they understand the technology.
A mini-infusion pump is a battery-operated machine that delivers medications in very small amounts to patients with controlled infusion times. The most common types of mini-infusion sets are insulin pumps or subcutaneous infusion devices. For more information on mini-infusion sets and volume-controlled sets, see Suggested Online Resources in section 7.8. |
||
| Data source: Canadian Diabetes Association, 2013; Perry et al., 2014 | |||

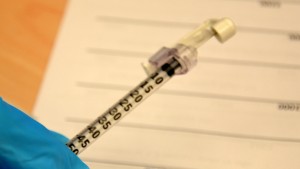
Figure 7.15 Insulin syringe with needle attached
Special considerations:
- Insulin is stored in the refrigerator. When a vial is in use, it should be at room temperature. Do not administer cold insulin. Check agency policy for how long a vial can be used.
- Patients who take insulin should monitor their blood sugar (glucose) levels as prescribed by their health care provider.
- Vials of insulin should be inspected prior to use. Any change in appearance may indicate a change in potency.
- Use the type of insulin prescribed. Do not change the type unless ordered by a health care provider.
- Allow patient to choose site for injection. A patient may self-administer insulin if it’s determined to be safe and in the patient’s best interest.
- All health care providers should be aware of the signs and symptoms of hypoglycemia. Signs and symptoms include fruity breath, restlessness, agitation, confusion, slurring of words, clammy skin, inability to concentrate or follow commands, hunger, and nausea. The patient may complain of blurred or double vision. Late signs include unconsciousness. Hypoglycemia is a medical emergency. Always have an emergency diabetic kit available. If a conscious diabetic patient appears to be hypoglycemic or has a blood sugar (glucose) reading of 4 mmol/L or lower, give glucose, such as sucrose tablets, solution, or juice. Follow agency policy regarding hypoglycemic reactions.
Heparin SC Injections
Heparin is an anticoagulant used to reduce the risk of thrombosis formation by suppressing clot formation (Perry et al., 2014). Heparin is also considered a high-alert medication (ISMP, 2014).
Table 7.6 provides specific guidelines to consider before and after administering heparin.
| Table 7.6 Guidelines for Administering SC Heparin | |||
|
Heparin |
Additional Information |
||
| Heparin is considered a high-risk medication. | Heparin is available in vials and prefilled syringes in a variety of concentrations. Because of the dangerous adverse effects of the medication, it is considered a high-risk medication. Always follow agency policy regarding the preparation and administration of heparin. | ||
| Rotate heparin injection sites. | It is important to rotate heparin sites to avoid bruising in one location. To minimize bruising and pain associated with heparin injections, they can be given in the abdominal area, at least 5 cm away from the belly button. | ||
| Know the risks associated with heparin. | There are many risks associated with the administration of heparin, including bleeding, hematuria, hematemesis, bleeding gums, and melena. | ||
| Review lab values. | Review lab values (PTT and aPTT) before and after heparin administration. | ||
| Use prepackaged heparin syringes. | Many agencies use prepackaged heparin syringes. Always follow the standards for safe medication administration when using prefilled syringes. Low molecular weight heparin (LMWH) is more effective in some patients. | ||
| Assess patient conditions prior to administration. | Some conditions increase the risk for hemorrhage (bleeding), such as recent childbirth, severe diabetes, severe kidney and liver disease, severe traumas, cerebral or aortic aneurysm, cerebral vascular accidents (CVA), blood dyscrasias, and severe hypotension. | ||
| Assess medications prior to administration. | Over-the-counter (OTC) herbal medications, such as garlic, ginger, and horse chestnut, may interact with heparin. Additional medications that may interact include Aspirin, NSAIDS, cephalosporins, anti-thyroid agents, thrombolytics, and probenecids. | ||
| Data source: Clayton et al., 2010; Ogston-Tuck, 2014b; Perry et al., 2014 | |||
Checklist 57 provides the steps to complete a subcutaneous injection.
Checklist 57: Administering a Subcutaneous InjectionsDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety Considerations:
|
|||
Steps |
Additional Information |
||
| 1. Prepare medication or solution as per agency policy. Always compare the physician orders with the MAR. | Preparing medications ensures patient safety with medication administration.

Prepare medication |
||
| 2. Perform hand hygiene; gather supplies. | You will need medication syringe, non-sterile gloves, alcohol swab and sterile gauze, Band-Aid. | ||
| 3. Enter room and introduce yourself. Identify patient using two acceptable identifiers, explain procedure and the medication, and allow patient time to ask questions. | Explaining rationale increases the patient’s knowledge and reduces their anxiety. | ||
| 4. Close the door or pull the bedside curtains. | This provides patient privacy. | ||
| 5. Compare MAR to patient wristband and verify this is the correct patient using two identifiers. | This ensures accuracy of the medication or solution and prevents errors.
Compare MAR with patient wristband |
||
| 6. Assess patient for any contraindications for the medications. | Assessment is a prerequisite to the administration of medications. | ||
| 7. Put on non-sterile gloves. | Gloves help prevent exposure to contaminants.

Apply non-sterile gloves |
||
| 8. Select appropriate site for administration. Assist the patient to the appropriate position as required. | Site should be free from lesions, rashes, and moles. Choosing the correct site allows for accurate reading of the test site at the appropriate time.

SC site for injection (back of upper arm) |
||
| 9. Clean the site with an alcohol swab or antiseptic swab. Use a firm, circular motion. Allow the site to dry. | Pathogens from the skin can be forced into the tissues by the needle. Allowing the skin to dry prevents introducing alcohol into the tissue, which can be irritating and uncomfortable.

Clean site with alcohol swab |
||
| 10. Remove the needle cap with the non-dominant hand, pulling it straight off. | This technique lessens the risk of an accidental needle-stick injury. | ||
| 11. Grasp or pinch the area surrounding the injection site, or spread the skin taut at the site. | The decision to create a skin fold is based on the nurse’s assessment of the patient and the needle length used. Pinching is advised for thinner patients.

Select SC site (back of upper arm) |
||
| 12. Hold the syringe in the dominant hand between the thumb and forefinger. Insert the needle quickly at a 45- to 90-degree angle. | Inserting quickly causes less pain to the patient. Subcutaneous tissue is abundant in well-nourished, well-hydrated people. For patients with little subcutaneous tissue, it is best to insert the needle at a 45-degree angle. | ||
| 13. After the needle is in place, release the tissue. Move your non-dominant hand to steady and lower the end of the needle. With your dominant hand, inject the medication at a rate of 10 seconds per ml. Avoid moving the syringe. | Keeping the needle steady helps keep the needle in place.

SC injection 
Inject medication |
||
| 14. Withdraw the needle quickly at the same angle at which it was inserted, while supporting the surrounding tissue with your non-dominant hand. | Withdrawing at the same angle prevents tissue damage and increased pain at the injection site. | ||
| 15. Using a sterile gauze, apply gentle pressure at the site after the needle is withdrawn. Do not massage the site. | Massage is not necessary and can damage underlying tissue. Massaging after a heparin injection can contribute to the formation of a hematoma. | ||
| 16. Do not recap the needle. Apply the safety shield or needle guard on needle and dispose in a sharps container. | Safety shields and needle guards help prevent accidental needle-stick injuries.
SC needle with safety shield 
Discard syringe in sharps container |
||
| 17. Dispose of supplies; remove gloves and perform hand hygiene. | This reduces the risk of infection and the spread of microorganisms.

Hand hygiene with ABHR |
||
| 18. Document procedure and findings according to agency policy. | Timely documentation ensures patient safety. | ||
| 19. Evaluate patient response to medication. | It is important to evaluate the therapeutic effect of the medication and assess for adverse effects. | ||
| Data source: ATI, 2015b; Berman & Snyder, 2016; Brookside Associates, 2015b; Clayton et al., 2010; National Institute of Health Clinical Center, 2015; Ogston-Tuck, 2014b; Perry et al., 2014 | |||
Critical Thinking Exercises
- Why should a health care provider rotate sites with a heparin SC injection, but only rotate within a site with insulin SC injections?
- What are three risks associated with administering insulin and heparin subcutaneously?