1.45: Cricopharyngeal Myotomy Surgical Technique
- Page ID
- 53485
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
CRICOPHARYNGEAL MYOTOMY: SURGICAL TECHNIQUE
John Fagan
Cricopharyngeal myotomy may be indicated for cricopharyngeal spasm causing dysphagia or aspiration and is done in patients undergoing external resection of a pharyngeal pouch / Zenker’s diverticulum (ZD).
Cricopharyngeal dysfunction / achalasia may be primary or secondary. Primary achalasia refers to persistent spasm or failure of the cricopharyngeus to relax, where the pathology is confined to the muscle and there is no underlying neurologic or systemic cause. It may be idiopathic or be associated with intrinsic disorders of the muscle e.g. polymyositis, muscular dystrophy, and hypothyroidism. Cricopharyngeal spasm may be secondary to neurologic disorders e.g. poliomyelitis, oculopharyngeal dysphagia, stroke, and amyotrophic lateral sclerosis (ALS), or diabetic neuropathy, myasthenia gravis, and peripheral neuropathies.

Figure 1: Note cricopharyngeal bar

Figure 2: Spasm of cricopharyngeus muscle causing dysphagia
The diagnosis is made on history and contrast swallow (videofluoroscopy). The contrast swallow typically shows a prominent bulge in the posterior wall of the proximal esophagus due to contraction of the cricopharyngeus muscle (Figure 1). Figure 2 shows spasm of the cricopharyngeus muscle causing dysphagia and regurgitation.
The myotomy is commonly done via an external approach, although an endoscopic approach using CO2 laser can also be employed. Alternative treatments include dilatations and Botulinum toxin injections.
Cricopharyngeal myotomy is also done in patients undergoing external resection of a pharyngeal pouch, as elevated cricopharyngeus muscle tone is considered a cause of a ZD.

Figure 3: Contrast swallow before and after endoscopic diverticolotomy: Cricopharyngeus (yellow arrows) and the party wall between the ZD and the esophagus are divided

Figure 4: Cricopharyngeal bar (CP) containing the cricopharyngeus muscle, which separates esophagus (O) from ZD
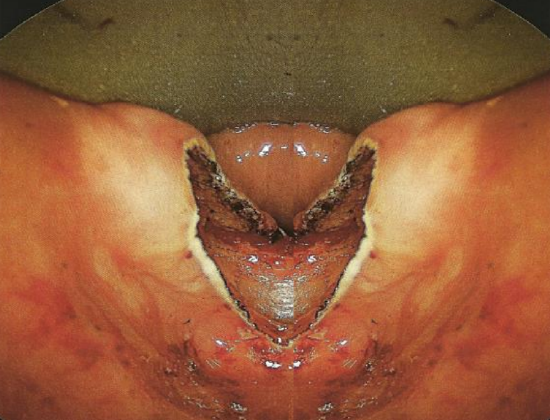
Figure 5: Party wall has been divided. Note that both the cricopharyngeus muscle and mucosa have been divided to the inferior aspect of the sac

Figure 6: ZD would be very difficult to treat with a stapler and is best done with CO2 laser cricopharyngeal myotomy, as it is too shallow for the stapling technique
With endoscopic diverticulotomy, the cricopharyngeus muscle is divided when cutting through the wall between the ZD and the esophagus (Figure 3-5). See chapter on Zenker’s Diverticulum. Cricopharyngeal myotomy may also be done in isolation for very small ZDs (Figure 6).
Surgical anatomy

Figure 7: Red arrow shows where ZD extrudes through Killian’s dehiscence (blue) between the inferior constrictor and the cricopharyngeus muscles
Figure 7 illustrates how the cricopharyngeus muscle fans out from its origin from the cricoid cartilage to surround the proximal end of the esophagus. Note Killian’s dehiscence through which a ZD typically herniates between the cricopharyngeus and inferior constrictor muscles. Note also the proximity of the recurrent laryngeal nerve, which should be protected from injury with external surgical approaches.

Figure 8: Barium swallow of ZD. Note how the buccopharyngeal fascia contains the pharynx, esophagus and diverticulum (green line)
Figure 8 illustrates the buccopharyngeal fascial layer that contains the pharynx and esophagus, and a ZD.
The anatomic relationship between the ZD and the surrounding buccopharyngeal fascial layer is key to understanding how the upper digestive tract remains separated from the retropharyngeal space when incising the anterior wall of the diverticulum, or with isolated endoscopic cricopharyngeal myotomy. Disrupting this fascial layer can theoretically increase the likelihood of developing mediastinitis. When endoscopically dividing a hypertrophic cricopharyngeus muscle in the absence of a ZD, the buccopharyngeal fascia is situated immediately behind the cricopharyngeus muscle; hence great care must be taken to preserve this fascial layer when endoscopically dividing the cricopharyngeus muscle. Despite initial fears that this fascia could not be preserved during endoscopic cricopharyngeal myotomy, Chang et al demonstrated in a cadaveric study that the buccopharyngeal fascial layer remained histologically intact with CO2 laser cricopharyngeal myotomy. 1
Special investigations
Diagnosis of cricopharyngeal spasm and a ZD is confirmed with a contrast swallow or videofluoroscopy (Figures 1-2). Laryngoscopy is done to rule out other causes of dysphagia. Preoperative evaluation must include assessment of the function of the lower esophageal sphincter, as cricopharyngeal myotomy in patients with an incompetent lower sphincter places them at risk of developing severe gastroesophageal and laryngopharyngeal reflux.
External cricopharyngeal myotomy
External cricopharyngeal myotomy is a quick and relatively simple procedure.
- Perform direct laryngoscopy and rigid esophagoscopy to exclude other pathology causing dysphagia such as tumors and strictures

Figure 9: Suction tubing used to stent esophagus
- Stent the esophagus with a piece of suction tubing (Figure 9) / endotracheal tube / Maloney dilator; this helps the surgeon to palpate and identify the esophagus during dissection
- Extend the neck and turn the head to the right side
- Palpate and identify the cricoid cartilage; this denotes the level of cricopharyngeus

Figure 10: Transverse skin incision

Figure 11: Liberal exposure achieved with transverse incision and subplatysmal flaps; AJV: Anterior jugular vein; SCM: Sternocleidomastoid
- Make a liberal transverse cervical skin incision to the left of the midline at the level of the cricoid (Figure 10). A transverse incision is cosmetically preferable to a vertical incision
- Incise platysma muscle
- Elevate subplatysmal flaps (Figure 11)
- Dissect along the anterior border of the sternocleidomastoid muscle
- Identify and divide the omohyoid muscle as it crosses the internal jugular vein
- Dissect along the medial aspect of the internal jugular vein and common carotid artery, and the lateral aspect of the thyroid gland, larynx and trachea
- Identify, ligate and divide the middle thyroid vein

Figure 12: Retracting the sternocleidomastoid (SCM) exposes the thyroid gland (TG), larynx (L), internal jugular vein (IJV) and common carotid artery (CA)
- Continue the dissection until the prevertebral fascia is reached, and strip superiorly and inferiorly with a finger to expose the larynx, esophagus, thyroid gland (medially) and contents of the carotid sheath (laterally) (Figure 12)
- The superior laryngeal nerve defines the superior boundary of the dissection
- Palpate the cricothyroid joint

Figure 13: The rake is retracting the thyroid gland to expose the 1st tracheal ring (TR), esophagus (O), cricopharyngeus (CP), and inferior constrictor (IC)
- Place a double pronged hook or sharp rake under the posterior edge of the thyroid cartilage or the thyroid gland and rotate the laryngotracheal complex to bring the esophagus, cricopharyngeus and inferior pharyngeal constrictor muscles into view (Figure 13)
- With this laryngotracheal rotation the RLN is safe, provided one dissects close to the posterior midline of the cricopharyngeus muscle
- Palpate and identify the cricoid cartilage
- Palpate and identify the firm tubing / dilator within the esophagus
- The cricopharyngeus muscle is easily palpated and visualized, stretched over the esophageal stent

Figure 14: Cricopharyngeal myotomy, with esophageal mucosa stretched over suction tubing coming into view

Figure 15: Completion of cricopharyngeal myotomy with muscle elevated from mucosa

Figure 16: Closed wound and suction drain
- Cut vertically with a 15# scalpel blade through the cricopharyngeus muscle until the underlying esophageal mucosa comes into view (Figures 14, 15)
- Ensure hemostasis
- Insert a suction drain, and close the neck in a layered fashion (Figure 16)
- Introduce oral fluids the same day if the mucosa has not been breached
Endoscopic cricopharyngeal myotomy
- Administer broad spectrum antibiotics perioperatively
- General anesthesia is done with orotracheal intubation (nasotracheal intubation hampers access)
- Protect the upper teeth with a gum guard
- Perform laryngoscopy
- Perform rigid esophagoscopy
- Inspect the esophagus to rule out other pathology that may be causing symptoms such as tumors or strictures
- Dilating the esophageal opening with the scope facilitates subsequent passage of the diverticuloscope

Figure 17: Weerda bivalve diverticuloscope

Figure 18: Benjamin diverticuloscope
- Insert a Weerda or Benjamin diverticuloscope (Figures 17, 10)
- Extend the neck posteriorly as far as the cervical spine allows
- Lubricate the scope
- Advance the scope with blades slightly apart until the esophageal opening appears
- It is not always possible to insert the scope due to anatomical limitations
- Pass the anterior blade of the scope into the esophagus and keep the posterior blade against the posterior wall of the hypopharynx
- Identify the transverse bar denoting the upper edge of cricopharyngeus
- Distract the blades further to better visualize the cricopharyngeus bar
- Suspend the scope with a scope holder
- Visualize the cricopharyngeus bar using an operating microscope with an integrated CO2 laser microsled
- Set the CO2 laser at 5-10W, CW mode and with a slightly defocused spot size to improve hemostasis

Figure 19: Transmucosal laser cricopharyngeal myotomy: incising mucosa and muscle

Figure 20: Transmucosal laser cricopharyngeal myotomy: completed myotomy
- Use CO2 laser to transect the mucosa overlying the muscle in the midline (Figure 19)
- Meticulously completely transect the cricopharyngeus muscle without disrupting the posterior layer of perioesophageal fascia (Figure 20)
- Instruct the anesthetist to avoid ventilating the patient with a face mask when reversing the anesthesia, as it may cause air to track through the defect into the tissues of the neck, causing surgical emphysema and potentially increasing the risk of a postoperative leak and sepsis
- Observe the patient overnight
- Following CO2 laser, a small number of patients develop some subcutaneous emphysema; this almost never results in mediastinitis
- Monitor for signs and symptoms that signal mediastinitis e.g. radiating back or chest pain, fever, and tachycardia despite adequate pain control, as early intervention for this rare but potentially fatal complication is mandatory
- Commence a clear liquid diet the morning following surgery
- Discharge the patient if he/she tolerates a clear liquid diet without concerning signs or symptoms
- The patient should remain on liquids and soft foods for at least a week
Reference
- Chang CWD, Liou SS, Netterville JL. Anatomic Study of Laser-Assisted Endoscopic Cricopharyngeus Myotomy. Ann Otol Rhinol Laryngol 2005; 114(12):897-901
Suggested chapters in Open Access Atlas
- CO2 laser transoral microsurgery
- Surgery for pharyngeal pouch / Zenker’s diverticulum
Author & Editor
Johan Fagan MBChB, FCS (ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


