15.6: Applying the Nursing Process
- Page ID
- 52501
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The nursing process is used continuously when caring for individuals who have fluid, electrolyte, or acid-base imbalances, or at risk for developing them, because their condition can change rapidly. This systematic approach to nursing care ensures that subtle cues or changes are not overlooked and that appropriate outcomes and interventions are implemented according to the patient’s current condition.
Assessment
A thorough assessment provides valuable information about a patient’s current fluid, electrolyte, and acid-base balance, as well as risk factors for developing imbalances. Performing a chart review or focused health history is a good place to start collecting data, with any identified gaps or discrepancies verified during the physical assessment. It is also important to consider pertinent life span or cultural considerations that impact a patient’s fluid and electrolyte status.
Subjective Assessment
Subjective assessment data is information obtained from the patient as a primary source or family members or friends as a secondary source. This information must be obtained by interviewing the patient or someone accompanying the patient. Some of this information can be obtained through a chart review, but should be verified with the patient or family member for accuracy.
Subjective data to obtain includes age; history of chronic disease, surgeries, or traumas; dietary intake; activity level; prescribed medications and compliance with taking medications; pain; and bowel and bladder functioning. Subjective assessment data is helpful to determine normal pattern identification and risk identification. For example, a history of kidney disease or heart failure places the patient at risk for fluid volume excess, whereas diuretic use places the patient at risk for fluid volume deficit and electrolyte and acid-base imbalances. A history of diabetes mellitus also places a patient at risk for fluid, electrolyte, and acid-base imbalances. Recognizing these risks helps nurses be prepared for complications that may arise and allows the nurse to recognize subtle cues as problems develop.
Objective Assessment
Objective assessment data is information that the nurse directly observes. This data is obtained through a physical examination using inspection, auscultation, and palpation. A complete head-to-toe assessment should be performed to avoid missing clues to the patient’s condition.
Focused assessments such as trends in weight, 24-hour intake and output, vital signs, pulses, lung sounds, skin, and mental status are used to determine fluid balance, electrolyte, and acid-base status.
- Accurate daily weights can provide important clues to fluid balance. Weights must be taken on the same scale, at the same time of day, with the patient wearing similar clothing in order to be accurate. A one kilogram change in weight in 24 hours is considered significant because this represents a one liter fluid gain or loss and should be reported to the provider.
- Accurate measurement of 24-hour intake and output helps validate weight findings. Averaged urine output of less than 30 mL/hour or 0.5mL/hr/kg of concentrated urine should be reported to the provider.
- Vital signs should be analyzed. An elevated blood pressure and bounding pulses are often seen with fluid volume excess. Decreased blood pressure with an elevated heart rate and a weak or thready pulse are hallmark signs of fluid volume deficit. Systolic blood pressure less than 100 mm Hg in adults, unless other parameters are provided, should be reported to the health care provider.
- Lung crackles can signify fluid volume excess and are often first auscultated in the lower posterior lung fields.
- Tight, edematous, shiny skin indicates fluid volume excess. See Figure 15.15[1] for an image of edema. Conversely, skin tenting, dry mucous membranes, or dry skin indicate fluid volume deficit.
- New mental status changes such as confusion or decreased level of consciousness can indicate fluid, electrolyte, or acid-base imbalance, especially hypo- or hypernatremia, acid-base imbalances, or fluid volume deficit.
- Cardiac arrhythmias can be seen with acid-base imbalances and electrolyte imbalances, especially with hypo- or hyperkalemia and alkalosis. See Table 15.6a for a comparison of expected and unexpected findings and those that require notification of a health care provider.

| Assessment | Expected Findings | Unexpected Findings Indicating Excessive Fluid Volume
*Bolded items are critical conditions that require immediate health care provider notification. |
Unexpected Findings Indicating Deficient Fluid Volume |
|---|---|---|---|
| Vital signs | Blood pressure, heart rate, and oxygen saturation levels within normal limits | Elevated blood pressure, increased respiratory rate, or decreased oxygen saturation | Decreased blood pressure or elevated heart rate |
| Neurological | Alert and oriented | Headache | Headache, confusion, decreased level of consciousness, dizziness, or weakness |
| Cardiac | Normal heart rate and rhythm, capillary refill <3 seconds, and normal pulses | Bounding pulses, S3 heart sound, or jugular venous distention | Weak, thready pulses; sluggish capillary refill; or chest pain |
| Respiratory | Clear lung sounds throughout, normal respiratory rate, and no shortness of breath | Crackles in lung fields, pink frothy sputum, shortness of breath, or respiratory distress | Shortness of breath possible |
| Gastrointestinal | Bowel sounds present x4 quadrants and normal stool consistency and frequency for patient | Constipation with dry, hard stools | |
| Urinary | Clear urine, normal urine specific gravity, and urine output greater than 30 ml/hr | Decreased urine output <30 mL/hr or < 0.5 mL/kg/hr concentrated urine | Decreased urine output <30 mL/hr or <0.5 mL/kg/hr concentrated urine, or elevated urine specific gravity |
| Integumentary | Normal skin turgor and moist mucous membranes | Tight, edematous, or shiny skin | Tenting (poor skin turgor); dry, sticky mucous membranes; or dry skin |
| Weight | <1kg change in weight over 24 hours | >1kg increase over 24 hours | >1kg decrease over 24 hours |
Review additional details about assessing these body systems in Open RN Nursing Skills.
Diagnostic and Lab Work
Diagnostic tests and lab work provide important information about fluid status, electrolyte, and acid-base balance and should be used in conjunction with a thorough subjective and objective assessment to form a complete picture of the patient’s overall status. It is important to cluster diagnostic and lab assessment data with subjective and objective assessment data to ensure a complete assessment picture. This will help ensure correct information is reported to the provider as necessary.
Lab work provides important clues to overall fluid status. Common lab tests used to evaluate fluid status include serum osmolarity, urine specific gravity, hematocrit, and blood urea nitrogen (BUN).
Serum osmolarity (often interchanged with the term serum osmolality) measures the concentration of particles in the blood with a normal range of 275 to 295 mmol/kg). Normal value ranges may vary slightly among different laboratories. In healthy people, when serum osmolality in the blood becomes high, the body releases antidiuretic hormone (ADH). This hormone causes the kidneys to reabsorb water, resulting in dilution of the blood and the return of serum osmolarity to normal range. An elevated serum osmolarity level means the blood is more concentrated than normal and often indicates deficient fluid volume deficit. A decreased serum osmolarity means the blood is more dilute than normal and may indicate a fluid volume excess.[3]
Urine osmolarity measures the concentration of particles in the urine. An increased urine osmolarity result means the urine is concentrated and can indicate fluid volume deficit. A decreased urine osmolarity result means the urine is dilute and can indicate excess fluid intake.[4] Urine specific gravity is a urine test that commonly measures hydration status by measuring the concentration of particles in urine. Normal urine specific gravity levels are between 1.010 and 1.020. A urine specific gravity above 1.020 indicates concentrated urine and can indicate a fluid volume deficit, similarly to an elevated urine osmolarity. A urine specific gravity below 1.010 indicates dilute urine, which can occur with excessive fluid intake.[5]
When a condition called “Excessive Fluid Volume” occurs, altered physiological mechanisms impact the kidney’s ability to increase urine output to eliminate excessive fluid volume, causing urine output to decrease. As a result, the serum osmolarity decreases as fluid is retained but the urine specific gravity is elevated because urine is concentrated.
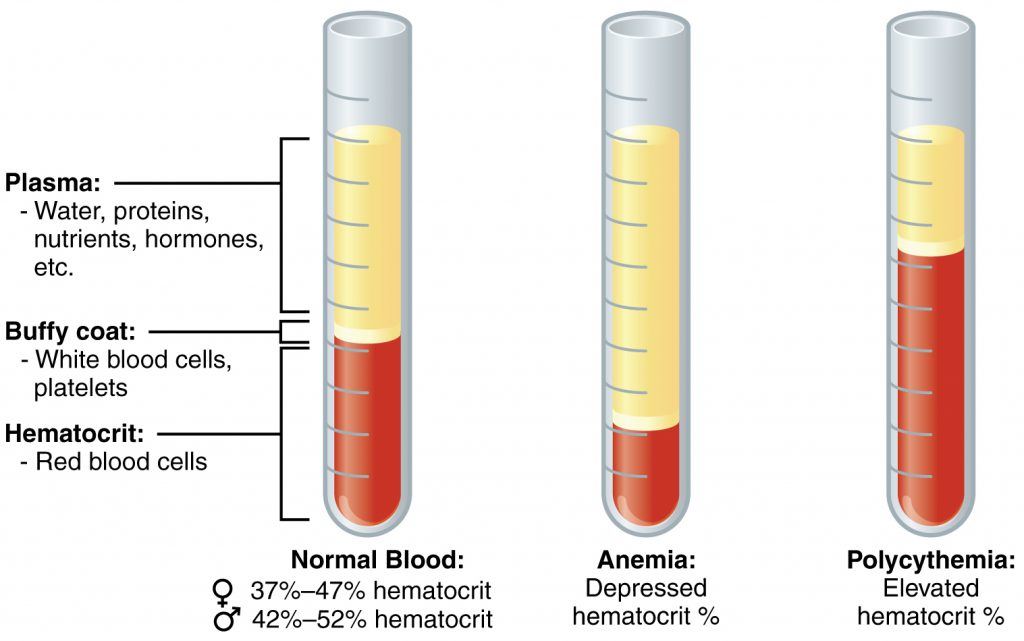
Hematocrit (HCT) is a blood test that measures how much of your blood is made up of red blood cells compared to the liquid component of blood called plasma. It is often part of a complete blood count (CBC), a routine test that measures different components of your blood. The normal hematocrit for men is 42 to 52%; for women it is 37 to 47%, but these ranges may vary slightly across labs.
In addition to measuring red blood cells, hematocrit levels can also be used to evaluate fluid balance. When deficient fluid volume is occurring, the plasma component of the blood also decreases, causing an elevated concentration of red blood cells (and an elevated hematocrit). In this case, drinking more fluid or receiving intravenous fluids will bring the hematocrit level back to normal range. Conversely, if a patient is experiencing “Excessive Fluid Volume,” the plasma component of the blood is increased, causing dilution of the red blood cells and a decreased hematocrit level.[6],[7] See Figure 15.16[8] for an illustration of normal hematocrit, elevated hematocrit, and decreased hematocrit due to fluid imbalance.
Blood Urea Nitrogen (BUN) measures the amount of urea nitrogen in your blood. BUN and serum creatinine levels are used to evaluate kidney function, with increased levels indicating worsening kidney function. In general, the normal BUN range is 7 to 20 mg/dL, but normal ranges vary depending on the reference range used by the lab and the patient’s age. Patients with “Deficient Fluid Volume” can also have elevated BUN levels for the same reason that hematocrit is affected; as plasma levels decrease, the blood becomes more concentrated.
In addition to monitoring lab work for results indicating fluid imbalance, electrolytes, specifically sodium, potassium, calcium, phosphorus, and magnesium, should be monitored closely for patients at risk. Refer to Table 15.4 in the “Electrolytes” section for an overview of electrolyte imbalances, common symptoms, and common treatments.
Additional diagnostic tests used to evaluate for signs of fluid and electrolyte imbalances are the chest X-ray and the electrocardiogram. A chest X-ray evaluates for fluid in the lungs, a common complication of excessive fluid volume. An electrocardiogram (ECG) evaluates for cardiac complications resulting from electrolyte imbalances.
Arterial blood gases are used to closely monitor critically ill patients, such as patients in diabetic ketoacidosis or in severe respiratory distress. ABG results provide important clues about respiratory status, oxygenation, and metabolic processes occurring in the body. See Table 15.6b for a summary of laboratory findings associated with fluid, electrolyte, and acid-base imbalances.
| Lab Value | Normal Ranges |
|---|---|
| Serum osmolarity | 275 to 295 mmol/kg |
| Urine Specific Gravity | 1.010 and 1.020 |
| Hematocrit | Men: 42 to 52%
Women: 37 to 47% |
| BUN | 7 to 20 mg/dL |
| Serum sodium | 135-150 mEq/L |
| Serum potassium | 3.5-5 mEq/L |
| Serum magnesium | 1.5-2.4 mEq/L |
| Serum calcium | 8.5-10.3 mg/dL |
| Serum phosphorus | 2.5-4 mg/dL |
| ABG | pH: 7.35 and 7.45
PaO2: 80-100 mm Hg HCO3: 22-26 mEq/L PaO2: 35-45 mm Hg |
Life Span Considerations
There are several life span considerations when assessing for fluid, electrolyte, and acid-base balance.
Newborns and Infants
Newborns and infants have a large proportion of water weight compared to adults, with approximately 75% of weight being water. During the first week after birth, extracellular fluid is lost in urine along with sodium. Additionally, compensatory mechanisms such as the Renin-Angiotensin-Aldosterone System are less developed, and newborn kidneys are less able to concentrate urine, resulting in a decreased ability to retain sodium. Newborns and infants also have a greater body surface area, making them more susceptible to insensible fluid losses through the skin and lungs via evaporation. This causes increased risk of developing hyponatremia and fluid volume deficit. In contrast, newborns are less able to excrete potassium, placing them at risk for hyperkalemia.[9] Episodes of vomiting and diarrhea also place infants at an increased risk of quickly developing fluid and electrolyte disturbances.
When monitoring urine output in infants, parents are often asked about the number of wet diapers in a day. Nurses may also weigh diapers for hospitalized infants for more accurate measurement of urine output.
Children and Adolescents
Children and adolescents are at risk for dehydration when physically active in hot environments causing excessive sweating. Illnesses causing diarrhea, vomiting, or fever can also quickly cause fluid deficit if there is little fluid intake to replace the water and sodium lost. For this reason, it is important to educate parents regarding the importance of fluid intake when their child is sweating or ill.[10]
Older Adults
Older adults are at risk for fluid and electrolyte imbalances for a variety of reasons, including surgery, chronic diseases such as heart and kidney disease, diuretic use, and decreased mobility that limits the ability to obtain hydration. They also have a decreased thirst reflex, which contributes to decreased fluid consumption. Kidney function naturally decreases with age, resulting in decreased sodium and water retention, as well as decreased potassium excretion. These factors place older patients at risk for fluid volume deficit and electrolyte abnormalities.[11]
Diagnoses
There are many nursing diagnoses applicable to fluid, electrolyte, and acid-base imbalances. Review a nursing care planning resource for current NANDA-I approved nursing diagnoses, related factors, and defining characteristics. See Table 15.6c for commonly used NANDA-I diagnoses associated with patients with fluid and electrolyte imbalances.[12]
| NANDA-I Diagnosis | Definition | Defining Characteristics |
|---|---|---|
| Excess Fluid Volume | Surplus intake and/or retention of fluid. | Adventitious breath sounds
Elevated blood pressure Altered mental status Anxiety Decreased hematocrit, serum osmolarity, and BUN Dyspnea Edema Fluid intake exceeds output Jugular vein distension Restlessness Weight gain >1 kg/24 hours |
| Deficient Fluid Volume | Decreased intravascular, interstitial, and/or intracellular fluid. This refers to dehydration, water loss alone without change in sodium. | Altered mental status
Decreased skin turgor Decreased blood pressure Decreased urine output Dry skin and mucous membranes Increased heart rate Increased serum osmolarity, hematocrit, and BUN Increased urine concentration Sudden weight loss Thirst Weakness |
| Risk for Imbalanced Fluid Volume | Susceptible to a decrease, increase, or rapid shift from one to the other of intravascular, interstitial, and/or intracellular fluid, which may compromise health. This refers to body fluid loss, gain, or both. | Diarrhea
Vomiting Excessive fluid volume Insufficient fluid volume |
| Risk for Electrolyte Imbalance | Susceptible to changes in serum electrolyte levels, which may compromise health. | Diarrhea
Vomiting Excessive fluid volume Insufficient fluid volume |
Excess Fluid Volume Example
A patient with heart failure has been hospitalized with an acute exacerbation with dyspnea and increased edema in the lower extremities. A sample PES statement is, “Fluid Volume Excess related to a compromised regulatory mechanism as evidenced by edema, crackles in lower posterior lungs, and weight gain of 2 kg in 24 hours.”
Deficient Fluid Volume Example
An elderly patient develops severe diarrhea due to food poisoning and is admitted to the hospital with dehydration. A sample PES statement is, “Deficient Fluid Volume related to insufficient fluid intake as evidenced by blood pressure 90/60, dry mucous membranes, decreased urine output, and an increase in hematocrit.”
Risk for Imbalanced Fluid Volume Example
A patient who is ten weeks pregnant has developed severe vomiting due to severe morning sickness. A sample PES statement is, “Risk for Imbalanced Fluid Volume as evidenced by vomiting.” The nurse plans to educate the patient about tips to stay hydrated despite vomiting, as well as when to contact the provider if signs of dehydration develop.
Risk for Electrolyte Imbalance Example
A patient with chronic kidney disease is prescribed a diuretic to control fluid retention. A sample PES statement is, “Risk for Electrolyte Imbalance as evidenced by insufficient knowledge of modifiable factors.” The nurse plans to educate the patient about signs and symptoms of fluid and electrolyte imbalance and when to contact the provider.
Note: Recall that risk diagnoses do not contain related factors in PES statements because a vulnerability for a potential problem is being identified for the patient. Instead, the phrase “as evidenced by” is used to refer to the evidence of risk that exists. Read more about formulating PES statements in the “Nursing Process” chapter.
Outcome Identification
Goals for a patient experiencing fluid, electrolyte, or acid-base imbalances depend on the chosen nursing diagnosis and specific patient situation. Typically, goals should relate to resolution of the imbalance. For example, if the nursing diagnosis is Excess Fluid Volume, then an appropriate goal would pertain to resolution of the fluid volume excess. Remember that goals are broad and outcomes should be narrowly focused and written in SMART format (Specific, Measurable, Achievable, Realistic, and Time Oriented).
For the nursing diagnosis of Excess Fluid Volume, an overall goal is, “Patient will achieve fluid balance.” Fluid balance for a patient with Excess Fluid Volume is indicated by body weight returning to baseline with no peripheral edema, neck vein distention, or adventitious breath sounds.[14] An example of a SMART outcome is, “The patient will maintain clear lung sounds with no evidence of dyspnea over the next 24 hours.”
For patients experiencing Electrolyte Imbalances, an appropriate goal is, “Patient will maintain serum sodium, potassium, calcium, phosphorus, magnesium, and/or pH levels within normal range.” An additional goal is, “The patient will maintain a normal sinus heart rhythm with regular rate,” because many electrolyte imbalances impact the electrical conduction system of the heart and this is a life-threatening complication.
Planning Interventions
Evidence-based interventions should be planned according to the patient’s history and specific fluid, electrolyte, or acid-base imbalance present. Refer to a nursing care planning resource for evidence-based interventions for specific nursing diagnoses. Table 15.6d lists selected interventions for key imbalances.[15],[16],[17],[18]
| Nursing Diagnosis | Interventions |
|---|---|
| Excessive Fluid Volume |
|
| Deficient Fluid Volume |
|
| Risk for Electrolyte Imbalance |
|
Read more about medications affecting fluid and electrolyte balance, such as diuretics, in the “Cardiovascular and Renal System” chapter in Open RN Nursing Pharmacology.
Read about intravenous fluids used to treat Fluid Volume Deficit in the “IV Therapy Management” chapter in Open RN Nursing Skills.
Implement Interventions Safely
Patients with fluid and electrolyte imbalances can quickly move from one imbalance to another based on treatments received. It is vital to reassess a patient before implementing interventions to ensure current status warrants the prescribed intervention. For example, a patient admitted with Fluid Volume Deficit received intravenous fluids (IV) over the past 24 hours. When the nurse prepares to administer the next bag of IV fluids, she notices the patient has developed pitting edema in his lower extremities. She listens to his lungs and discovers crackles. The nurse notifies the prescribing provider, and the order for intravenous fluids is discontinued and a new order for diuretic medication is received.
Therefore, assessments for new or worsening imbalances should be performed prior to implementing interventions:[20]
- Monitor daily weights for sudden changes. A weight change of greater than 1 kg in 24 hours (using the same scale and type of clothing) should be reported to the provider.
- Monitor location and extent of edema using the 1+ to 4+ scale to quantify edema.
- Monitor intake and output over a 24-hour period; note trends of decreasing urine output in relation to fluid intake indicating potential development of Fluid Volume Excess.
- Monitor lab work such as serum osmolarity, serum sodium, BUN, and hematocrit for abnormalities. (For example, a patient receiving IV fluids may develop Fluid Volume Excess, resulting in decreased levels of serum osmolarity, serum sodium, BUN, and hematocrit. Conversely, a patient receiving IV diuretics can quickly become dehydrated, resulting in elevated levels of serum osmolarity, serum sodium, BUN, and hematocrit.)
- For patients receiving intravenous fluids, monitor for the development of excessive fluid volume. Monitor lung sounds for crackles and ask about the presence of dyspnea. Report new abnormal findings to the provider.
- For patients receiving diuretic therapy, monitor for fluid volume deficit and electrolyte imbalances such as hypokalemia and hyponatremia.
Implement fall precautions for patients with orthostatic hypotension, restlessness, anxiety, or confusion related to fluid imbalances.
Evaluation
The effectiveness of interventions implemented to maintain fluid balance must be continuously evaluated. Evaluation helps the nurse determine whether goals and outcomes are met and if interventions are still appropriate for the patient. If outcomes and goals are met, the plan of care can likely be discontinued. If outcomes and goals are not met, they may need to be revised. It is also possible that interventions may need to be added or revised to help the patient meet their goals and outcomes. Table 15.6e provides a list of assessment findings indicating imbalances are improved.
| Imbalance | Signs and Symptoms of Improvement |
|---|---|
| Fluid Volume Excess | Decreased crackles, decreased edema, decreased shortness of breath, and/or improved jugular venous distention |
| Fluid Volume Deficit | Increased blood pressure, decreased heart rate, normal skin turgor, and/or moist mucous membranes |
| Electrolyte Imbalances | Electrolyte levels return to normal and/or absence of signs or symptoms of deficit or excess |
| Acid-Base Imbalance | ABGs return to normal or baseline, resolution of vomiting or diarrhea, and/or no respiratory distress |
- “Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0↵
- El-Sharkawy, A. M., Sahota, O., Maughan, R. J., & Lobo, D. N. (2014). The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clinical Nutrition, 33(1), 6-13. https://doi.org/10.1016/j.clnu.2013.11.010↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Osmolality blood test; [updated 2021, February 8]. https://medlineplus.gov/ency/article/003463.htm↵
- RnCeus.com. (n.d.). Serum and urine osmolality. https://www.rnceus.com/renal/renalosmo.html↵
- Flasar, C. (2008). What is urine specific gravity? Nursing2008, 38(7), 14. https://doi.org/10.1097/01.nurse.0000325315.41513.a0.↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); Hematocrit test; [updated 2020, Jul 31; reviewed 2020, Jul 31; cited 2021, Feb 11]. https://medlineplus.gov/lab-tests/hematocrit-test/↵
- Billett, H. H. (1990). Hemoglobin and hematocrit. In Walker H. K., Hall W. D., Hurst J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK259/↵
- “1901_Composition_of_Blood.jpg” by Arabic is licensed under CC BY 3.0↵
- Ringer, S. (2020). Fluid and electrolyte therapy in newborns. UpToDate. https://www.uptodate.com/contents/fluid-and-electrolyte-therapy-in-newborns↵
- Iglesia, I., Guelinckx, I., De Miguel-Etayo, P. M., González-Gil, E. M., Salas-Salvadó, J., Kavouras, S. A., Gandy, J., Martínez, H., Bardosono, S., Abdollahi, M., Nasseri, E., Jarosz, A., Ma, G., Carmuega, E., Thiébaut, I., & Moreno, L. A. (2015). Total fluid intake of children and adolescents: cross-sectional surveys in 13 countries worldwide. European Journal of Nutrition, 54, 57–67. https://doi.org/10.1007/s00394-015-0946-6↵
- El-Sharkawy, A. M., Sahota, O., Maughan, R. J., & Lobo, D. N. (2014). The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clinical Nutrition, 33(1), 6-13. https://doi.org/10.1016/j.clnu.2013.11.010↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 182-186. ↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 182-186. ↵
- Ackley, B., Ladwig, G., Makic, M. B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier. pp. 360-363, 406-416. ↵
- Ackley, B., Ladwig, G., Makic, M. B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier. pp. 360-363, 406-416. ↵
- Fluid overload. (2021). Lippincott advisor. http://advisor.lww.com↵
- Dehydration. (2021). Lippincott advisor. http://advisor.lww.com↵
- Electrolyte imbalance. (2021). Lippincott advisor. http://advisor.lww.com↵
- Centers for Disease Control and Prevention. (2017). Assessment - measuring orthostatic blood pressure. cdc.gov/steadi/pdf/Measuring_Orthostatic_Blood_Pressure-print.pdf↵
- Ackley, B., Ladwig, G., Makic, M. B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier. pp. 360-363, 406-416. ↵


