1.42: Surgical Drainage of Neck Abscesses
- Page ID
- 17681
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
SURGICAL DRAINAGE OF NECK ABSCESSES
Johan Fagan, Jean Morkel
Neck abscesses can be difficult to drain and have fatal consequences if not timeously diagnosed, accurately localized and promptly incised and drained. Yet the management is commonly left in the hands of surgical trainees.
This chapter presents the relevant surgical anatomy and surgical approaches to the different fascial spaces of the head and neck. Because fascial planes both direct and confine spread of sepsis, it is important to have an understanding of the fascial planes and fascial spaces of the head and neck.
Classification of Cervical Fasciae
- Superficial cervical fascia (Figures 1, 2)
- Deep cervical fascia (Figures 2-4)
- Superficial (investing) layer
- Middle layer
- Muscular layer
- Visceral layer
- Deep layer
- Alar fascia
- (Pre)vertebral fascia
Superficial Cervical Fascia

Figure 1: Delicate superficial cervical fascia overlying external jugular vein and fat following division of platysma over the lateral neck
This very thin, delicate fascia is found just deep to the skin and envelopes the muscles of the head and neck including platysma and the muscles of facial expression. It is so thin that it may be difficult to identify when incising the neck. It extends from the epicranium above to the axillae and upper chest below and includes the superficial musculoaponeurotic system/SMAS. The space deep to the superficial cervical fascia contains fat, vessels (e.g. anterior and external jugular veins), nerves and lymphatics and is by definition not a deep neck space (Figure 1). Abscesses located either superficial to or within the tissue space immediately deep to the superficial cervical fascia are treated by simple incision and drainage.
Deep Cervical Fascia (Figures 2-4)
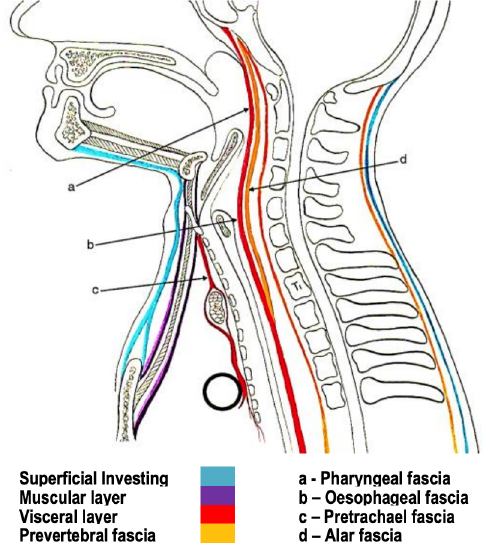
Figure 2: Sagittal view of 3 layers of deep cervical fascia
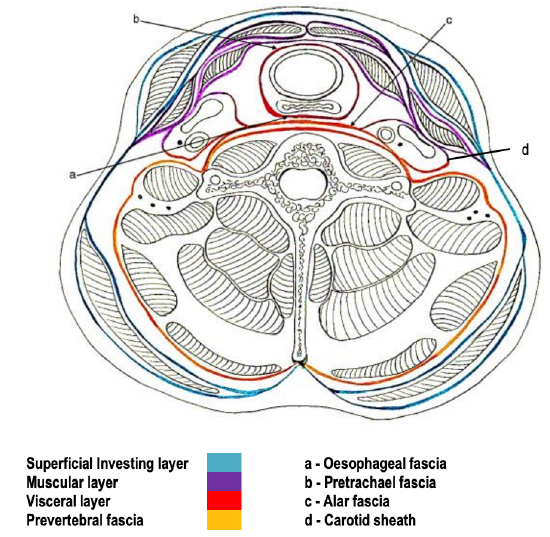
Figure 3: Infrahyoid cross-section of deep cervical fasciae
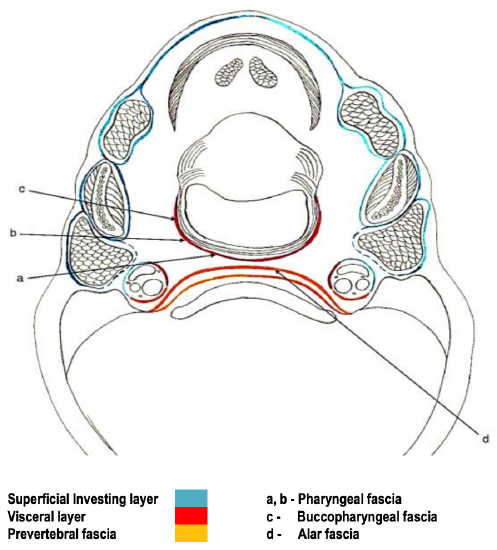
Figure 4: Suprahyoid cross-section of deep cervical fasciae
This envelopes the deep neck spaces; hence an understanding of its anatomy is key to managing deep neck sepsis. It comprises 3 layers i.e. superficial, middle, and deep.
Deep Cervical Fascia: Superficial layer (Figures 2-5)
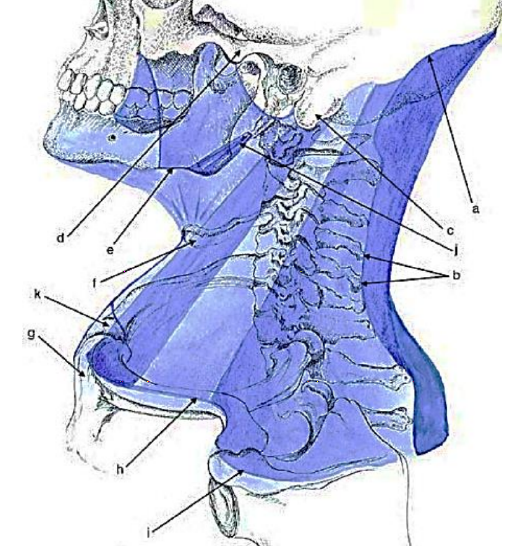
Figure 5: Attachments of superficial layer of deep cervical fascia
The superficial layer, also known as the investing layer, surrounds the neck and envelopes the muscles of mastication i.e. masseter, buccinator, digastric and mylohyoid (Figures 4, 5).
The attachments of the superficial layer of deep cervical fascia are as follows (Figure 5):
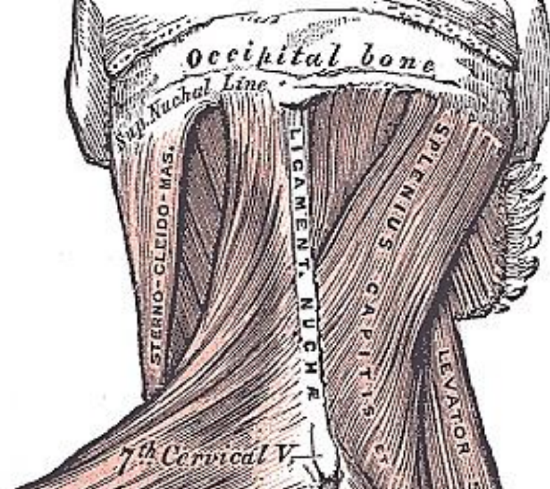
Figure 6: The superficial/investing layer of deep cervical fascia attaches to superior nuchal line and ligamentum nuchae
a) Superior nuchal line of occipital bone (Figures 2, 6)
b) Posteriorly merges with ligamentum nuchae, a midline intermuscular extension of the supraspinous ligament (Figures 2, 3, 6).
c) Mastoid processes of temporal bones
d) Zygomatic arches
e) Inferior border of mandible
f) Hyoid bone
g) Manubrium sterni
h) Clavicles
i) Acromion
j) Forms stylomandibular ligament
k) Fascia parts just above manubrium sterni to contain anterior jugular veins, and attaches to anterior and posterior surfaces of the manubrium (Figure 2)
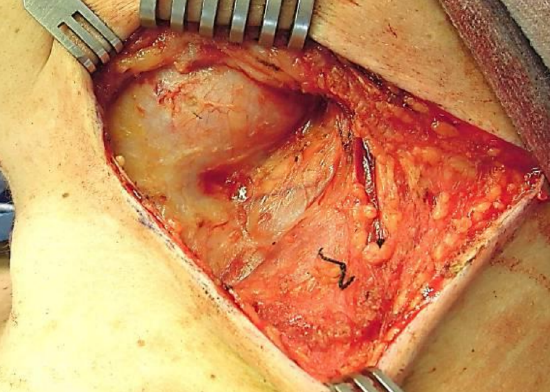
Figure 7: The superficial/investing layer of deep cervical fascia covers the submandibular gland and the lateral aspect of the major vessels as part of the outer surface of carotid sheath, and the sternocleidomastoid muscle
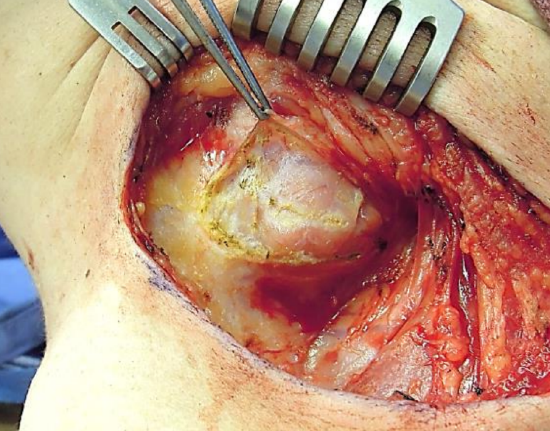
Figure 8: Submandibular capsule incised to demonstrate its thin capsule
The fascia splits into superficial and deep layers to enclose trapezius and sternocleidomastoid (Figure 3). It also encapsulates the submandibular and parotid glands (Figures 4, 7, 8), and contributes to the carotid sheath (Figure 3).
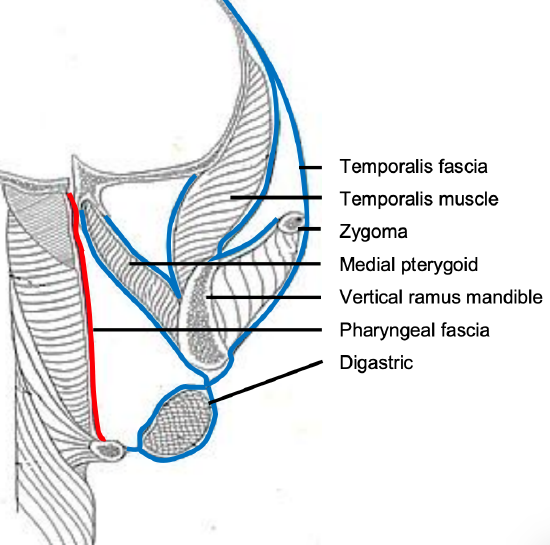
Figure 9: Coronal view of superficial (investing) layer (blue) surrounding masticator muscles (visceral fascia: red)
Between the ramus of the mandible and the hyoid bone it envelopes the anterior belly of the digastric muscle (Figure 9). The superficial layer of deep cervical fascia therefore defines the parotid, submandibular and masticator spaces and contributes to the wall of the carotid space (Figures 4, 7).
Deep Cervical Fascia: Middle layer
The middle layer of deep cervical fascia extends superiorly from the skull base along the carotid sheath to the pericardium (Figures 2, 3, 10). It has muscular and visceral layers:
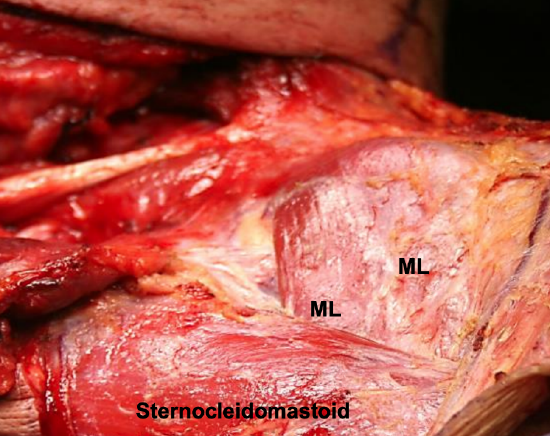
Figure 10: Muscular layer (ML) of middle layer of deep cervical fascia overlying the infrahyoid strap muscles

Figure 11: Thin carotid sheath being elevated off the internal jugular vein
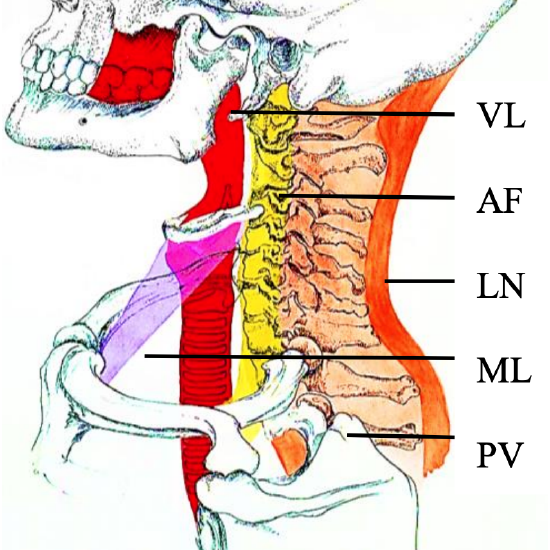
Figure 12: Middle and deep layers of deep cervical fascia: Visceral layer (VL), Alar Fascia (AF), Ligamentum Nuchae (LN), Muscular layer (ML), and Prevertebral Fascia (PV)
- Muscular layer (Figures 2, 3, 10, 11, 12): It envelopes the infrahyoid strap muscles (sternohyoid, sternothyroid, omohyoid, thyrohyoid), the carotid artery and internal jugular vein (carotid sheath and carotid space)
- Visceral layer (Figures 2, 3, 4, 9, 12): It lies deep to the infrahyoid muscles, and splits to enclose thyroid, trachea, pharynx and esophagus
Deep Cervical Fascia: Deep Layer
This encircles the prevertebral and paraspinal muscles, and also contributes to the carotid sheath. It is divided into prevertebral and alar fasciae.
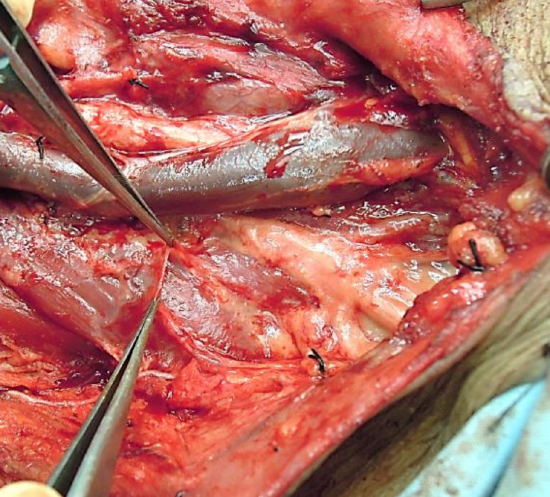
Figure 13: The thin prevertebral fascia that covers the prevertebral muscles and brachial plexus
- Prevertebral fascia (a.k.a. vertebral fascia) (Figures 2, 3, 4, 12, 13): This attaches to the vertebral bodies in the midline, and extends laterally over the prevertebral muscles to attach to the transverse processes of the vertebrae, and then envelops the paraspinal muscles to meet with the superficial layer of deep cervical fascia at the ligamenttum nuchae in the midline posteriorly (Figures 3, 12). It extends from the base of the skull to T3 (Figure 12). It covers the floor of the posterior traingle of the neck; inferiorly it constitutes the fascial covering over the brachial plexus from where it extends laterally as the axillary sheath to encase the axillary vessels and brachial plexus (Figure 13).
- Alar fascia (Figures 1, 2, 3, 12): This fascia is interposed between the prevertebral and visceral fasciae and forms the posterior wall of the retropharyngeal/retrovisceral space. It extends between the transverse processes from the skull base to the superior mediastinum where it merges with the visceral layer of deep fascia on the posterior surface of the esophagus at the level of T2, thereby terminating the retropharyngeal space inferiorly (Figure 2).
Classification of Deep Neck Spaces
The deep fasciae create clinically relevant deep neck spaces, some of which interconnect with one another. Some are potential spaces and become apparent only when distended by pus or air (surgical emphysema). The terminology and classifications of deep neck spaces used in the literature are not entirely consistent.
Working from cephalad-to-caudad the deep neck spaces may be grouped as follows:
I. Facial region
a. Buccal space
b. Canine space
c. Masticator space
i. Masseter space
ii. Pterygoid space
iii. Temporal space
d. Parotid space
II. Suprahyoid region
a. Sublingual space
b. Submental space
c. Submandibular space
d. Ludwig’s Angina (IIa + IIb +IIc)
e. Parapharyngeal space
f. Peritonsillar space
III. Infrahyoid region: Pretracheal space
IV. Entire Neck
a. Retropharyngeal space
b. Danger Space
c. Carotid Space
d. Prevertebral Space
Dental numbering systems
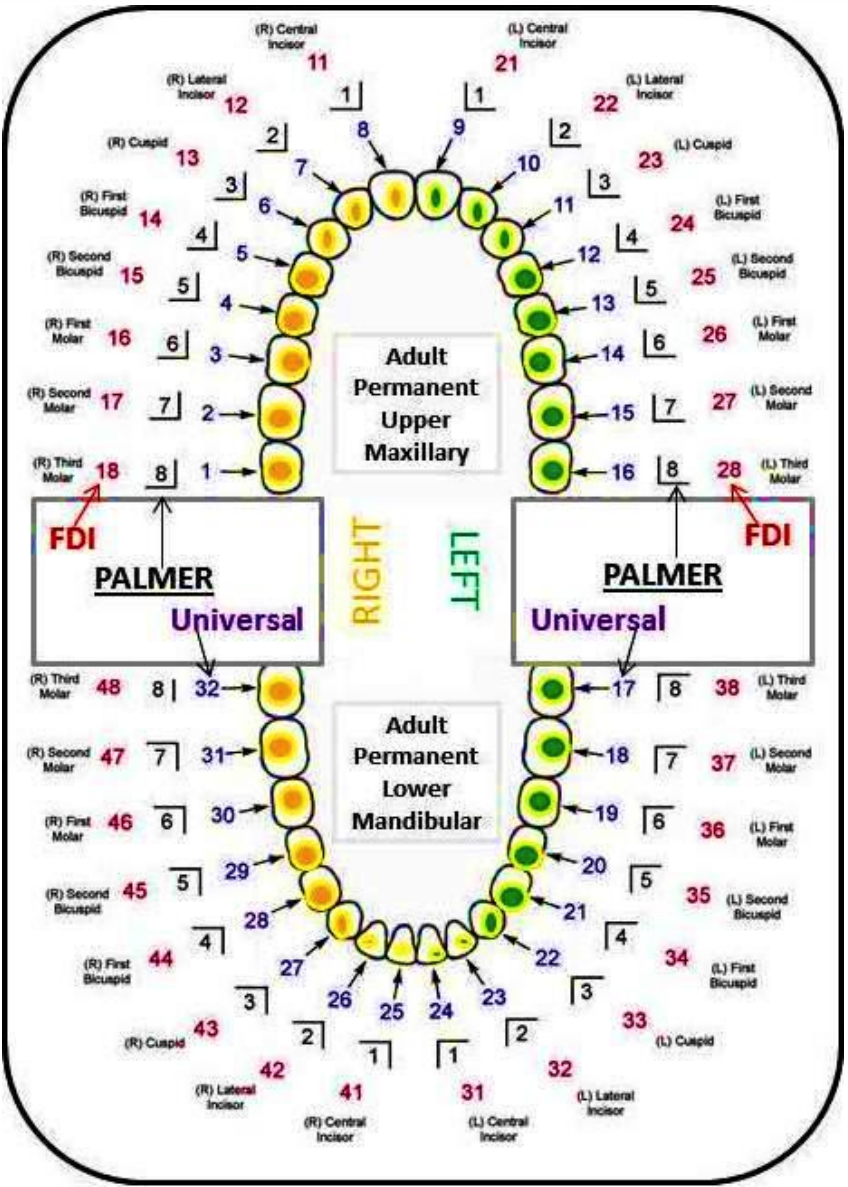
Figure 14: Three dental numbering systems
Fascial space infections are often of odontogenic origin. Hence it is important to know how to number the teeth, especially when interpreting radiology reports. Three different numbering systems are used in dentistry (Figure 14).
Surgical drainage deep neck spaces
I.a. Buccal Space Abscess
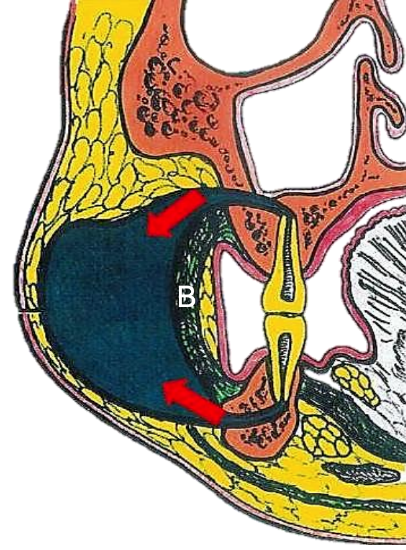
Figure 15: Buccal space abscess; note how dental sepsis drains above and below the buccinator muscle (B)
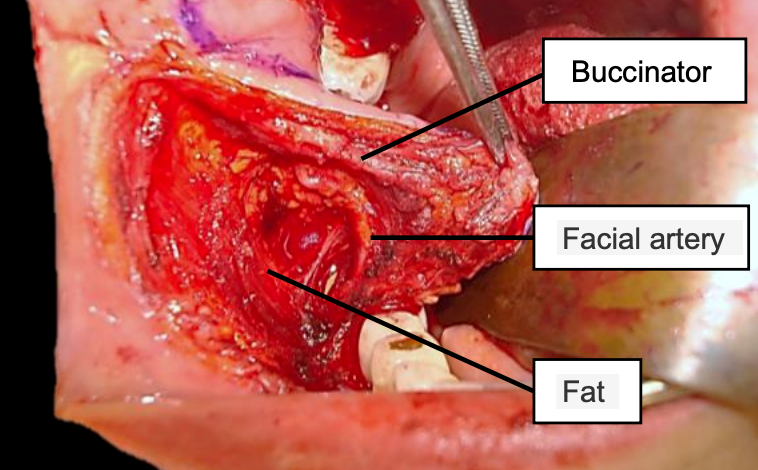
Figure 16: Right buccal space exposed during elevation of buccinator flap; Note buccinator muscle, facial artery and the fat which contains the terminal branches of the facial nerve
The buccal space is confined laterally by the superficial cervical fascia just deep to the skin, medially by the investing layer of cervical fascia that overlies the buccinator muscle, anteriorly by the labial musculature, posteriorly by the pterygomandibular raphe, superiorly by the zygomatic arch and inferiorly by the lower border of the mandible (Figure 15). It contains buccal fat, Stenson’s duct, terminal branches of the facial nerve, and the facial artery and veins (Figure 16).

Figure 17: Buccal space abscess with marked swelling of the cheek and minimal trismus
Buccal space sepsis is principally of odontogenic origin in adults (Figure 15); this includes the maxillary bicuspid and molar teeth and even the mandibular equivalents. However buccal space sepsis in children may have non-odontogenic causes as well. The infection is easily diagnosed as there is often marked cheek swelling, trismus is not severe (Figure 17) and there are often carious bicuspid or molar teeth. More specifically the abscess manifests as loss of the nasolabial skin fold, a rounded, tender cheek swelling, and swelling of the lower eyelid (Figure 17). Diagnostic needle aspiration is easily performed.

Figure 18: CT of buccal space abscess
Initial radiology should include an orthopantomograph (OPG) or Cone Beam CT (CBCT) to exclude an odontogenic causes. More advanced imaging such as contrast enhanced CT (Figure 18) or MRI may be useful in more complex cases.
Surgical approaches to the buccal space
Treat the cause, e.g. carious teeth. Transoral drainage is done just inferior to the point of fluctuance. Generally an incision is made intraorally just inferior to the opening of the parotid duct; with necessary care and using blunt dissection only into the periphery of the space, injury to branches the facial nerve is avoided. The intraoral approach does not allow for dependent drainage.
If one elects to make a more inferiorly placed external incision parallel to the inferior border of the mandible, blunt dissection should be directed superiorly and anteriorly remaining superficial to the masseter. Take care not to injure the marginal mandibular nerve, facial artery or vein.
Alternately one can place incisions in the mandibular and/or maxillary vestibules, and dissect bluntly either inferiorly (mandible) or superiorly (maxilla) through the buccinator muscle into the abscess.
I.b. Canine Space Abscess
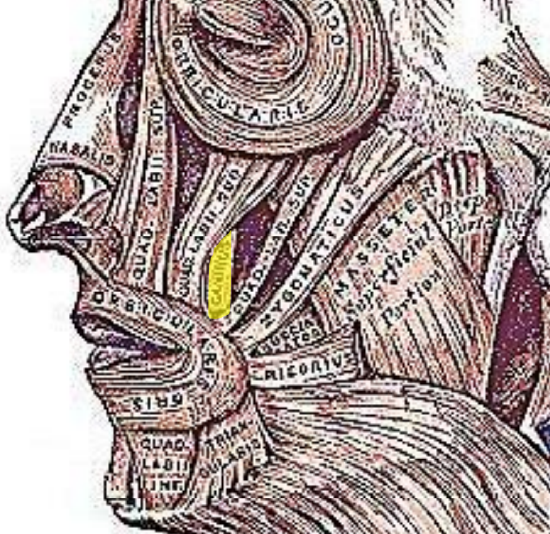
Figure 19: Levator anguli oris muscle (yellow)

Figure 20: Canine space abscess with swelling lateral to the nares and of the upper lip.

Figure 21: Canine space infection causing marked cellulitis of the eyelids

Figure 22: Sinus formation and ectroprion following canine space abscess
Whether the canine space is a true fascial space or simply a muscular apartment is a matter for debate. A canine space infection is usually caused by maxillary cuspid infection that perforates the lateral cortex of the maxilla above the insertion of the levator anguli oris muscle of the upper lip (Figure 19). The muscle’s origin is the maxillary wall high up in the canine fossa; it inserts into the angle of the mouth with the orbicularis and zygomatic muscles. If infection extends below the insertion of the levator muscle, as is more commonly found, it presents as a swelling of the labial sulcus or, less commonly, as a palatal swelling. However infection of the canine space generally presents as swelling lateral to the nares and of the upper lip (Figure 20). It may cause marked cellulitis of the eyelids (Figure 21) or drain spontaneously, creating a sinus and cause subsequent scarring (Figure 22).
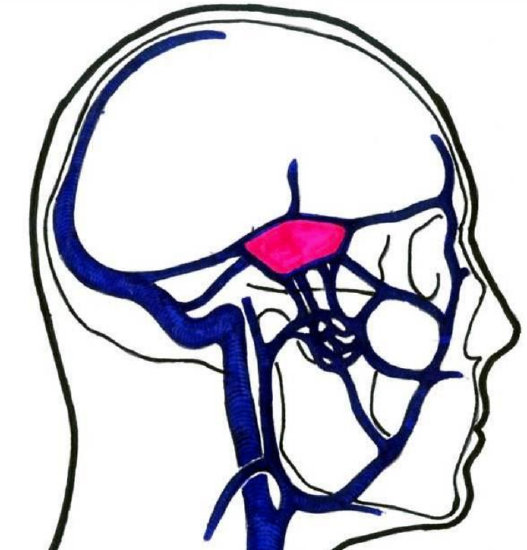
Figure 23: Septic thrombi of the angular vein may travel via the superior and inferior ophthalmic veins and cause cavernous sinus thrombosis
Septic thrombi of the angular vein may extend via the superior and inferior ophthalmic veins to the cavernous sinus and cause cavernous sinus thrombosis with the classical signs of ptosis, proptosis, chemosis and ophthalmoplegia/paresis (Cranial nerves III, IV, VI) (Figure 23).
Surgical approaches to the canine space
Drainage is normally achieved via an intraoral approach, with access high in the maxillary labial vestibule. Dissect superiorly through the levator anguli oris muscle using blunt dissection to avoid injury to the infraorbital nerve.
I.c. Masticator Space(s)
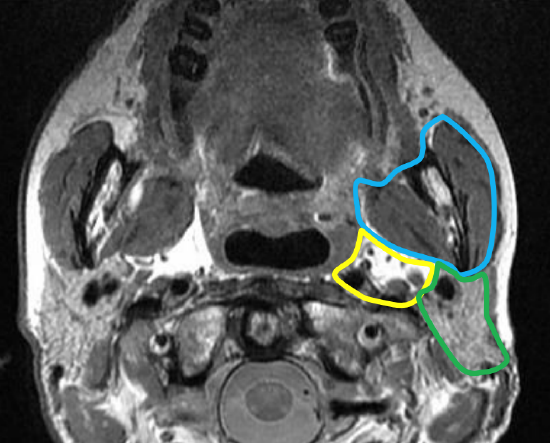
Figure 24: Masticator space (blue outline), parapharyngeal space (yellow outline) and parotid space (green outline)
The masticator space(s) is defined by the superficial (investing) layer of deep cervical fascia (Figure 9). It contains the masseter, medial and lateral pterygoids, ramus and body of the mandible, temporalis tendon, and inferior alveolar vessels and nerve. It is related superiorly to the temporal space; posteromedially to the parapharyngeal space; and posteriorly to the parotid space (Figure 24).
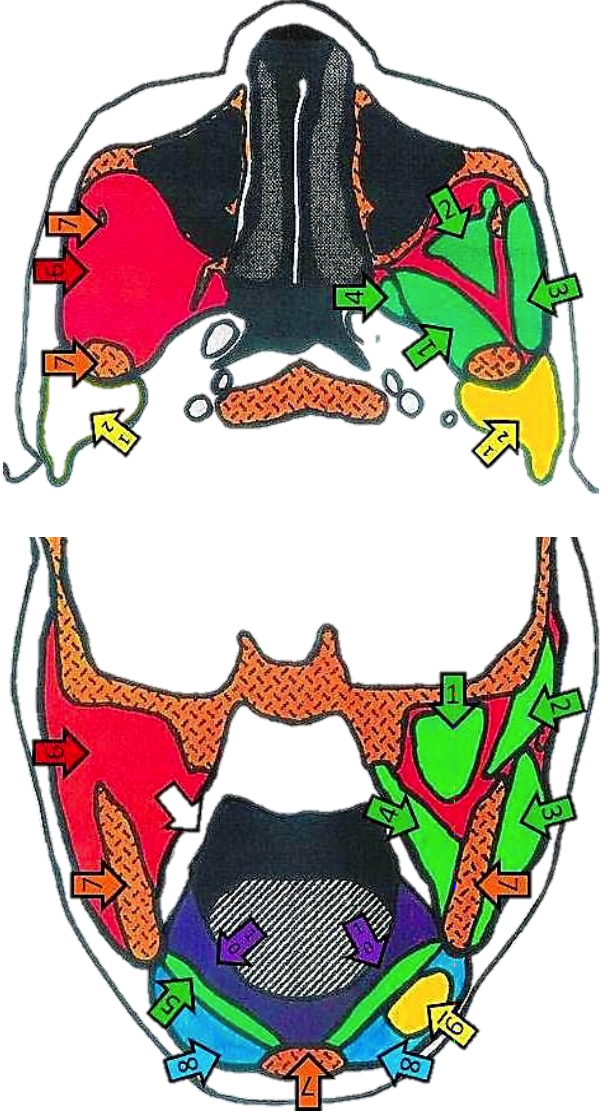
Figure 25ab: Axial and coronal views of the masticator space and relevant anatomy and other spaces: 1-Lateral Pterygoid m, 2-Temporalis m, 3-Masseter m, 4-Medial Pterygoid m, 5-Mylohyoid m, 6-Masticator space, 7-Mandible, 8-Submandibular space, 9-Submandibular gland, 10- Sublingual space, 11-Parapharyngeal space, 12-Parotid/Parotid space
The literature is not consistent about how to define the masticator space and often speaks about “masticator spaces” or a “masticator space with compartments”. The masticator space(s) has masseteric, pterygoid and temporal spaces/compartments which communicate with each other as well as with the buccal, submandibular and parapharyngeal spaces (Figures 25 a, b).

Figure 26: Needle aspiration is a valuable diagnostic tool
Sepsis is primarily of dental origin, especially from the 3rd inferior molar tooth. Infection may be confined to only one the masticator compartments or may spread to any or all the above mentioned compartments/spaces. Patients generally present with local pain and marked trismus. Needle aspiration is a valuable diagnostic tool (Figure 26).
Drainage of abscesses of the masticator spaces will next be discussed according to the individual masseteric, pterygoid and temporal spaces /compartments.
I.c.i. Masseteric Space
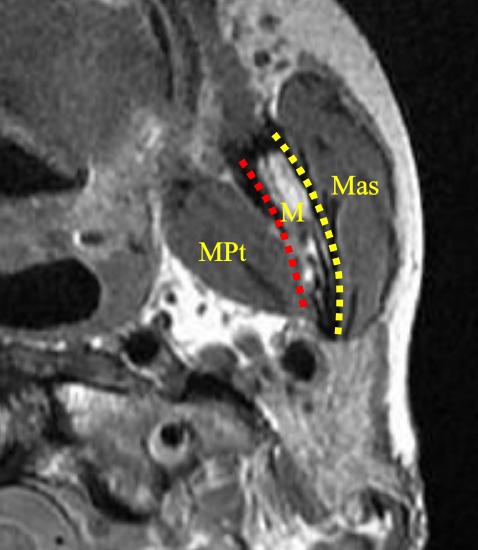
Figure 27: (Sub)masseteric space (Yellow line); pterygoid space (red line); Medial pterygoid (MPt); mandible (M); and masseter (Mas)
The masseteric (submasseteric) space is located between the masseter muscle laterally and the mandibular ascending ramus medially (Figure 27). Anteriorly, the space is bound by the inner surface of the masseteric fascia and posteriorly by the parotidomasseteric fascia as it splits to envelop the parotid gland. The superior and inferior borders are, respectively, the zygomatic arch and angle and the inferior border of the ramus where the masseter muscle is attached.

Figure 28: Masseteric space abscess with bulging of the masseter and severe trismus
Clinically patients present with bulging of the masseter muscle, severe trismus and pain (Figure 28). Due to its submasseteric location, palpation often reveals a nonfluctuant, very firm swelling.
Surgical approaches to masseteric space

Figure 29: Tongue depressors used to overcome trismus
Tongue depressors are a useful aid to overcome the severe trismus and to gain access to the mouth for intraoral local anesthetic blocks, incision and drainage procedures and even for intubation (Figure 29).
An external approach is generally employed. An incision is made at the angle of the mandible, parallel to the inferior border of the mandible. After cutting through the skin and subcutaneous tissue, blunt dissection is directed superiorly through the platysma and the submandibular space. Care should be taken to avoid injury to the mandibular branch of the facial nerve. An intraoral approach can be used via a vertical incision made along the pterygomandibular raphe; use blunt dissection lateral to the mandibular ramus and medial/deep to the masseter muscle to reach the abscess. Combined approaches can also be used. Ultrasound-guided drainage can be considered in patients with unilocular submasseteric space infection and severe trismus causing a significant anesthetic risk.
I.c.ii. Pterygoid Space

Figure 30: Left Pterygoid space abscess
The pterygoid (pterygomandibular) space consists mostly of loose areolar tissue. It is located between the pterygoid muscles and the ramus of the mandible (Figures 27, 30). Other nomenclature includes “internal pterygoid space” or “superficial pterygoid space”.
It is bound medially and inferiorly by the medial pterygoid muscle and the pterygomasseteric sling respectively. The lateral pterygoid muscle is located superomedially. The medial ramus of the mandible is located laterally. The parotid gland curves medially around the back of the mandibular ramus to form its posterior border, while anteriorly the buccinator and superior constrictor muscles join to form a fibrous junction, the pterygomandibular raphe. The pterygoid space contains the inferior alveolar nerve, artery and vein, the lingual nerve and the nerve to the mylohyoid muscle.
Sepsis of the pterygoid space is commonly due to infection of the 3rd molar tooth, or results from infection following 3rd molar surgery or mandibular orthognathic surgery; it may also follow mandibular local anesthetic blocks. Trismus and pain are often the presenting sign and symptom.
Surgical approaches to the pterygoid space
An extraoral submandibular approach is normally employed. Dissect bluntly through the pterygomasseteric sling up to the pterygoid space, remaining medial to the ramus and lateral to the medial pterygoid muscle. An intraoral approach is done via a vertical incision, lateral and parallel to the pterygomandibular raphe. Blunt dissection is then used to reach the pterygoid space by dissecting along the medial surface of the ramus. A combined approach with through-and-through drains can also be employed.
I.c.iii. Temporal Space (Figures 31, 32)
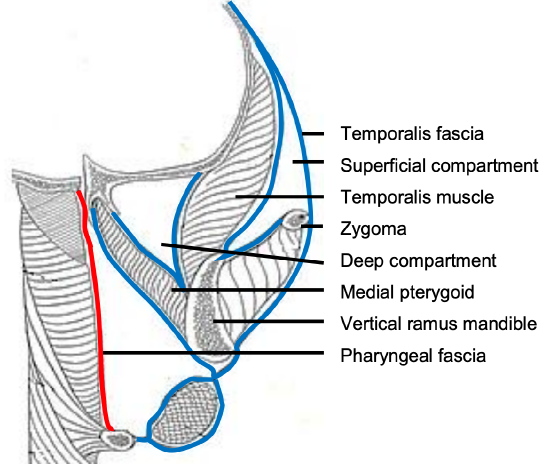
Figure 31: Deep and superficial compartments of temporal space
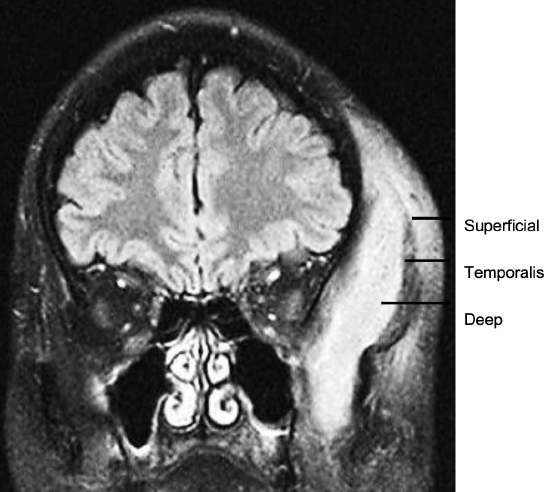
Figure 32: MRI of deep and superficial temporal space abscesses (BMJ Case Reports 2010; doi:10.1136/bcr.01.2010.2656)
The temporalis muscle partitions this space into deep and superficial compartments. The superficial compartment is contained laterally by the temporalis fascia (superficial/investing layer of deep fascia), and medially by the temporalis muscle; the deep compartment is limited laterally by the deep surface of the temporalis muscle, and medially by the periosteum overlying the temporal bone.
It contains the internal maxillary artery and its branches, the inferior alveolar artery and nerve, and is bisected by the temporalis muscle. It is related inferiorly to the masticator space. Sources of sepsis include maxillary molar infection or post-extraction sepsis; maxillary sinusitis, maxillary sinus fractures; temporomandibular arthroscopy and sepsis following injections into the temporomandibular joint.
Temporal space sepsis typically presents as swelling of the temporal fossa, pain and trismus. Contrast enhanced CT or MRI scans indicate the relations of the abscess to the temporalis muscle and extension to other spaces e.g. masticator space (Figure 32).
Surgical approaches to temporal space
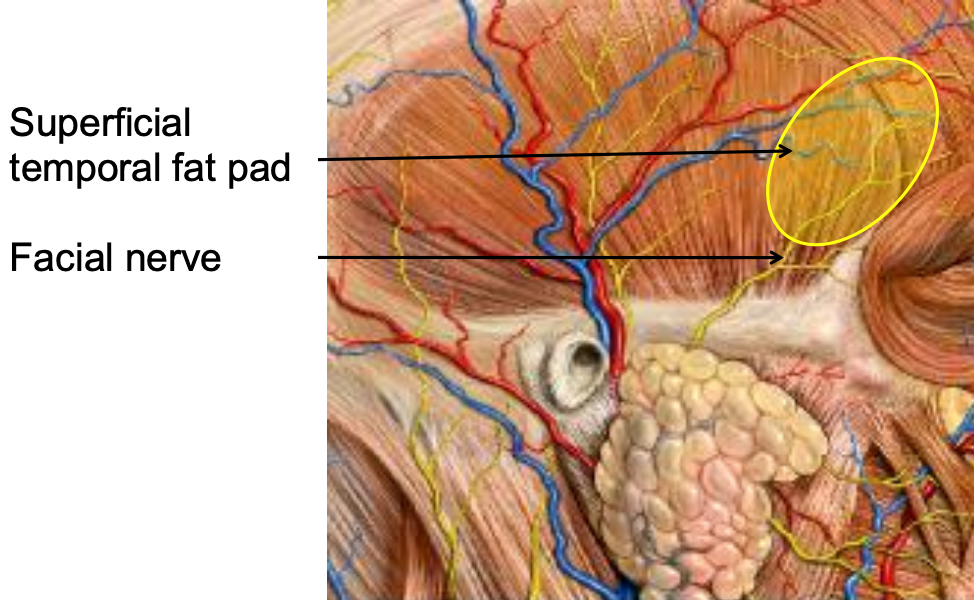
Figure 33: Facial nerve crossing zygoma

Figure 34: External approach to the superficial and deep compartments of the temporal space
External approach to superficial and deep compartments: An incision is made 3 cm lateral to the lateral canthus of the eye taking care not in injure the frontal/temporal branches of the facial nerve which run across the superficial temporal fat pad, deep to the orbicularis oculi muscle, just lateral to the orbital rim (Figure 33, 34); or by a horizontal brow incision. The deep compartment is drained by advancing a hemostat through the temporalis muscle into the space between the temporalis muscle and temporal and sphenoid bone.
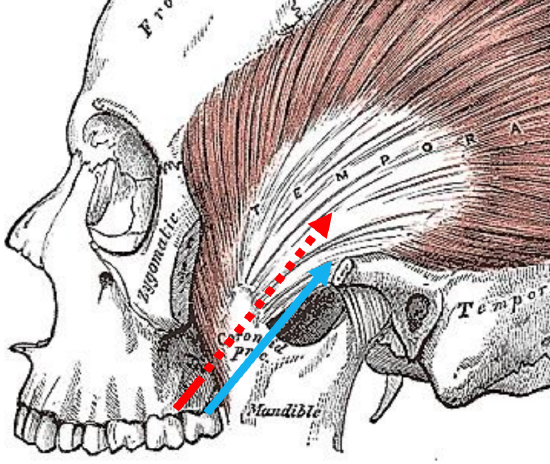
Figure 36: Intraoral drainage: Red arrow: medial to coronoid process to reach deep compartment; Blue arrow: lateral to coronoid process to reach superficial compartment
Intra-oral drainage: The temporalis muscle attaches to the coronoid process of the mandible (Figure 35). The key anatomical landmark for intraoral drainage therefore is the vertical ramus of the mandible where it ascends from the retromolar trigone. To drain the superficial compartment, make a stab incision in the mucosa lateral to vertical ramus of the mandible and advance a hemostat lateral to the coronoid process into the abscess. To drain the deep compartment, make a stab incision in the mucosa medial to the vertical ramus and advance a hemostat medial to the coronoid process into the abscess. A combined approach can also be used.
I.d. Parotid Space

Figure 36: (R) parotid space (yellow outline) and (L) parotid abscess
The parotid space is bound by the superficial (investing) layer of deep cervical fascia (Figures 24, 36). The investing fascia splits at the level of the stylomandibular ligament to enclose the gland by superficial and deep parotid capsules. The space extends from the external auditory canal to the angle of the mandible. It is located lateral to the carotid and parapharyngeal spaces and posterior to the masticator space (Figure 24). It contains the parotid gland, proximal part of the parotid duct, facial nerve, posterior facial / retromandibular vein, intraparotid lymph nodes and terminal branches of external carotid artery. The superficial capsule is strong, but the deep capsule is thin, allowing for infection to spread easily into the parapharyngeal space.

Figure 37: Parotid space abscess
Sources of sepsis include parotitis, sialadenitis and adjacent sepsis. Parotid space sepsis typically presents with tenderness, swelling, and trismus (Figure 37). Fluctuation is often absent and it may be difficult to distinguish clinically between parotitis and a parotid abscess. Ultrasound or a contrast enhanced CT scan is useful to diagnose a parotid abscess (Figure 36).
Surgical approaches to the parotid space
Injury to the facial nerve is the principle concern. Incision and drainage is done under general anesthesia by elevating a parotidectomy skin flap to expose the parotid capsule. Incisions are made in the parotid capsule along the axis of the facial nerve, a hemostat is passed bluntly into the abscess(es), and drains are inserted. Resolution of the parotid swelling is generally quite delayed.
II.a. Sublingual Space
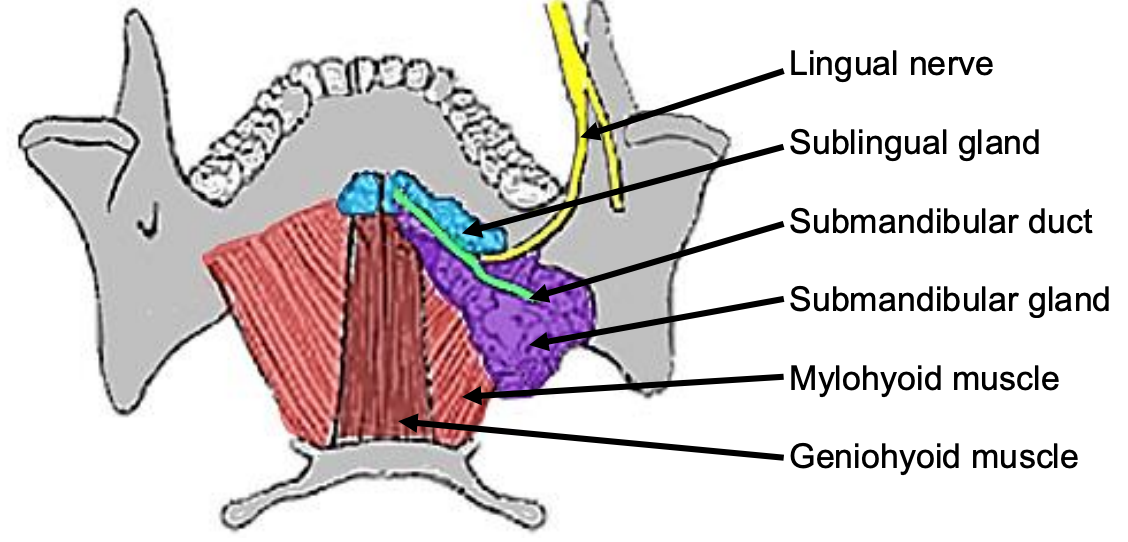
Figure 38: Superior intraoral view of SMG, duct, lingual nerve and mylohyoid and geniohyoid muscles
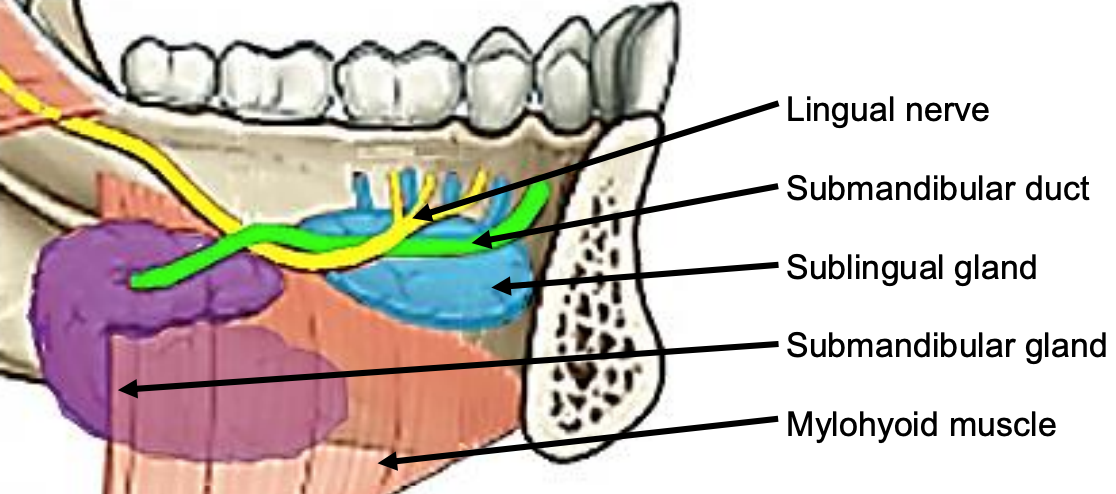
Figure 39: Intraoral view of left sublingual gland with ducts of Rivinus, SMG and duct, lingual nerve and mylohyoid muscles
The sublingual space is contained by the mucosa of the floor of the mouth above, the mylohyoid muscle below (Figures 38, 39), and is continuous with the opposite side across the midline. Anteriorly and laterally it is bound by the mandible. The posterior border is the hyoid bone. The space contains the sublingual salivary glands, intraoral components of the submandibular salivary glands and the submandibular ducts, and the hypoglossal and lingual nerves (Figures 35, 36).
The space is connected with the submandibular space at the posterior edge of the mylohyoid muscle around which pus can track; as well as with the submental space inferiorly with mylohyoid muscle interposed; and the parapharyngeal space posteriorly.
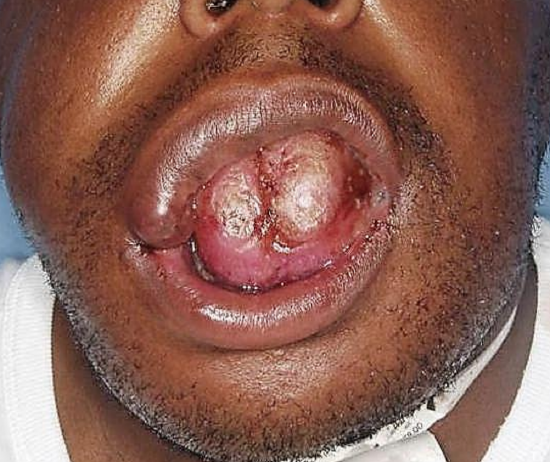
Figure 40: Swelling of the floor of the mouth with elevation of the tongue
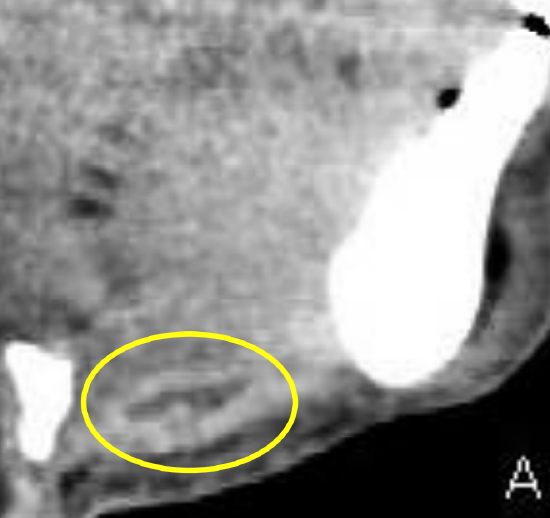
Figure 41: Sublingual space abscess situated above mylohyoid

Figure 42: Coronal CT scan of sublingual space abscess situated above mylohyoid
Sources of infection include dental sepsis, especially of the 3rd lower molar tooth, sialolithiasis, and an infected ranula. Patients present with pain, swelling, induration in the floor of the mouth and elevation of the tongue (Figure 40-42).
Surgical approaches to the sublingual space
Drain the sublingual space transorally by incising the mucosa in the anterior floor of the mouth, preferably parallel to the submandibular duct, and proceed with blunt dissection taking care not to injure the lingual nerve or the submandibular ducts. If the submandibular space is also affected, both spaces can be reached via a submandibular approach.
II.b. Submental Space
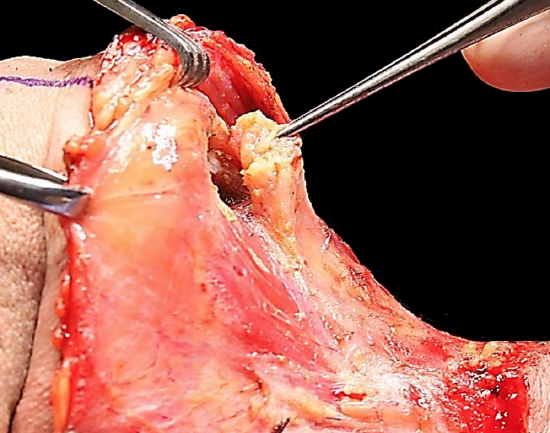
Figure 43: Elevating the contents of submental space from between the anterior bellies of digastric during a neck dissection
The submental space is located below the chin, crosses the midline and is bound superficially by the superficial layer of cervical fascia and skin, laterally by the anterior bellies of the digastric muscles, and deeply by the investing layer of cervical fascia overlying the mylohyoid muscle. The anatomical relations are the sublingual space (above mylohyoid) and the submandibular spaces laterally. It contains fat, lymph nodes and the anterior jugular vein (Figure 43).

Figure 44: Clinical presentation of infection of the submental space secondary to a carious mandibular incisor
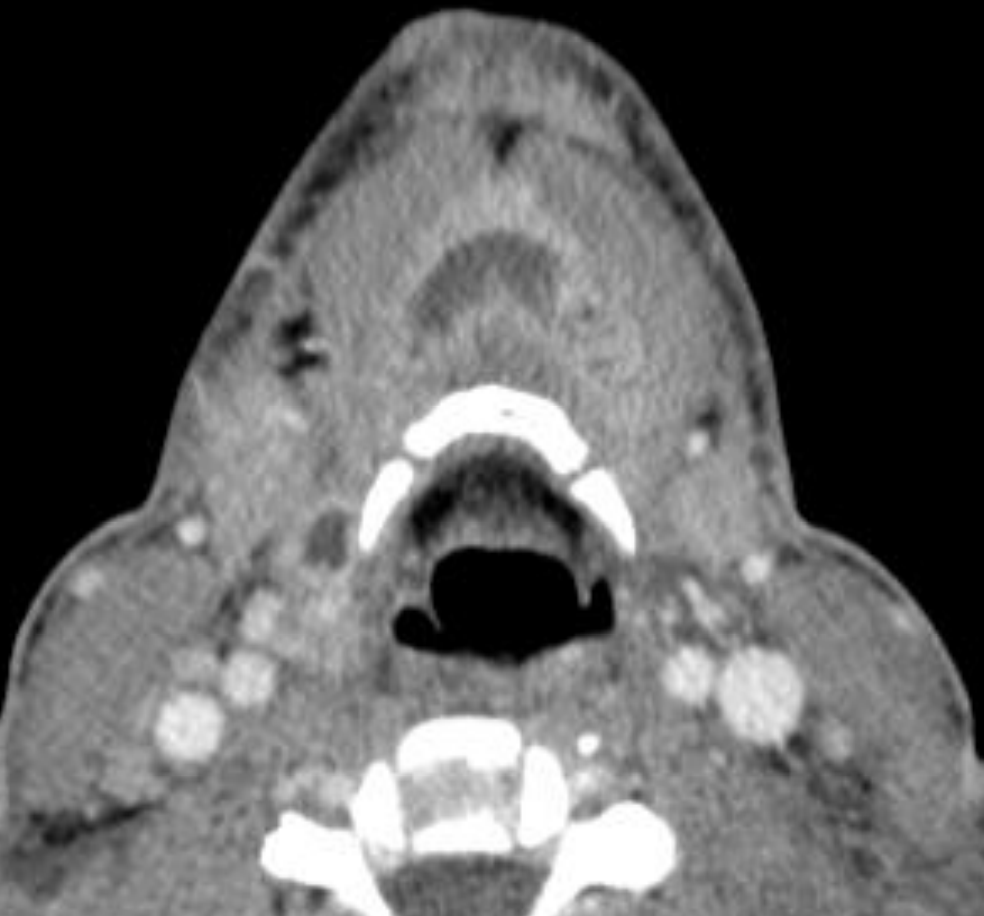
Figure 45: Submental space abscess anterior to the hyoid bone
Sources of sepsis are typically dental (mandibular incisor), an infected ranula, lymphadenitis or extension of infections of the submandibular space. Patients present with a tender submental swelling (Figures 44, 45).
Surgical approaches to the submental space
Drainage is achieved via an external transverse skin incision made between the hyoid bone and the mentum.
II.c. Submandibular Space
A lack of conformity exists in the literature about what is meant by “submandibular space”. Some subdivide the “submandibular space” into submaxillary, sublingual and submental spaces, while others consider the submaxillary and submandibular spaces to be synonymous. To best conform to conventional head and neck surgery terminology, the latter use of the word is adopted in this chapter.
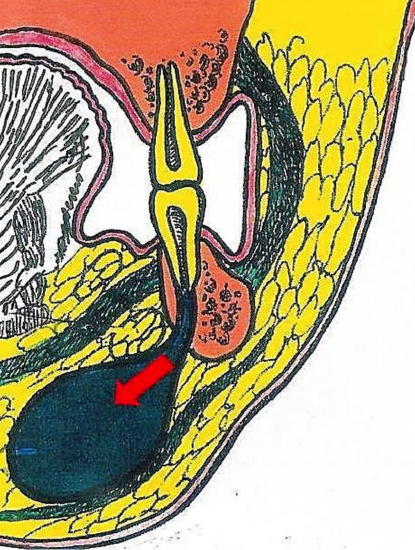
Figure 46: Coronal view depicting an odontogenic submandibular space abscess
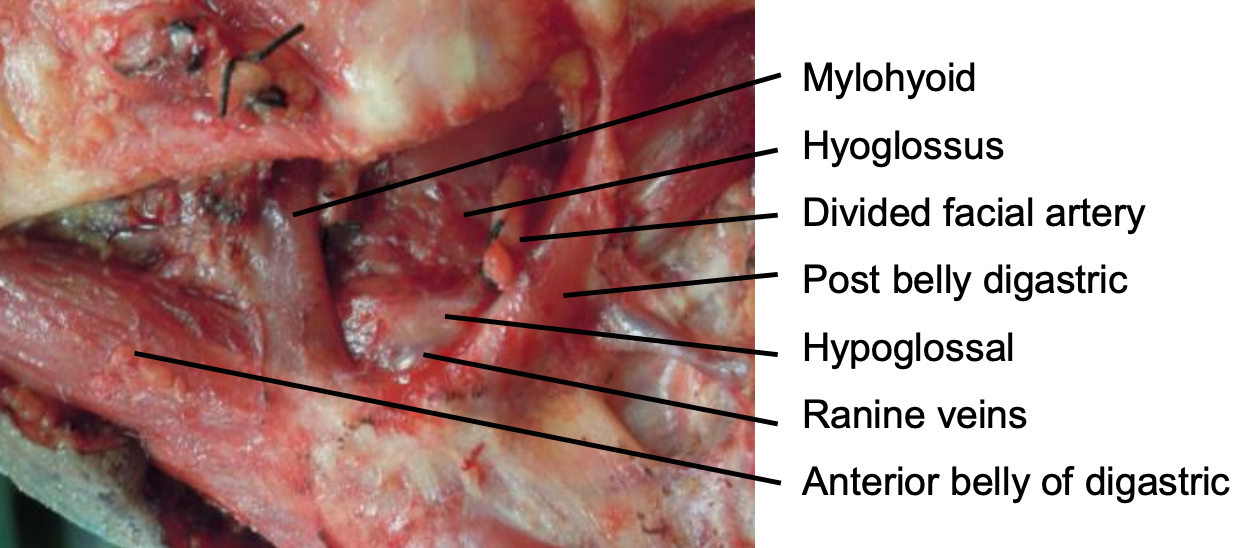
Figure 47: Medial wall of (L) submandibular space comprising thin investing fascia covering the mylohyoid muscle, hypoglossal nerve, ranine veins and hyoglossus muscle
As the most inferior space of the suprahyoid neck, the submandibular space extends upwards from the hyoid and is contained laterally between the hyoid and mandible by the superficial (investing) layer of deep cervical fascia and by the medial surface of the mandible up to its mylohyoid line (Figures 7, 8, 9, 46). Medially it is limited by the investing fascia that covers the mylohyoid muscle, the hypoglossal nerve, ranine veins and hyoglossus muscle (Figure 47). It contains the superficial portion of the submandibular gland, submandibular and submental lymph nodes, facial artery and vein, fat and the inferior loop of the hypoglossal nerve. The anterior belly of digastric separates it from the submental space (Figure 47). The submandibular gland and its duct pass around the posterior margin of the mylohyoid to enter the sublingual space in the floor of the mouth (Figures 38, 39). Behind the posterior margin of the mylohyoid muscle is a direct communication between the submandibular and sublingual spaces. Infection may spread anteriorly to the submental space and posteriorly to the parapharyngeal and/or retropharyngeal spaces.
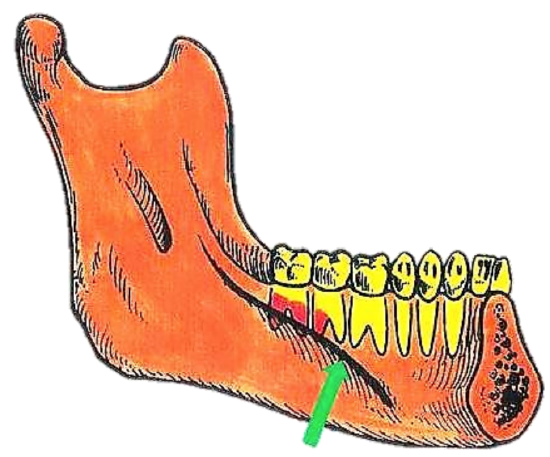
Figure 48: Odontogenic infections are commonly caused by the 2nd and 3rd mandibular molars as the apices of the dental roots extend below the mylohyoid line (green arrow)

Figure 49: OPG depicting a periradicular radiolucency of the 3rd molar

Figure 50: Submandibular space abscess
Sources of sepsis include sialadenitis, sialolithiasis, and dental sepsis (Figures 46, 48, 49). Patients typically present with swelling and tenderness over the submandibular triangle of the neck and only very minor trismus (Figures 50).
Surgical approaches to submandibular space

Figure 51: Horizontal skin crease incision made at level of hyoid extended through platysma muscle with blunt dissection

Figure 52: Corrugated extraoral drain in place
Make a horizontal skin crease incision at the level of the hyoid to avoid transecting the marginal mandibular nerve. Extend the incision through the platysma muscle using blunt dissection (Figures 51, 52).
II.d. Ludwig’s Angina

Figure 53: Typical appearance of Ludwig’s angina with sublingual, submental and submandibular swelling
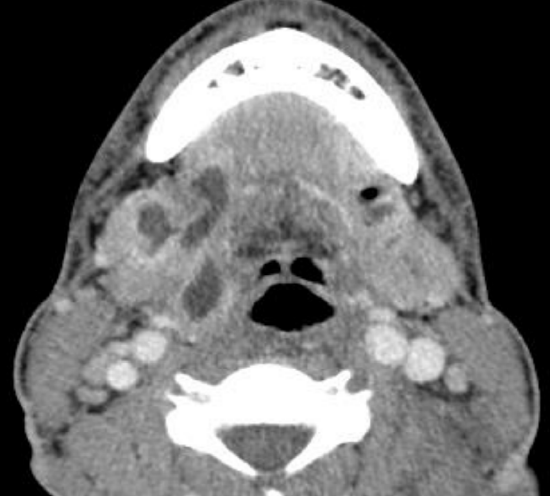
Figure 54: Bilateral submandibular space abscesses
Ludwig’s Angina, named after Wilhelm Friedrich Von Ludwig (1790-1865) refers to inflammation, cellulitis or an abscess, generally of dental origin, that involves the sublingual, submental and submandibular spaces. “Angina” is derived from the Latin term “angere”, which means “to strangle”. Patients present with pain, drooling, dysphagia, submandibular swelling, and trismus. Upward and posterior displacement of the tongue may cause severe airway compromise (Figure 53) which is the primary morbidity and mortality. In the pre-antibiotic era the mortality rate for was 50%; today the mortality rate is <5%. Sepsis is typically bilateral (Figure 54).
An orthopantomogram (OPG) or a CT scan should be requested to identify the source of dental sepsis; special attention should be paid to the status of the 2nd and 3rd lower molars. A contrast-enhanced CT scan or even MRI provides a roadmap for the surgeon to drain all septic foci in the neck (Figure 54).
Surgical approaches to Ludwig’s Angina

Figure 55: Fibreoptic flexible endoscope for nasotracheal intubation
Securing an airway is the initial objective. One should have a low threshold for doing an awake tracheostomy under local anesthesia to secure the airway before inducing anesthesia. Transoral intubation may be hazardous and is often unsuccessful. Fibreoptic intubation requires skill and experience and may cause nasal/nasopharyngeal bleeding (Figure 55).

Figure 56: Day 1 post-surgery depicting a severely compromised airway with marked elevation of the tongue
Nebulized adrenaline (1 mL 1:1000 adrenaline diluted to 5 mL with 0.9% saline) and intravenous dexamethasone (controversial) has been suggested to create more controlled conditions for flexible nasotracheal intubation. It is important to note that after incision and drainage, there is often even more swelling which may compromise the airway on day 1-2 after the surgery (Figure 56).
Early aggressive empiric intravenous antibiotic therapy targeting gram-positive and anaerobic organisms should be employed.
Incision and drainage: Ludwig’s angina starts as a rapidly spreading cellulitis without lymphatic involvement and generally without abscess formation. There is absolute consensus that drainage is indicated when there is a suppurative infection and/ or radiological evidence of a fluid collection or air in the soft tissues.
However one of the main controversies in management of Ludwig’s angina is whether surgical drainage is always indicated in the earlier stages of the infection. In the authors’ experience, a more aggressive surgical approach should be followed in all cases i.e. early tracheostomy and empiric placement of drains in the affected spaces after removal of the underlying cause. It must however be noted that this combined medical and surgical protocol is dictated by surgical/anesthesia/intensive care logistical problems often experienced in developing world practice.
Drainage may be intraoral and/or external, depending on the spaces involved. The submandibular spaces are drained externally. If sepsis extends both above and below the mylohyoid muscle, through-and-through drains extending between the oral cavity and the skin of the neck may be inserted.
II.e. Parapharyngeal Space (PPS)
The PPS extends from the base of the skull to the hyoid bone as an inverted pyramid in the center the head and neck, and consists mostly of fat. It is also known as the lateral pharyngeal space, pterygomaxillary space or pharyngomaxillary space.
Medially it is defined by the visceral layer of the deep cervical fascia (pharyngobasilar fascia above and buccopharyngeal fascia covering the superior pharyngeal constrictor muscle). The posterior border is formed by the prevertebral fascia of the deep layer and by the posterior aspect of the carotid sheath. Laterally the space is limited by the superficial/investing layer of deep cervical fascia that overlies mandible, medial pterygoids and parotid. The anterior boundary is the interpterygoid fascia and the pterygomandibular raphe.
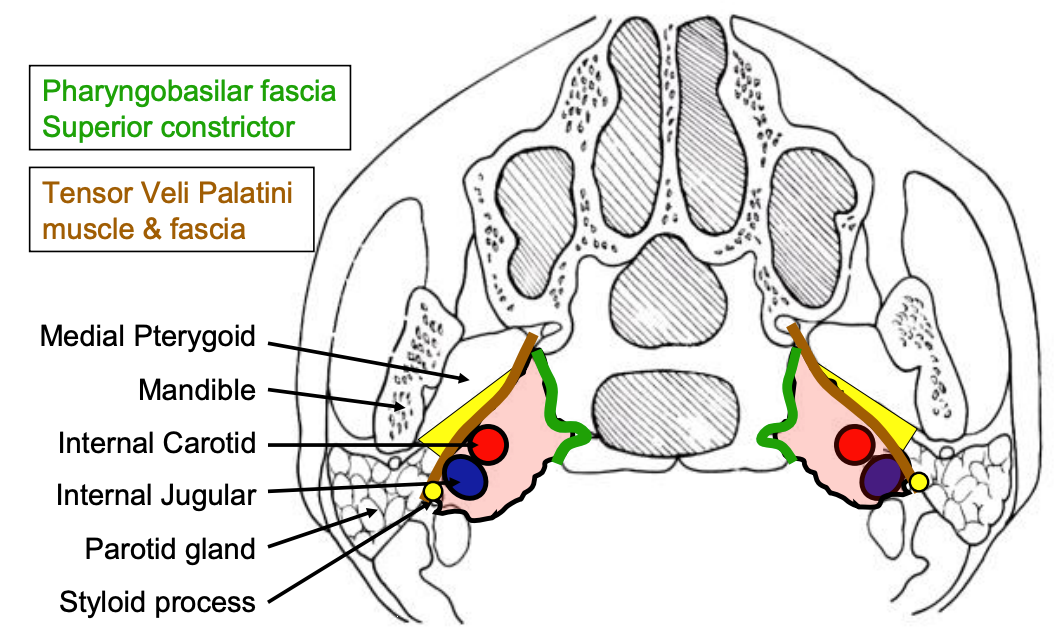
Figure 57: Schematic axial view of prestyloid (yellow) and poststyloid (pink) parapharyngeal spaces
The space is often divided into a prestyloid and a poststyloid compartment/space as the styloid process and styloid fascia divides this space. Some authors elect to use the terms prestyloid parapharyngeal space and parapharyngeal space synonymously as the poststyloid parapharyngeal space is regarded as a separate space namely the carotid sheath or space. Figure 57 illustrates the prestyloid and poststyloid components of the PPS, separated by the styloid process, tensor veli palatini and its fascia. The prestyloid PPS contains the internal maxillary artery, inferior alveolar nerve, lingual nerve, and auriculotemporal nerve, the deep lobe of the parotid gland, fat and occasionally ectopic salivary gland tissue. The poststyloid space encompasses the carotid space and contains the internal carotid artery, internal jugular vein, cranial nerves IX - XII, and the sympathetic trunk (Figure 57).
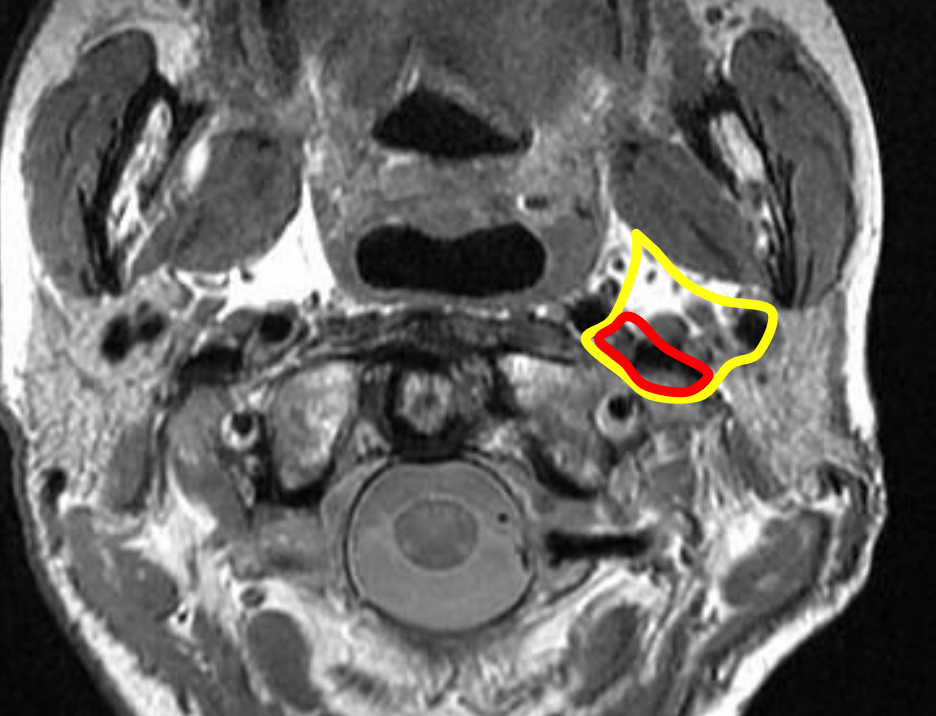
Figure 58: Parapharyngeal space (yellow outline) and carotid space/poststyloid space (red outline)
The PPS (Figure 58) is a central connection for all other deep neck spaces and was the most commonly affected space before the modern antibiotic era. It interfaces posterolaterally with the parotid space, posteromedially with the retropharyngeal space and inferiorly with the submandibular space. Anterolaterally it abuts the masticator space. The carotid space courses through the PPS. Infections can arise from tonsils, pharynx, teeth, salivary glands, nose, or may extend from a Bezold’s abscess (mastoid abscess).

Figure 59: Parapharyngeal space abscess (axial view)
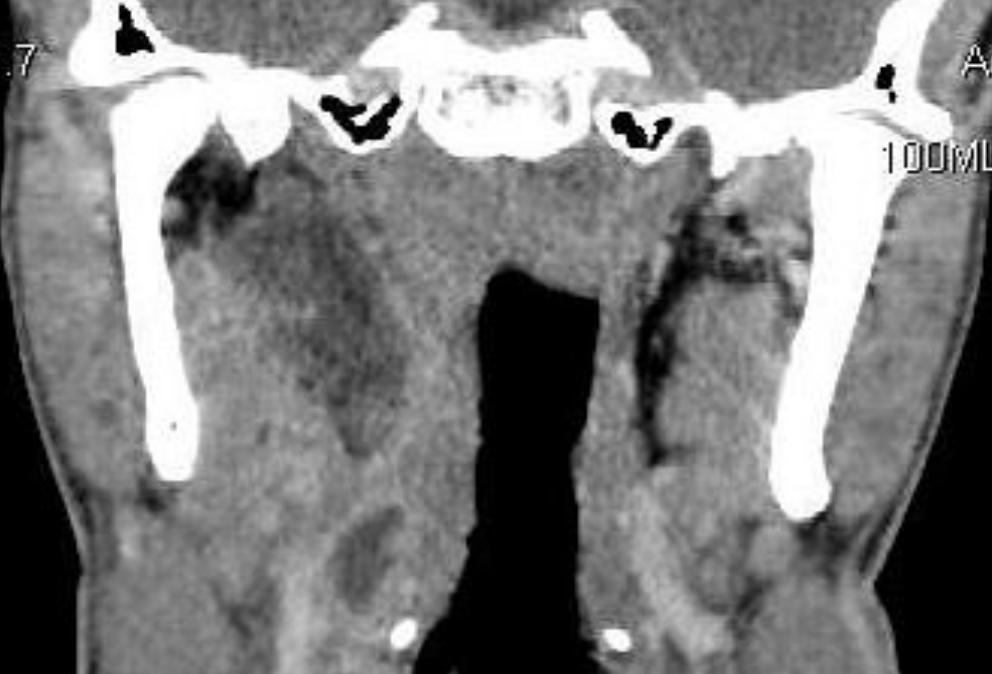
Figure 60: Parapharyngeal space abscess extending from hyoid to skull base
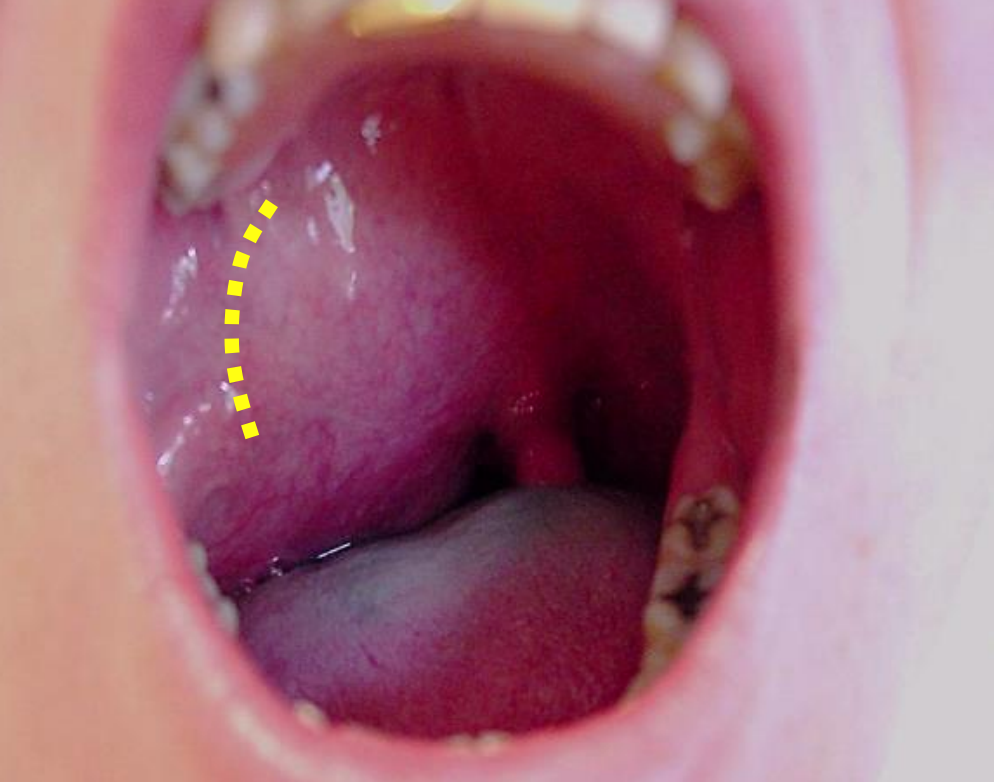
Figure 61: Typical clinical picture of a prestyloid PPS abscess and incision
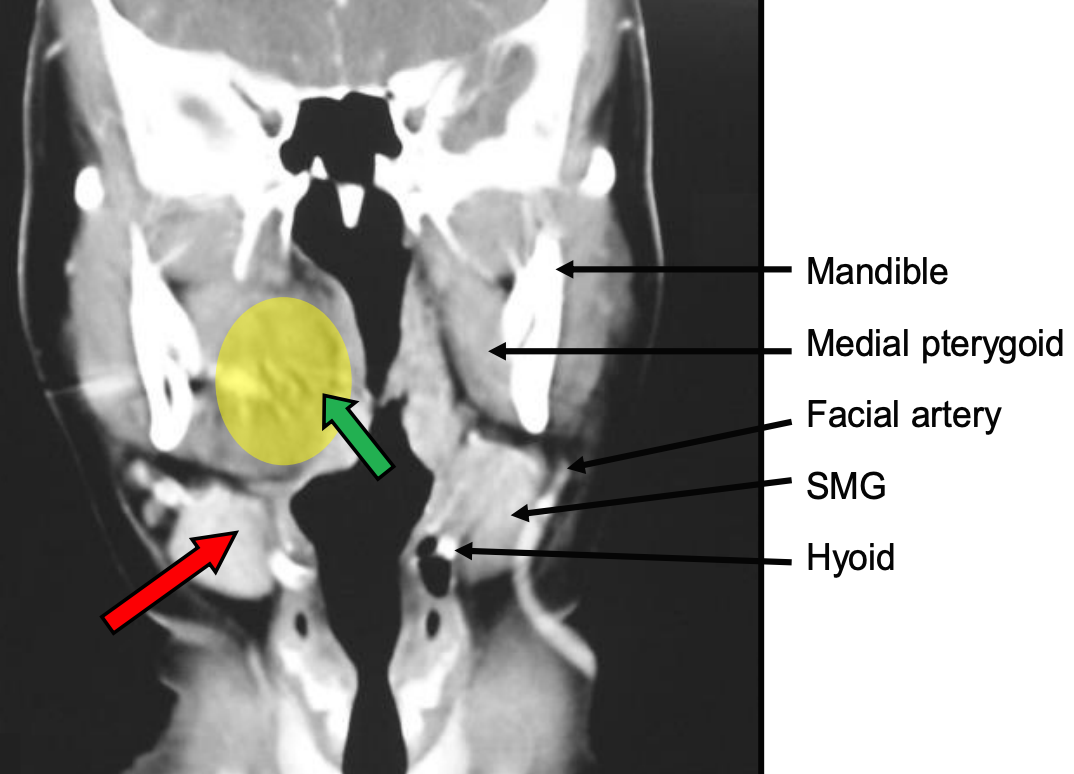
Figure 62: Anatomical relations of PPS abscess and drainage approaches either via oral cavity (green arrow) by incising the anterior tonsillar pillar lateral to the tonsil or via submandibular triangle above hyoid by dissecting bluntly with a finger posterior to the submandibular gland (red arrow)
Medial displacement of the lateral pharyngeal wall and tonsil is a hallmark of PPS infection (Figures 59-62). Trismus, drooling, dysphagia, odynophagia, neck stiffness, a “hot potato” voice and swelling below the angle of the mandible may be present when the anterior compartment is involved. The ipsilateral neck pain can be intensified by lateral flexion of the neck to the contralateral side which compresses the lateral pharyngeal space. Trismus suggests inflammation of the pterygoid muscle which lies close to the anterior compartment. Infection of the posterior compartment often has no trismus or visible swelling.
Surgical approaches to the PPS
Three approaches may be employed depending on the location of the abscess. Additional approaches may be considered to drain adjacent sepsis.
The prestyloid PPS may be drained transorally (Figure 61) by incising the lateral pharyngeal wall, or via a suprahyoid approach (Figure 62).
The retrostyloid PPS is best approached transcervically from Level 2a of the neck. A transverse cervical skin incision is made, and subplatysmal flaps elevated to expose the anterior border of sternomastoid. The investing layer of deep cervical fascia is divided along the anterior border of the sternocleidomastoid, and a finger is passed deep to the posterior belly of digastric, dissecting bluntly along the carotid sheath up to the tip of the styloid.
II.f. Peritonsillar Space
The peritonsillar space is bound medially by the capsule of the palatine tonsil, laterally by the superior constrictor, while the anterior and posterior borders are defined by the anterior and posterior tonsillar pillars. It is a potential space and has no important contents, mostly loose connective tissue. Laterally it abuts the masticator space; this accounts for the typical occurrence of trismus with inflammatory processes. Posteriorly it borders the parapharyngeal space.
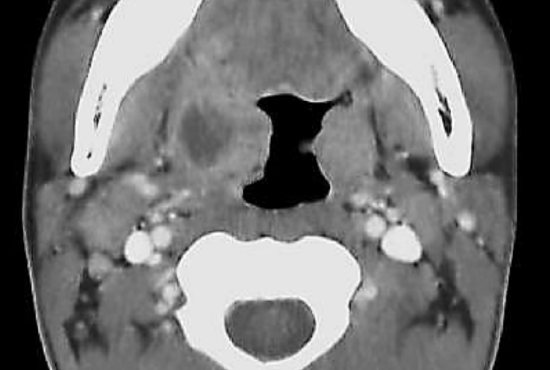
Figure 63: Peritonsillar abscess displacing tonsil medially
Peritonsillar abscesses (Figure 63) are the most common deep neck space abscesses and occur as a consequence of tonsil infection. It has also been proposed that it is a consequence of inflammation of Weber’s glands which are minor salivary glands found in the peritonsillar space.
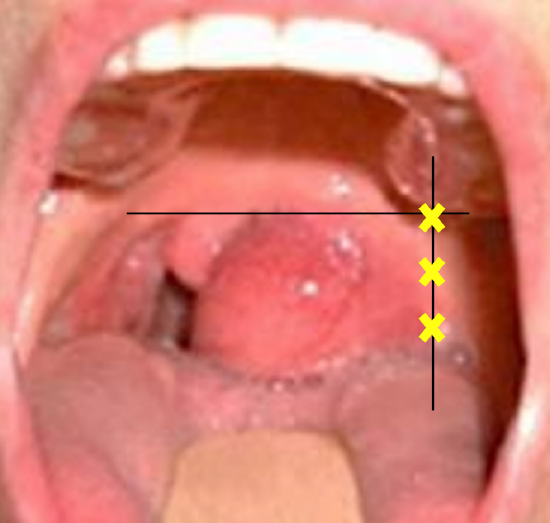
Figure 64: Avoid entering the tonsil by commencing aspiration where horizontal line at the base of uvula intersects with a vertical line through molar teeth; if unsuccessful, then aspirate along the vertical line
Patients typically present with pain, odynophagia, drooling, dehydration, trismus, medial displacement of the tonsil, palatal asymmetry, edema and contralateral displacement of the uvula (Figure 64). The diagnosis is clinical and special radiological investigations are usually unnecessary.
Surgical approaches to peritonsillar space
Peritonsillar abscesses may be treated by needle aspiration, incision and drainage, or quinsy tonsillectomy.
Needle aspiration/Incision and drainage: Local anesthetic is injected along the anterior tonsillar pillar followed by transoral needle aspiration and/or incision and drainage with a scalpel superomedially. The incision is then opened widely with a hemostat. The classical needle aspiration sites are demonstrated in Figure 64. A needle inserted too medially will enter the tonsil tissue and miss the abscess cavity.
Quinsy tonsillectomy: This is advocated by some surgeons for patients with recurrent tonsillitis or in children who would not tolerate a procedure under local anesthesia. The patient, however, should first be rehydrated and optimized for surgery. As trismus is generally due to muscle spasm, it resolves on induction of anesthesia. Hence intubation is generally not a problem. The tonsillectomy on the side of the quinsy is usually quite straight-forward once the abscess cavity has been entered as the abscess wall defines the lateral dissection plane. Bipolar cautery is required for hemostasis as ligating vessels in inflamed tissues may prove difficult.
III.a. Pretracheal Space

Figure 65ab: Pretracheal abscesses
The pretracheal (anterior visceral or previsceral space) is enclosed by the visceral layer of the middle layer of deep cervical fascia. It lies immediately anterior to the trachea, abuts the ventral wall of the esophagus posteriorly and extends from the superior border of the thyroid cartilage to the superior mediastinum at level T4 (Figures 65 a, b). Etiology includes perforation of the anterior esophageal wall by endoscopic instrumentation, foreign bodies, trauma and thyroiditis. Patients present with dysphagia, odynophagia, pain, fever, voice change and stridor.
Surgical approaches to pretracheal space
Drainage is achieved by a transverse anterior skin crease cervical incision.
IV.a. Retropharyngeal Space
The retropharyngeal space is located immediately behind the nasopharynx, oropharynx, hypopharynx, larynx, and trachea. It is bound anteriorly by the visceral layer of the middle layer of the deep cervical fascia where it surrounds the pharyngeal constrictors, and posteriorly by the alar layer of the deep layer of deep cervical fascia. It extends from the skull base to T2/tracheal bifurcation where the visceral and alar layers fuse (Figures 2, 3, 4). It contains retropharyngeal lymphatics and lymph nodes, and communicates laterally with the parapharyngeal spaces where it abuts the carotid sheaths.
Because retropharyngeal lymph nodes generally regress by age 5 years, retropharyngeal space infection occurs more commonly in young children. Most retropharyngeal abscesses in children are related to upper respiratory tract infections. In adults they are generally caused by direct trauma and foreign bodies, and may also be caused by traumatic perforations of the posterior pharyngeal wall or esophagus. Sepsis may also extend from the parapharyngeal space, or from infections originating in the nose, adenoids, nasopharynx, and sinuses. The differential diagnosis includes an abscess secondary to spinal tuberculosis.

Figure 66: Lateral X-ray demonstrating flattening of the spine and soft tissue swelling of >½ of the vertebral bodies (arrow) (Wikipedia)
Patients present with malaise, neck stiffness, odynophagia, bulging of the posterior pharyngeal wall, trismus, stertor or stridor. Sepsis may extend posteriorly to the prevertebral space, into the chest causing mediastinitis and empyema, or laterally to the parapharyngeal space. It can cause carotid artery rupture and jugular vein thrombosis. CT is the imaging investigation of choice. Lateral cervical X-rays show loss of cervical lordosis and widening of the prevertebral soft tissues which should normally be less than ½ the width of the corresponding vertebral body (Figure 66). CXR or CT is done to exclude intrathoracic extension of sepsis.
Surgical approaches to retropharyngeal space
Sedation and muscle relaxants should be avoided to prevent loss of control of the airway.
Small abscesses may be aspirated transorally with a needle in a compliant patient. Larger abscesses require incision and drainage using transoral and/or transcervical approaches.
With transoral drainage it may be helpful to localize the abscess by first aspirating it before incision and drainage. Make an incision through the posterior pharyngeal wall mucosa, and open the abscess with blunt dissection.
Transcervical drainage is achieved by a transverse cervical skin incision, raising subplatysmal flaps to expose the neck and dissecting along the anterior border of the sternomastoid. The sternocleidomastoid muscle and carotid sheath are then retracted laterally and blunt dissection is done up to the hypopharynx to open the retropharyngeal space abscess.
IV.b. Danger Space
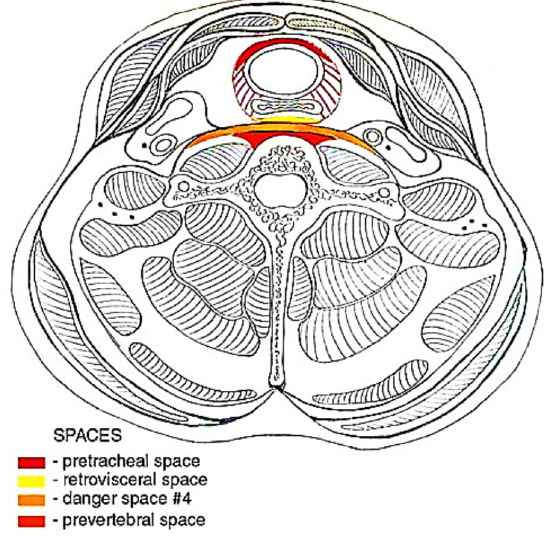
Figure 67: Danger space (orange); prevertebral space (red), retropharyngeal space (yellow), and pretracheal space
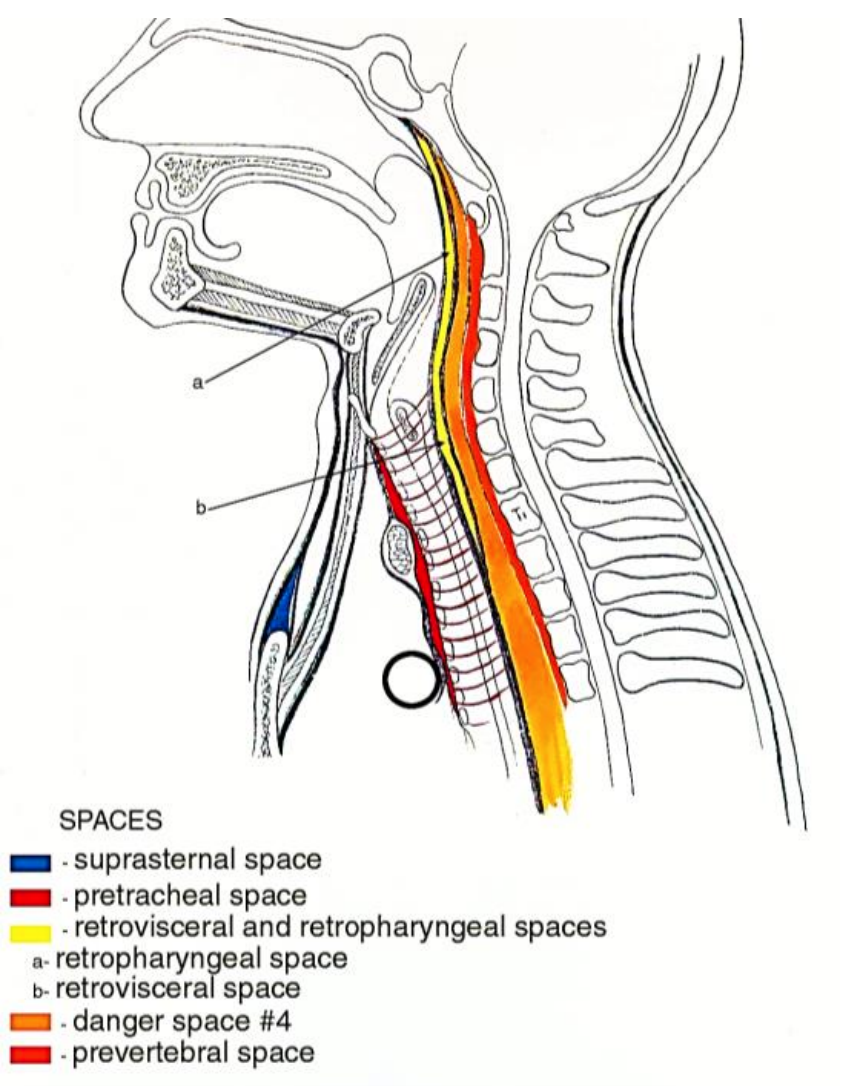
Figure 68: Danger space (orange); prevertebral space (red), retropharyngeal space (yellow), and pretracheal space
The term “danger space” is derived from the potential for rapid spread of infection along this space to the posterior mediastinum. It is a potential space that contains mostly fat. It is located between the alar and prevertebral layers of the deep layer of deep cervical fascia and laterally is bordered by the transverse processes (Figure 67, 68). It is immediately posterior to the retropharyngeal space, anterior to the prevertebral space, and extends from the skull base above to the posterior mediastinum and diaphragm below.

Figure 69: CT depicting soft tissue air in a patient with mediastinitis caused by spread from a fascial space infection
Infection usually originates from adjacent retropharyngeal, parapharyngeal, or prevertebral sepsis and may spread rapidly because of the loose areolar tissue that occupies this space to cause mediastinitis (Figure 69), empyema, and septicaemia.
Clinically the infection is difficult to distinguish from infection of the retropharyngeal space. Even contrast-enhanced CT may not adequately differentiate between infection of the retropharyngeal and danger spaces, but extension below T4 suggests involvement of the danger space. The differential diagnosis includes tuberculosis.
Surgical approaches to the Danger Space
Surgical drainage is achieved by an external transcervical approach along the anterior border of the sternocleidomastoid, dissecting between the larynx and the carotid sheath. One may need to divide the superior thyroid artery for access.
IV.c. Carotid Space
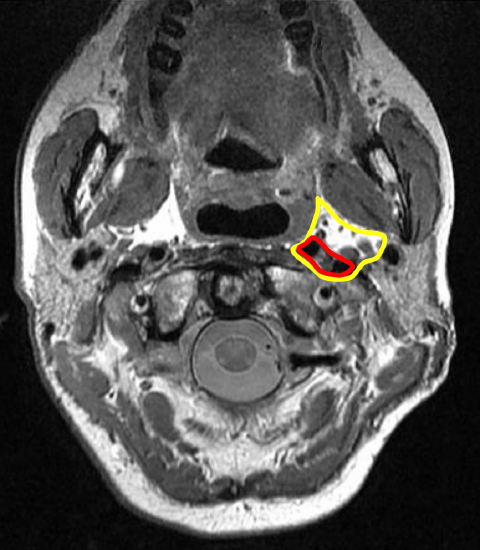
Figure 70: Parapharyngeal space (yellow outline) and carotid/poststyloid space (red outline)
The carotid space is a potential space contained within the carotid sheath (Figure 70). The nomenclature is confusing and terms such as carotid sheath and post-styloid parapharyngeal space (PPS) are used synonymously. The carotid sheath is formed by the muscular layer of the middle layer of deep cervical fascia. The investing layer of deep cervical fascia contributes to the anterior wall (Figures 3, 4).
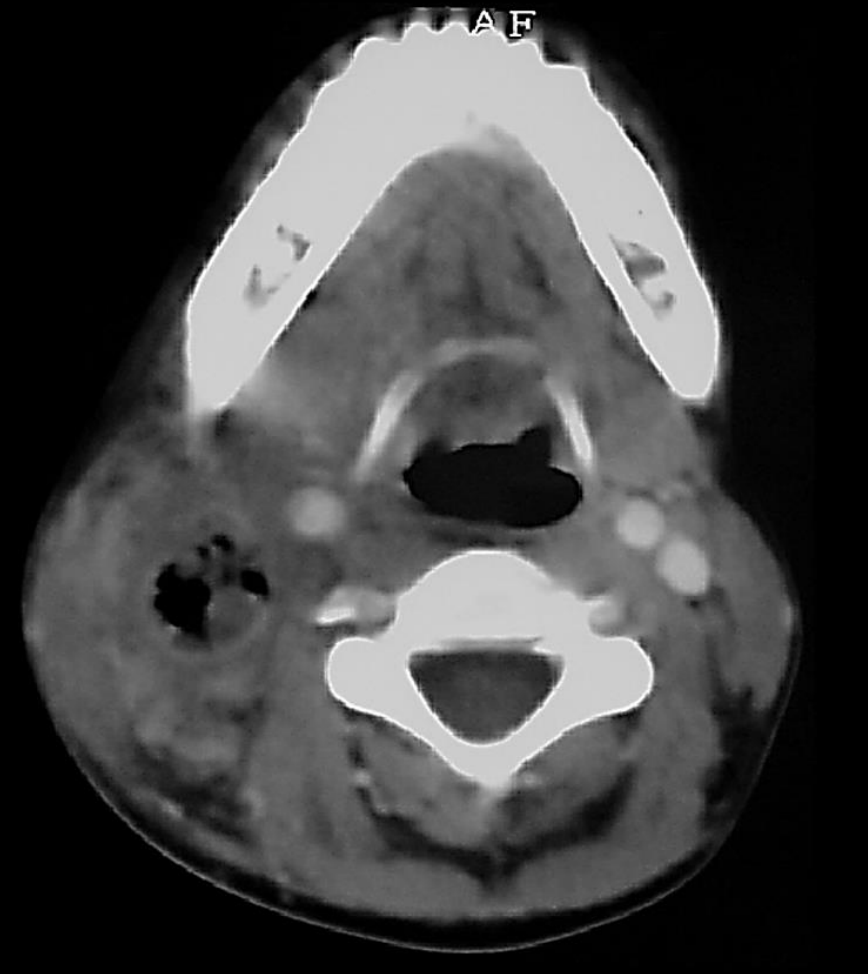
Figure 71: Carotid space abscess within lumen of internal jugular vein as a consequence of mastoiditis
The space contains the internal carotid artery, internal jugular vein, cranial nerves IX-XII, lymph nodes and the sympathetic trunk. Above the level of the hyoid bone it is contained within the retrostyloid component of the PPS (Figure 71). In the suprahyoid neck the space is bordered anteriorly by the styloid process and the PPS, laterally by the anterior belly of digastric and the parotid space and medially by the lateral margin of the retropharyngeal space.
Sepsis may originate from infection within the PPS, from intravenous drug abuse, central venous (CVP) line sepsis, or from lateral sinus thrombosis related to mastoiditis (Figure 71). Patients may initially not have localising signs as the infection is deep-seated. Often clinical signs may only become evident after onset of neurological or vascular complications. Patients may present with torticollis to the side opposite to the sepsis, and tenderness along the course of the carotid. They lack trismus. Vascular complications include suppurative jugular vein thrombophlebitis (Lemierre syndrome), septic pulmonary emboli, carotid artery thrombosis, carotid aneurysm, stroke, or carotid or jugular vein blowouts. Involvement of the sympathetic trunk can cause Horner’s syndrome. Contrast enhanced CT is recommended. Duplex ultrasonography can identify vascular complications.
Surgical approaches to the carotid space
Treatment is directed at drainage of the sepsis via a transverse cervical skin crease incision with elevation of subplatysmal flaps superiorly and inferiorly for exposure. Clot propagation and pulmonary emboli are limited by anticoagulation.
IV.d. Prevertebral Space
This is a potential space and extends from the skull base to the coccyx. Due to the anatomy of the potential space, it has also been named the perivertebral space. It is divided into two divisions, namely the prevertebral and paraspinal spaces. It is immediately posterior to the Danger Space and is bound anterolaterally by the carotid space. It is located anterior to the vertebral bodies, behind the prevertebral fascial layer of the deep layer of deep cervical fascia that separates it from the Danger Space (Figures 67, 68). Laterally it is limited by the fusion of the prevertebral fascia with the transverse processes of the vertebral bodies.
Infection may be caused by trauma, especially surgery, or may originate from the cervical or thoracic spine. The diagnosis is difficult to make. Patients may present with neck and/or back pain, just fever and/or neurologic dysfunction ranging from nerve root pain to paralysis. MRI is the imaging modality of choice to assess epidural or spinal cord involvement.
Surgical approaches to prevertebral space
Incision and drainage may be done using transoral or transcervical approaches. The latter approach is made along the anterior border of sternocleidomastoid, dissecting between the larynx and the carotid sheath. One may have to divide the superior thyroid artery for access.
Antibiotics for odontogenic infections
Antibiotics should initially be administered empirically, parenterally, at high doses, and should cover a broad spectrum of oral flora i.e. gram-positive, gram-negative, and anaerobic organisms. The literature advises empiric treatment with combinations of penicillin, clindamycin, and metronidazole. The authors favor a combination of penicillin G and metronidazole. Alternatively, amoxicillin-clavulanate with metronidazole can be used, or clindamycin for patients who are allergic to penicillin. Antibiotic cover needs to be extended to cover Methicillin-resistant Staphylococcus aureus (MRSA) and gram-negative rods in immune compromised patients. Antibiotics should be modified based on the results of microscopy, culture and sensitivity reports.
Recommended reading
Author
Jean Morkel BChD, MBChB, MChD, FCMFOS
Professor and Academic Head
Department of Maxillo-Facial and Oral
Surgery and Anesthesiology & Sedation
Faculty of Dentistry
University of the Western Cape
Cape Town, South Africa
jamorkel@uwc.ac.za
Author & Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


