11.4: Pain Management
- Page ID
- 52473
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Pain management requires collaboration with the interdisciplinary team, including nurses, health care providers, pharmacists, and sometimes pain specialists. There are many different types of pain medications (called analgesics) that can be administered by various routes. Analgesics are classified as nonopioids, opioids, or adjuvants. An adjuvant is a medication that has been found in clinical practice to have either an independent analgesic effect or additive analgesic properties when administered with opioids. Examples of adjuvant medications include antidepressants (e.g., amitriptyline) and anti-seizure medications (e.g., gabapentin).
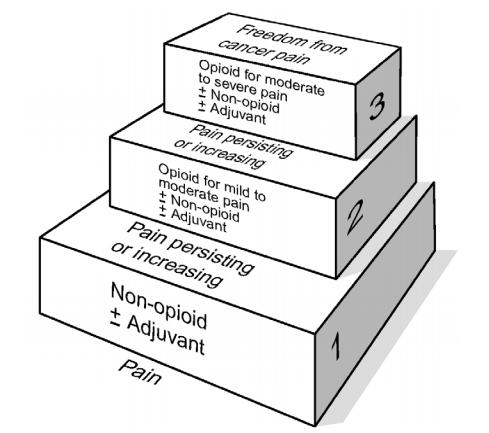
A general rule of thumb when administering analgesics is to use the lowest dose of medication, with fewest potential side effects and the least invasive route of administration, to effectively treat the level of pain as reported by the patient. The WHO ladder was originally developed by the World Health Organization for selecting analgesics for patients with cancer pain, but it can be broadened to illustrate this rule of thumb for managing pain appropriately for all patients. See Figure 11.6[1] for an image of the WHO ladder.
For example, if a patient reports a pain level of “2,” then a nurse typically starts at the lowest rung of the WHO ladder and administers a prescribed nonopioid via the oral route. If the nonopioid is not effective, then a prescribed adjuvant medication may be administered, or the nurse may decide to step up a rung on the ladder and administer a prescribed oral opioid for mild to moderate pain. On the other hand, if a patient reports severe pain, the nurse may start at the top rung of the ladder and administer a prescribed opioid for moderate to severe pain via the intravenous route for rapid relief.
Nonopioid Analgesics
Nonopioid analgesics include acetaminophen and NSAIDs.
Acetaminophen
Acetaminophen (Tylenol) is used to treat mild pain and fever but does not have anti-inflammatory properties. Acetaminophen is safe for all ages and can be administered using various routes, such as orally, rectally, and intravenously. Many over-the-counter (OTC) medications contain acetaminophen, along with other medications. See Figure 11.7[2] for an image of acetaminophen (Tylenol) and acetaminophen and diphenhydramine (Tylenol PM).
A potential severe side effect of acetaminophen is hepatotoxicity (severe liver damage). Severe liver damage may occur if an adult patient takes more than 4,000 mg of acetaminophen in 24 hours (or 3,200 mg for older adults or 2,000 mg for chronic alcoholics) or consumes three or more alcoholic drinks every day while using acetaminophen.
Because some medications are combined with acetaminophen or are prescribed “as needed,” the nurse must calculate the cumulative dose of acetaminophen over the previous 24-hour period before administering an additional dose. For example, Percocet 5/325 contains a combination of oxycodone 5 mg and acetaminophen 325 mg and may be prescribed as “1-2 tablets every 4-6 hours as needed for pain.” If two tablets are truly administered every four hours over a 24-hour period, this would add up to 3,900 mg of acetaminophen, exceeding the recommended guidelines for a geriatric patient, with the potential for causing liver damage.

NSAIDs
Nonsteroidal anti-inflammatories (NSAIDs) provide mild to moderate pain relief and also reduce fever and inflammation by inhibiting the production of prostaglandins. They can also be used as an adjuvant with opioids for severe pain. Examples of NSAIDs include ibuprofen, naproxen, and ketorolac. All NSAIDs, except aspirin, increase the risk of heart attack, heart failure, and stroke, with the risk being higher if the patient takes more than is directed or takes it for longer than directed. Common side effects include dyspepsia, nausea, and vomiting, so it is helpful to administer this medication with food. Older adults and those taking NSAIDs concurrently with other drugs, such as warfarin or corticosteroids, are at elevated risk for gastrointestinal bleeding. Renal failure can also occur with NSAIDs.
- Ibuprofen (Motrin) is safe for infants 6 months or older. It is typically prescribed every 6 to 8 hours.
- Naproxen (Naprosyn) is longer-acting than ibuprofen and is typically prescribed 2 or 3 times a day with a full glass of water.
- Ketorolac (Toradol) is commonly used to treat “breakthrough” pain that occurs during the treatment of severe acute pain already being treated with opioids. It is indicated for the short-term management (up to 5 days in adults) of moderate to severe acute pain that requires analgesia at the opioid level. Ketorolac is safe for adults, but the dosage should be reduced for patients ages 65 and over.
Read about nonopioid medications in the “Analgesic and Musculoskeletal” chapter in Open RN Nursing Pharmacology.
View a supplementary video on “How Do Pain Relievers Work?“
Opioid Analgesics
Opioids are used to treat moderate to severe pain and work by blocking the release of neurotransmitters involved in the processing of pain. Different opioids have different amounts of analgesia, ranging from codeine used to treat mild to moderate pain, up to morphine, used to treat severe pain and considered to be at the top of the WHO ladder. See Table 11.4a for a summary of common opioids. As always, check a drug reference for current dosage ranges before administering medications.
Table 11.4a Common Opioid Analgesics
| Generic Name | Trade Name(s) | Route | Adult Dosages |
|---|---|---|---|
| Codeine with acetaminophen | Tylenol #3 | PO | 30 mg/300 mg |
| Hydrocodone with acetaminophen | Lortab, Norco, Vicodin | PO | 5 mg/300 mg or 325 mg
10 mg/320 mg or 325 mg 5mg/500 mg |
| Oxycodone (immediate release and extended release)
OR Oxycodone with acetaminophen |
Oxycodone IR & OxyContin (ER)
Percocet & Roxicet |
PO
PO |
5 mg – 10 mg
5 mg/325 mg |
| Fentanyl | Duragesic, Sublimaze | Transdermal
IM IV |
12 mcg – 100 mcg/hr
0.5 – 1 mcg/kg 0.5 – 1 mcg/kg |
| Hydromorphone | Dilaudid | PO
Rectal SubQ, IM, & IV |
4 – 8 mg
3 mg 1.5 mg (may be increased) |
| Morphine | Duramorph, MS Contin, Oramorph SR, & Roxanol | PO & Rectal
SubQ, IM, & IV |
30 mg (may be increased)
4 – 10 mg (may be increased) |
Morphine is also commonly used to treat cancer pain and end-of-life pain because there is no “ceiling effect,” meaning the higher the dose, the higher the level of analgesia. Morphine is administered via various routes of administration, including orally, rectally, subcutaneously, intramuscularly, and intravenously. See Figure 11.8[3] for an image of a vial of morphine for injection or intravenous use.

Other types of opioids can be administered through the skin, such as the fentanyl transdermal patch. See Figure 11.9[4] for an image of a fentanyl transdermal patch.

Read more about analgesics and opioid medications in the “Analgesic and Musculoskeletal” chapter in the Open RN Nursing Pharmacology textbook.
Alternative Routes of Administration of Opioids
Analgesic medications can be administered via several routes, including orally, rectally, subcutaneously, and intravenously. Intramuscular routes are typically avoided. Other routes of administration include patient-controlled analgesia (PCA), intrathecally, and by epidural.
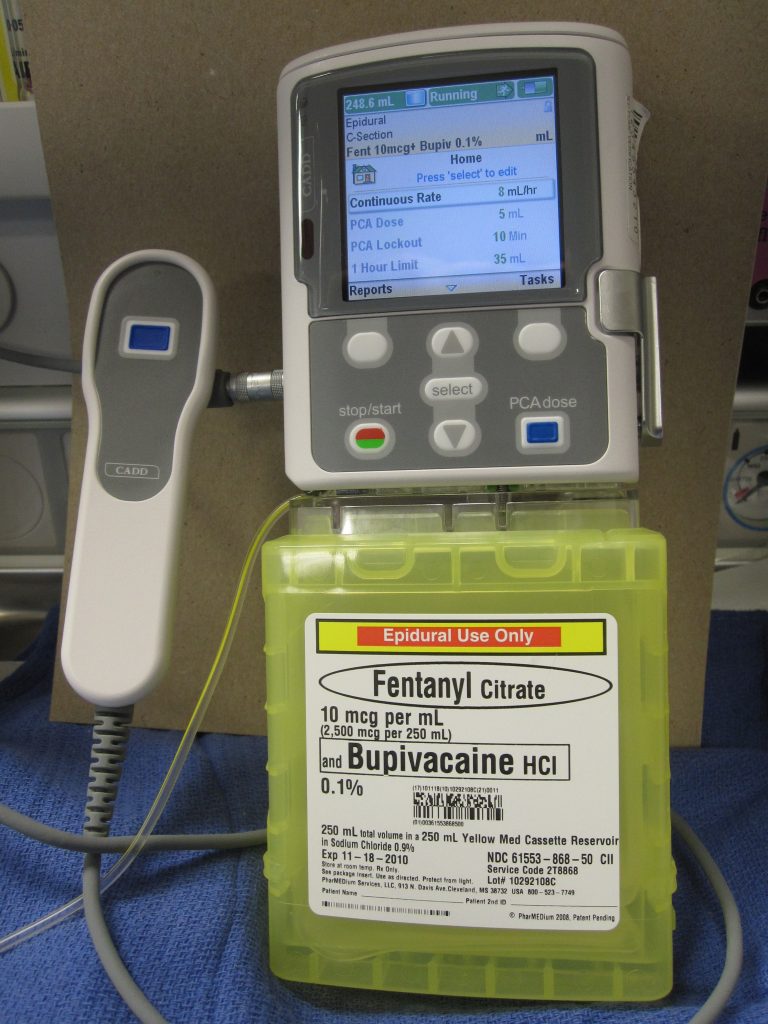
Patient Controlled Analgesia
Patient-controlled analgesia (PCA) is a method of pain management that allows hospitalized patients with severe pain to safely self-administer opioid medications using a programmed pump according to their level of discomfort. See Figure 11.10[5] for an image of a PCA pump. A computerized pump contains a syringe of pain medication and is connected directly to a patient’s intravenous (IV) line. Pain medication includes morphine, hydromorphone, and fentanyl. Doses of medication can be self-administered as needed by the patient by pressing a button. However, the pump is programmed to only allow administration of medication every set number of minutes with a maximum dose of medication every hour. These pump settings, and the design of the system requiring the patient to be alert enough to press the button, are safety measures to prevent overmedication that can cause sedation and respiratory depression. For this reason, no one but the patient should press the button for administration of medication (not even the nurse.)
In other cases, the PCA pump delivers a small, continuous flow of pain medication intravenously with the option of the patient self-delivering additional medication as needed, according to the limits set on the pump.
To document the amount and frequency of pain medication the patient is receiving, as well as to prevent drug diversion, the settings on the pump are checked at the end of every shift as part of the bedside report. The incoming and outgoing nurses double-check and document the pump settings, the amount of medication administered during the previous shift, and the amount of medication left in the syringe.
Intrathecal Pump
Another type of pump used to deliver pain medication is the intrathecal pump. This pump is surgically implanted under the skin and delivers small quantities of pain medication, such as morphine, directly into the spinal fluid. It is used to treat pain and muscle spasticity when other methods have not effectively treated the pain. It is typically used for patients with severe chronic pain, such as cancer pain, back pain, or nerve pain. However, the FDA urges cautious use because it has received numerous Medical Device Reports (MDRs) describing adverse events with implanted pumps. These reports describe pump failures, dosing errors, and other potential safety issues. Patient symptoms described in these reports include pain, opioid withdrawal, fever, vomiting, muscle spasm, cognitive changes, weakness, and cardiac and respiratory distress.[6]
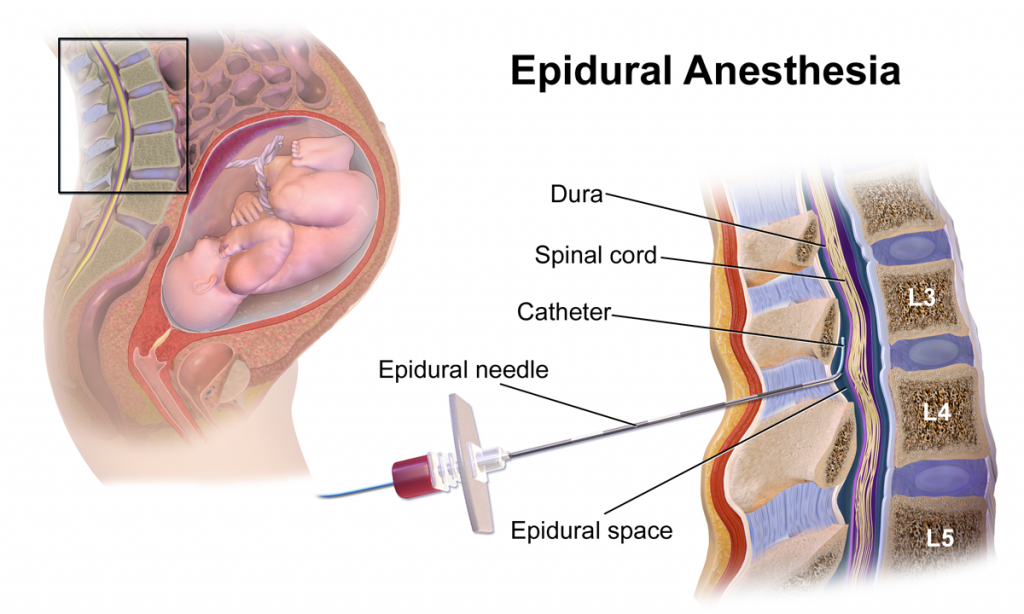
Epidural
A third route of alternative administration of pain medication is epidural anesthesia. See Figure 11.11[7] for an image of an epidural anesthesia. Morphine is administered into the spinal fluid via an epidural catheter for severe pain management associated with surgical procedures or during labor and delivery. It is also used to treat chronic pain that has not responded to other treatments. Epidural administration of 5 mg of morphine provides adequate postoperative analgesia for up to 24 hours.[8]
Adverse Effects of Opioids
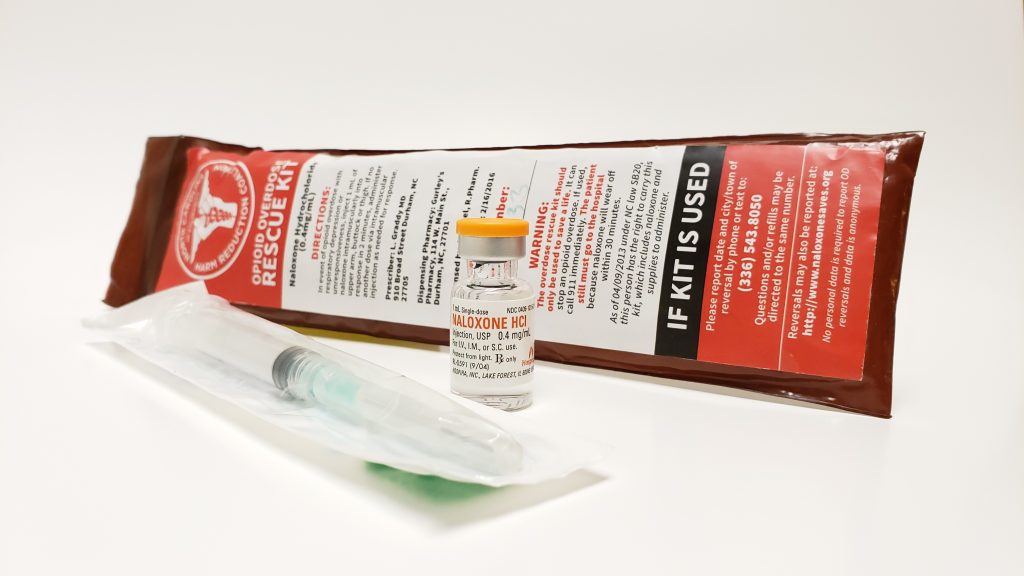
Respiratory Depression
The most serious potential adverse effect of opioids is respiratory depression. Respiratory depression is usually preceded by sedation. The nurse must carefully monitor patients receiving opioids for oversedation, which results in decreased respiratory rate. Patients at greatest risk are those who have never received an opioid and are receiving their first dose, those receiving an increased dose of opioids, or those taking benzodiazepines or other sedatives concurrently with opioids. If a patient develops opioid-induced respiratory depression, the opioid is reversed with naloxone (Narcan) that immediately reverses all analgesic effect.[9] See Figure 11.12[10] for an image of a naloxone rescue kit to treat respiratory depression caused by opioids.
Opioids can cause several other common adverse effects, such as constipation, nausea and vomiting, urinary retention, and pruritus (itching).
Constipation
Opioids slow peristalsis and cause increased reabsorption of fluid into the large intestine, resulting in slow-moving, hard stools. Nurses play an important role in preventing constipation for all patients taking opioids. A bowel management program should be initiated with the first dose and continued until the opioid is discontinued. A stool softener (such as docusate) is typically prescribed initially as part of the bowel management program. If needed, a stimulant laxative, such as sennoside (Senna), bisacodyl, or Milk of Magnesia may be added to maintain a normal bowel pattern. However, stimulants should not be taken long-term because they can be addictive. Patients taking opioids should be encouraged to increase fluid and fiber intake and ambulate, as appropriate.[11]
Nausea and Vomiting
Nausea and vomiting can occur with opioid administration due to several factors, such as the slowing of gastrointestinal mobility, constipation, or stimulation of the vestibular system. Tolerance will develop to these adverse effects within a few days. Treatment includes antiemetics, such as compazine or ondansetron.[12]
Urinary Retention
Urinary retention is common in opioid-naive patients or when opioids are delivered via the spinal route. Urinary catheterization may be required if the patient is unable to void. Tolerance to this effect occurs within a few days.[13]
Pruritus
Pruritus (itching) may occur, especially when opioids are administered via the spinal route. Antihistamines, such as diphenhydramine (Benadryl), may be used to treat pruritus, but the patient should be monitored for potential sedative effects of this medication.[14]
Adjuvant Medications
Adjuvants are medications that are not classified as analgesics but have been found to contribute to analgesic effects, especially when used in addition to opioids. Two common examples of adjuvant medications are amitriptyline and gabapentin.
Amitriptyline
Amitriptyline is a tricyclic antidepressant that is also believed to be effective in treating neuropathic pain, such as diabetic neuropathy, postherpetic neuralgia, or post‐stroke pain. The mechanism of action of amitriptyline in the treatment of neuropathic pain remains uncertain, although it is known to inhibit both serotonin and noradrenaline reuptake. It is usually administered at bedtime in an attempt to reduce any sedative effects during the day.[15]
Gabapentin
Gabapentin is an anticonvulsant that is also effective in treating neuropathic pain and restless leg syndrome. Patients taking gabapentin should be warned that their mental health may change in unexpected ways or they may become suicidal. Nurses should implement fall precautions for patients taking gabapentin because it can cause sleepiness, weakness, and unsteadiness.[16]
Nonpharmacological Interventions
Nonpharmacological interventions can be used with or without pharmacologic interventions and often provide tremendous benefits to the patient. A variety of techniques can be selected by the patient that best fit their needs and goals. Nonpharmacological interventions should be documented in the plan of care and their effectiveness evaluated in terms of their ability to meet the patient’s goals for pain relief. Table 11.4b provides examples of several types of nonpharmacological interventions.
Table 11.4b Nonpharmacological Interventions
| Intervention | Examples |
|---|---|
| Distraction | Describing photos, telling jokes, and playing games |
| Relaxation | Rhythmic breathing, meditation, prayer, imagery, and music therapy |
| Basic comfort measures | Proper positioning and therapeutic environment
Avoiding sudden movement Reducing pain stimuli within the environment |
| Cutaneous stimulation | Acupuncture and acupressure
Massage: 3-5 minutes offers benefits Transcutaneous Electrical Nerve Stimulation (TENS) unit: a specialized stimulator placed over the area of pain |
| Application of heat or cold | Heat: vasodilation increases blood flow; duration should be 5-20 minutes based on patient tolerance
Cold: vasoconstriction reduces blood flow; cold numbs nerve sensations; duration should be no longer than 20 minutes Cool baths and moist, cool compresses |
| Mind-body therapies | Biofeedback
Meditation and mindfulness |
| Aromatherapy | Lotions and moisturizing cream
Avoiding strong smells |
| Exercise | Physical activity
Tai chi Yoga |
| Therapy | Physical therapy
Occupational therapy |
See Figure 11.13[17] for images of various nonpharmacological interventions.

Patients may also consider using complementary health approaches to manage chronic pain. Complementary approaches include acupuncture, massage therapy, meditation, relaxation techniques, spinal manipulation, Tai Chi, yoga, and dietary supplements. Read more about complementary approaches using the hyperlink provided in the following box.
Read The Joint Commission document on “Non-pharmacologic and non-opioid solutions for pain management.”
Read more about complementary approaches to treat pain from the National Center for Complementary and Integrative Health.
Read about pain management for older adults from the University of Iowa.
- World Health Organization. (1996). Cancer pain relief (2nd ed.). http://apps.who.int/iris/bitstream/handle/10665/37896/9241544821.pdf;jsessionid=08444506DC35A33288AD7C0DE6D34667?sequence=1↵
- “Extra_Strength_Tylenol_and_Tylenol_PM.jpg” by Ragesoss is licensed under CC BY-SA 4.0↵
- “Morphine_vial.JPG” by Vaprotan is licensed under CC BY-SA 3.0↵
- “Fentanyl_Transdermal_System_50_mcg_Patch.jpg” by User:Crohnie is licensed under CC BY-SA 3.0↵
- “PCA-01.JPG” by DiverDave is licensed under CC BY-SA 3.0↵
- U.S. Food & Drug Administration. (2018, November 14). Use caution with implanted pumps for intrathecal administration of medicines for pain management: FDA safety communication. https://www.fda.gov/medical-devices/safety-communications/use-caution-implanted-pumps-intrathecal-administration-medicines-pain-management-fda-safety↵
- “Epidural_Anesthesia.png” by BruceBlaus is licensed under CC BY-SA 4.0↵
- This work is a derivative of StatPearls by Martinez-Velez and Singh and is licensed under CC BY 4.0↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care(ELNEC). https://www.aacnnursing.org/ELNEC↵
- “Opiod_Rescue_Kit_3.jpg” by Intropin (Mark Oniffrey) is licensed under CC BY_SA 4.0↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care(ELNEC). https://www.aacnnursing.org/ELNEC↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care(ELNEC). https://www.aacnnursing.org/ELNEC↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care(ELNEC). https://www.aacnnursing.org/ELNEC↵
- American Association of Colleges of Nursing. (n.d.). End-of-Life-Care(ELNEC). https://www.aacnnursing.org/ELNEC↵
- Moore, R. A., Derry, S., Aldington, D., Cole, P., & Wiffen, P. J. (2015). Amitriptyline for neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2015(7). https://doi.org/10.1002/14651858.CD008242.pub3↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); Gabapentin; [updated 2021, Jan 22; reviewed 2020, May 15; cited 2021, Feb 16]. https://medlineplus.gov/druginfo/meds/a694007.html↵
- “Massage-hand-4.jpg” by Lubyanka is licensed under CC BY-SA 3.0, “Biofeedback_training_program_for_post-traumatic_stress_symptoms.jpg” by Army Medicine is licensed under CC BY 2.0, “Tai_Chi1.jpg” by Craig Nagy is licensed under CC BY-SA 2.0, “Musicoterapia_lmidiman_flickr.jpg” by Midiman is licensed under CC BY 2.0, “Cold_Hot_Pack.jpg” by Mamun2a is licensed under CC BY-SA 4.0, “pexels-photo-1188511.jpeg” by Mareefe is licensed under CC0, “STOTT-PILATES-reformer-class.jpg” by MHandF is licensed under CC BY-SA 3.0, “prayer-2544994_960_720.jpg” by Himsan is licensed under CC0, “gaming-2259191_960_720.jpg” by JESHOOTS-com is licensed under CC0↵


