2.18: Lateral Temporal Bone Resection
- Page ID
- 17722
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
LATERAL TEMPORAL BONE RESECTION SURGICAL TECHNIQUE
Rajeev Mathew, Tashneem Harris, Parag Patel
Lateral temporal bone resection refers to en bloc resection of the external auditory canal (EAC) with the tympanic membrane (TM). It is generally performed for malignancies involving the EAC, the most common being primary squamous cell carcinoma. Tumors may arise from the skin of the external ear, parotid, glandular adnexa of the ear or may be metastases to parotid nodes.
History and examination
History and examination are directed at making a diagnosis and determining the extent of the tumor. Refractory pain is a hallmark of advanced malignancy of the ear canal. Other presenting symptoms include chronic ear discharge and hearing loss. A lesion of the ear canal may be visible and there may be a discharge. The parotid and neck should be examined for evidence of metastases. Facial nerve function should be documented. Assessing sensation of the face on the affected side as well as the lower cranial nerves is crucial to detect intracranial and inferomedial extension to the jugular foramen. Differential diagnoses include skull base osteomyelitis and inflammatory conditions e.g. TB.
Special investigations
The tumor is biopsied in the office to confirm the diagnosis. Imaging is requested to:
- Determine local extent of the tumor
- Stage the tumor (see below)
- Determine its operability
- Rule out regional nodal metastases to parotid and cervical nodes
- Plan the surgical approach
High resolution CT scans (0.5 mm slices with and without contrast) of the temporal bone, brain, parotid and neck allow assessment of the soft tissue extent, bony destruction, as well as clinical staging. MRI is useful to assess soft tissue involvement particularly if disease appears to have breached the EAC/TM and there is concern about involvement of dura or brain. Pure tone audiometry should be performed. Carotid angiography +/- balloon occlusion is considered if surgery is contemplated and there is concern about carotid artery involvement.
Modified Pittsburgh Staging System
T1: Limited to EAC without bony or soft tissue extension into mastoid/middle ear
T2: Limited EAC erosion (not full thickness) or radiological findings consistent with <0.5cm soft tissue involvement
T3: Full thickness erosion of EAC with <0.5cm soft tissue involvement or facial nerve paralysis
T4: Eroding cochlea, petrous apex, carotid canal, jugular foramen, medial wall of middle ear, dura or with >0.5cm soft tissue extension
Practical application of staging system
T1: Sleeve resection or lateral temporal bone resection
T2: Lateral temporal bone resection
T3: May be suited to lateral temporal bone resection with sacrifice of facial nerve
T4: Not amenable to lateral temporal bone resection
Surgical Anatomy
The lateral 1/3 of the EAC is composed of fibroelastic cartilage and contains the Fissures of Santorini - these communicate with the parotid anteriorly and the soft tissue overlying the mastoid posteriorly. The medial 2/3 of the EAC consists mainly of the tympanic portion of the temporal bone.
Important relations of the EAC include the tegmen tympani superiorly, mastoid bone posteriorly, styloid process inferiorly, and temporomandibular joint (TMJ) anteriorly (Figures 1 and 2). The foramen of Huschke is a developmental defect in the EAC and may provide a route of communication to the parotid gland and infratemporal fossa. If disease breaches the EAC it can invade several areas including the stylomastoid foramen, carotid canal, jugular foramen, petrotympanic fissure and eustachian tube.
Lymphatic spread of SCC of the temporal bone occurs in about 10% of patients whilst inflammatory lymphadenopathy occurs more commonly. Tumors of the pinna or EAC can metastasize to preauricular, infra-auricular, parotid, postauricular, or Level 2 nodes. The mucosa of the middle ear and mastoid drain to lymphatics around the eustachian tube which then drain into the deep upper jugular and retropharyngeal lymph nodes. The inner ear has no known lymphatic drainage system.
Surgical steps
Skin incisions
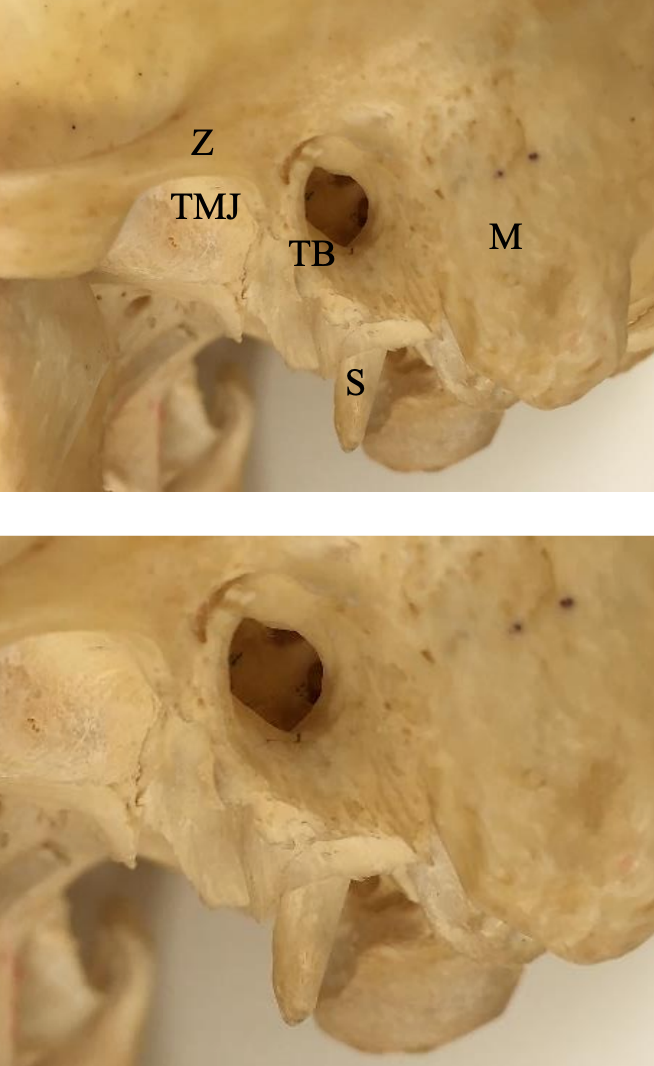
Figure 1: Lateral view of relations of EAC. TMJ = Temporomandibular joint; S = Styloid; TB = tympanic bone; M = Mastoid; Z = Zygoma
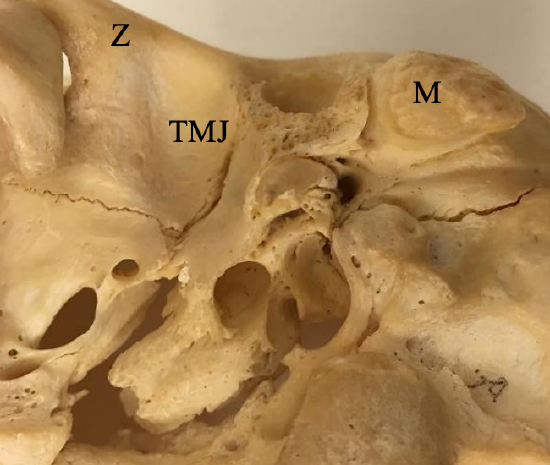
Figure 2: Inferior view of relations of EAC

Figure 3: Example of incision for lateral temporal bone resection involving concha/ tragus resection, parotidectomy and selective neck dissection
- Make a C-shaped postauricular incision (Figure 1)
- Place it far posterior to the postauricular crease so that the sigmoid sinus can be adequately exposed
- An adequate margin around the tumor is needed. This typically involves resecting part of the concha and tragus (Figure 3) or the entire pinna
- The incision can be modified depending on tumor size and location
- If a neck dissection is planned, the incision is extended into a cervical skin crease
- An anterior limb at the level of the hyoid bone is useful if a parotidectomy is to be performed
Skin flaps and soft tissue dissection

Figure 4: Skin flap elevated anteriorly around resection margins
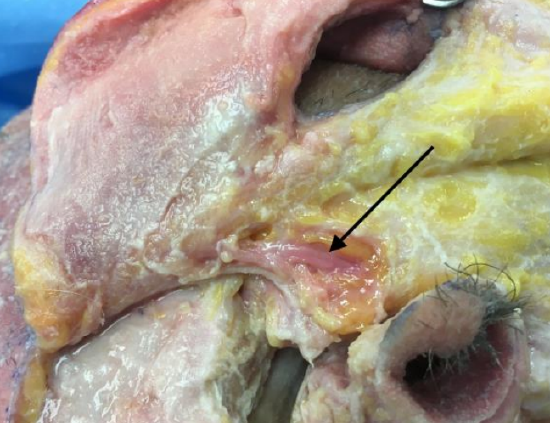
Figure 5: Skin flap elevated forwards over parotid. The superficial temporal artery has been identified and preserved (arrow)

Figure 6: Periosteum over mastoid has been excised and sent for histology. The temporalis muscle has been reflected superiorly
- Raise the skin flap from back-to-front (Figure 4)
- If a parotidectomy is required, raise the skin flap with the pinna up to the anterior border of the parotid
- Preserve the superficial temporal artery (Figure 5) to maintain the blood supply to the ear if the pinna is being preserved
- Incise the temporalis fascia and muscle along the temporal line (Figure 6)
- Expose the root of the zygoma; this is critical as it is the landmark when drilling to expose the TMJ
- Elevate the soft tissue and periosteum over the mastoid bone. This soft tissue can be excised and sent for frozen section histology (Figure 6)
Bone dissection
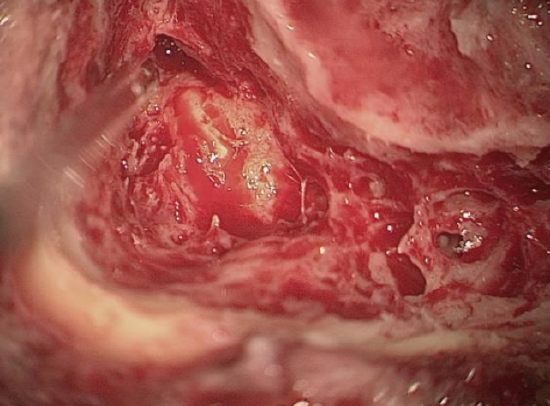
Figure 7: Skeletonize tegmen tympani and sigmoid sinus
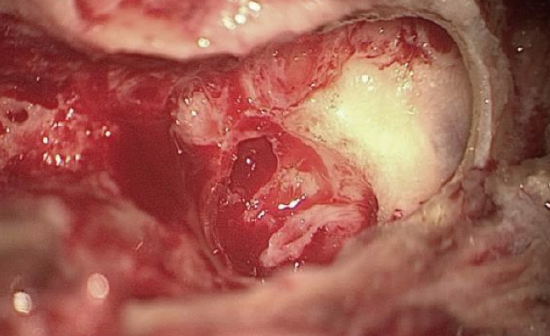
Figure 8: Drill out the mastoid tip to expose digastric ridge and retrofacial air cells
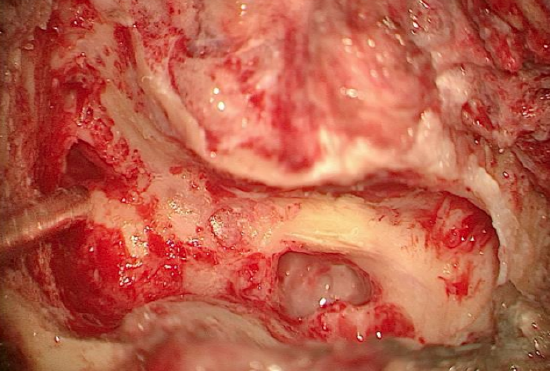
Figure 9: Skeletonize the mastoid segment of the facial nerve
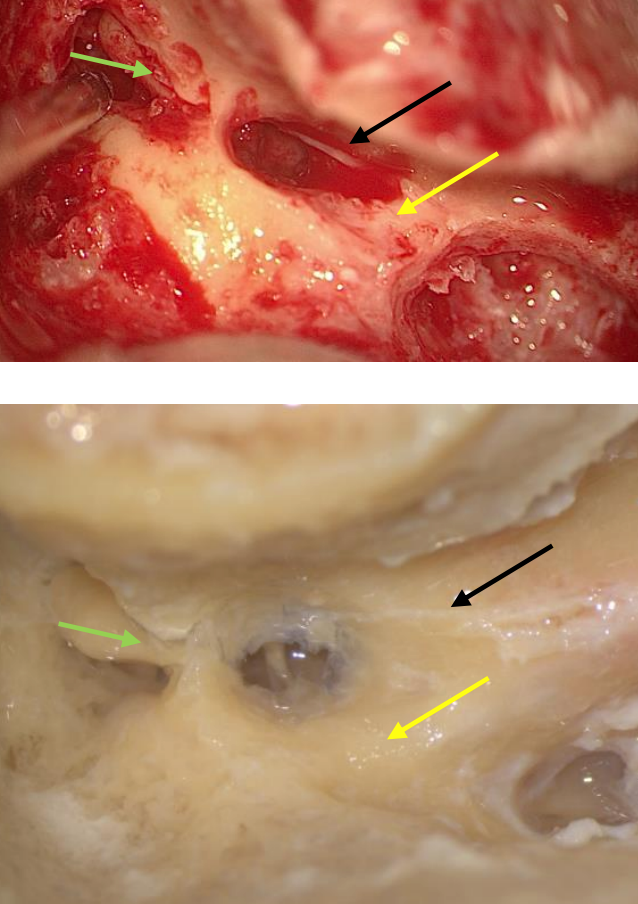
Figures 10ab: The beginnings of a posterior tympanotomy. The chorda tympani (black arrow) forms the anterior boundary and the facial nerve (yellow arrow) the posterior boundary. Note short process of incus in fossa incudes (green arrow)
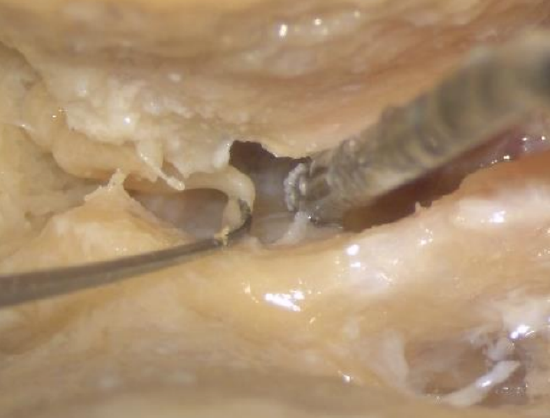
Figure 11: Disarticulating incudostapedial joint
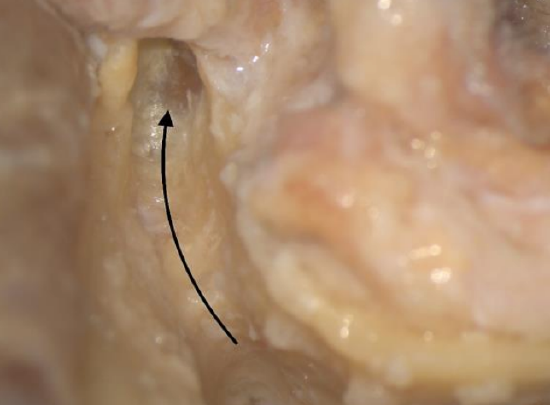
Figure 12: The curved arrow shows the drilling trajectory towards the root of zygoma. Arrowhead points to the TMJ capsule

Figure 13: The TMJ (arrow) has been exposed anterior to the ossicular heads, medial to the squamous temporal bone (I = Incus)
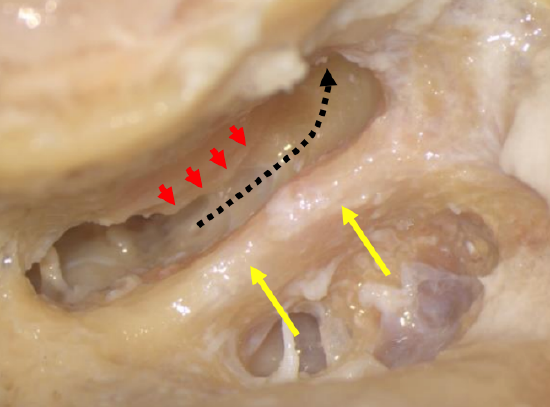
Figure 14: Extended posterior tympanotomy (chorda transected). Facial nerve (Yellow arrow), Annulus (Red arrows)
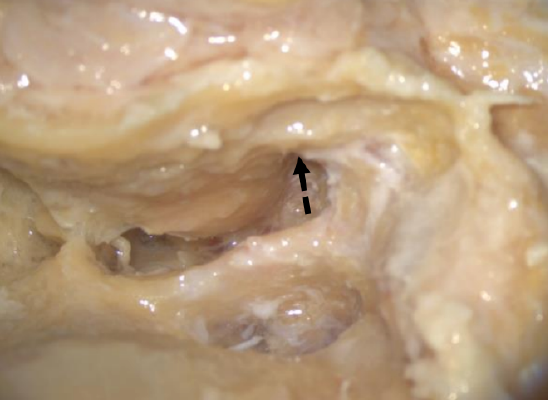
Figure 15: Drilling inferior to the ear canal

Figure 16: Gentle anterior pressure applied to the bone encasing the EAC to fracture the medial part of the anterior wall of the EAC
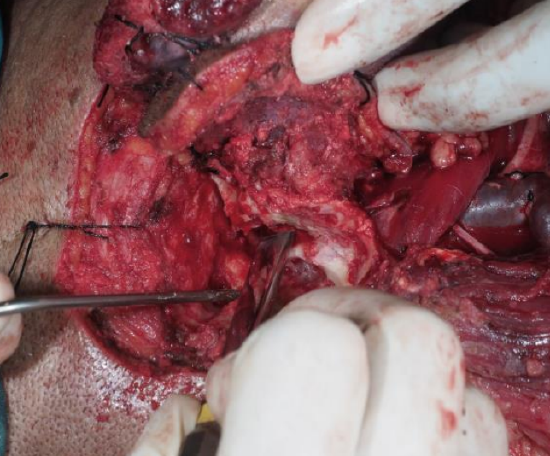
Figure 17: Curved osteotome passed medial to the TM, malleus and incus to fracture the tympanic bone
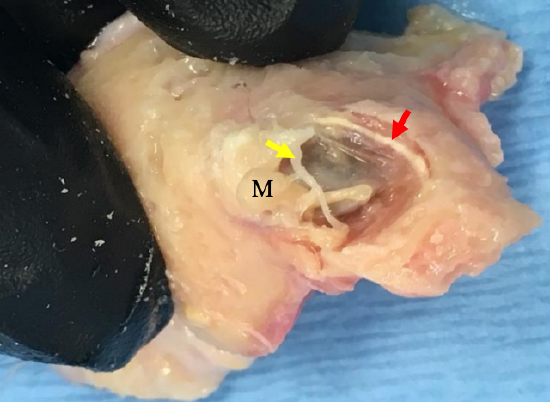
Figure 18: Surgical specimen viewed from medial side. Note the fibrous annulus (red arrow), the malleus (M), the medial surface of the EAC and the chorda tympani (yellow arrow)
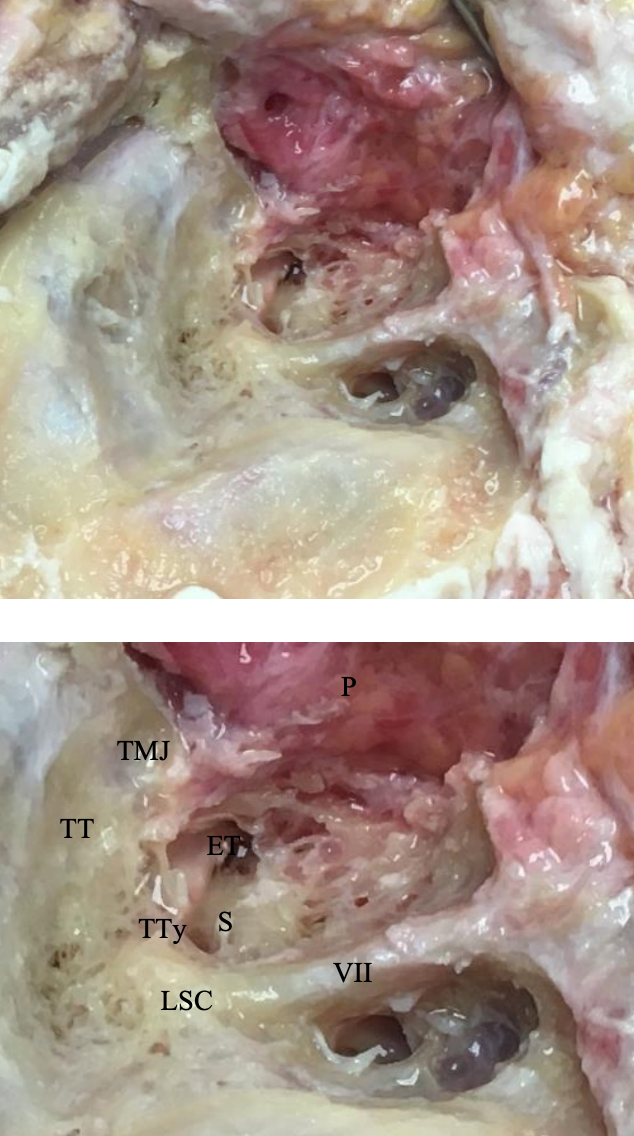
Figure 19: Surgical bed following lateral temporal bone resection; P = parotid; tensor tympani = TTy: tegmen tympani = TT; TMJ = temporomandibular joint; facial nerve = VII; Eustachian tube = ET; stapes = S; lateral semicircular canal = LSC
- Perform a cortical mastoidectomy
- Skeletonize the tegmen tympani and sigmoid sinus (Figure 7)
- Drill out the mastoid tip to expose the digastric ridge and retrofacial air cells (Figure 8)
- Skeletonize the mastoid segment of the facial nerve (Figure 9)
- Keep the posterior bony ear canal relatively thick to avoid inadvertent exposure of cancer
- Perform a posterior tympanotomy (Figures 10ab)
- Separate the incudostapedial joint with a joint knife to avoid causing sensorineural hearing loss when drilling in the epitympanum should the burr touch the ossicles (Figure 11)
- Drill the bone superior to the EAC towards the root of the zygoma in the space between the tegmen tympani and the EAC, using progressively smaller burrs (Figure 12)
- When there is limited space between the tegmen and the ear canal, it may be necessary to remove the bone of the tegmen and expose dura rather than to overthin the ear canal and expose cancer
- Use a diamond burr to avoid injuring the dura and causing a CSF leak
- Avoid sharp ledges of bone over the dura to allow good light into the surgical field
- Once one reaches the 12 o’clock position of the ear canal, direct the drilling trajectory inferiorly
- Expose the anterior epitympanum
- At this point one can remove the incus and use a malleus nipper to remove the malleus head
- Keep drilling anteriorly until the TMJ capsule becomes apparent. It is soft and whiter in color (Figures 12, 13)
- Ensure that the TMJ capsule is exposed all the way from the ossicular heads medially to the squamous temporal bone laterally
- Perform an extended posterior tympanotomy by drilling inferiorly along the anterior border of the mastoid segment of the facial nerve – this requires transection of the chorda; the fibrous (tympanic) annulus becomes the medial border of the resection (Figure 14)
- Continue the dissection inferior to the bony ear canal in an anterolateral direction (deep to superficial) towards the glenoid fossa
- It is important to use the correct burr: Never use a cutting burr as one needs a longer burr to drill anteriorly. It is dangerous to use a cutting burr, as a long cutting burr can “jump” risking injury to the carotid and jugular bulb. An appropriate sized (2-2.5 mm) diamond burr should rather be used
- It is important to check the height of the jugular bulb on the CT scan to ensure that the jugular bulb is not inadvertently injured!
- Continue drilling until soft tissue is encountered (Figure 15)
- The 2nd author (TH) favors a different technique to reduce the risk of the drill injuring the carotid. She drills into the bone in the hypotympanum under direct vision to weaken it, then switches to an osteotome which is directed lateral to the Eustachian tube (carotid forms medial wall of Eustachian tube)
- With an anterior sigmoid sinus, a favorable angle for drilling is obtained by ensuring the bone over the sigmoid is removed - this enables a flatter trajectory so that the jugular bulb and carotid are avoided
- While drilling, it is useful to gently rock the block of bone encasing the EAC anteriorly to determine where it is still attached
- With TMJ capsule exposed superiorly, and glenoid cavity exposed inferiorly, only the thin tympanic bone remains intact anteriorly and is therefore the only remaining bony attachment of the block of bone enclosing the EAC
- Apply gentle anterograde pressure to fracture this thin tympanic bone of the anterior canal (Figure 16)
- If the bone does not fracture readily, then a 2 mm osteotome or 2 mm burr can be used through the posterior tympanotomy to fracture the anterior ear canal
- Alternatively, a curved osteotome is passed medial to the TM, malleus and incus (this has been removed) to fracture the tympanic bone, taking care to remain lateral to the Eustachian tube (internal carotid artery passes medial to Eustachian tube). A useful trick is to turn the osteotome so that the bevelled edge faces the promontory and to angle the osteotome so that it points upwards (Figure 17)
- At this point, the anterior soft tissue attachments of the EAC can be dissected to remove the bone encasing the EAC with the TM and malleus (Figures 18 and 19)
Managing bleeding
- Minor sigmoid sinus bleeds with intact bone around the sinus can be controlled with bone wax
- Bleeding from the sigmoid sinus can be managed with application of hemostatic agents such as Haemopatch, Surgicel or Flowseal with a patty for compression. It is important to remember that venous bleeding should not cause panic and gentle pressure is much better than undue force which will only make the bleeding site widen.
- Jugular bulb bleeding can be more troublesome. A small bleed from the bulb tip can easily be dealt with using bone wax. However, significant bleeding can occur because of excess force used when cracking off the last bony attachments, leading to the bone fracturing along the jugular bulb or even the carotid canal.
- This can occur if the bone of the styloid apparatus has not been adequately drilled off the tympanic ring or there has been inadequate drilling around the anterior canal towards the glenoid fossa inferiorly. Jugular bulb bleeding at this site can rapidly fill the surgical field due to brisk sigmoid and inferior petrosal sinus blood flow. Sternocleidomastoid muscle can be mobilized and applied with gentle pressure to plug the area. Free muscle can be oversewn between the glenoid/ parotid tissue and the sternomastoid muscle as a patch. In the event of uncontrolled bleeding, the jugular vein is ligated in the upper neck and the sigmoid sinus and inferior petrosal sinuses are packed with Surgicel through the tear in the jugular bulb.
- The 2nd author applies pressure by packing with Surgicel, then ligates the jugular vein in the neck and the sigmoid in the mastoid cavity
- Skeletonize the sigmoid sinus, then remove the thin shell of bone over a small section of the sigmoid by using a Plester knife
- Use an aneurysm needle threaded with a double silk ligature and pass it behind the sigmoid sinus by making small slits in the dura next to the sigmoid sinus. Remove the needle, leaving behind the double ligature and tie these. This may cause a small CSF leak. This can be plugged using fat
- Complete the operation by obliterating the cavity with a temporalis muscle flap

Figure 20: Aneurysm needle
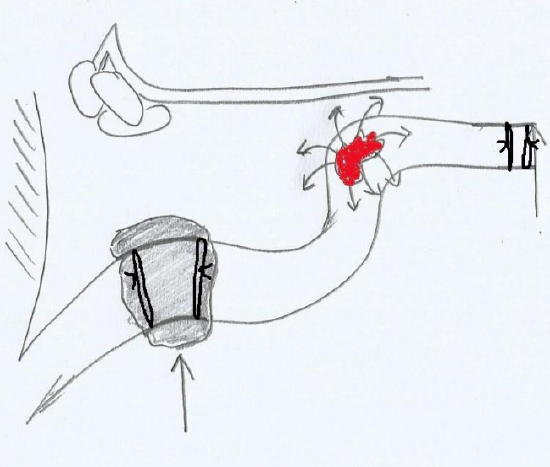
Figure 21: Double ligatures tied around sigmoid sinus
Ancillary procedures
Parotidectomy: If parotidectomy is to be done, it is best to do it before the lateral temporal bone resection. Superficial parotidectomy is usually performed for T1/2 tumors. Total parotidectomy is done for T3/4 tumors. For BCC without parotid invasion, parotidectomy is not required.
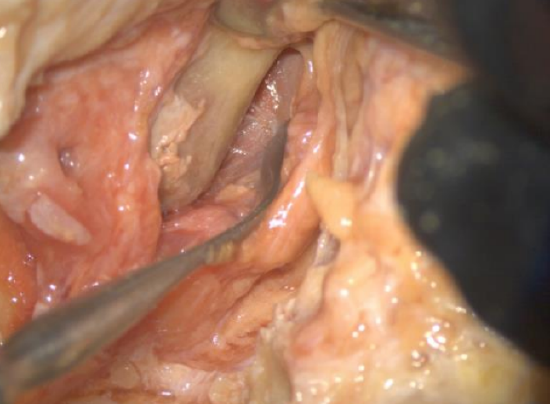
Figure 22: Exposure of mandibular condyle. An incision has been made on the condyle and the periosteum has been elevated so that it can be drilled
Temporomandibular joint: If tumor extends into or near the TMJ, a partial mandibulectomy is performed. Typically, this involves a condylectomy (Figure 22), but for more extensive disease the resection may extend from the mandibular notch to the angle of mandible.
Neck dissection: For SCC with or without nodal metastasis, neck dissection including Levels 1b, 2-5 should be considered.
Reconstruction

Figure 23: Temporalis muscle reflected over temporal bone defect

Figure 24: Split skin graft over temporalis muscle
If the pinna is preserved but the concha and tragus are removed, then reconstruction can be performed using a pedicled muscle flap e.g. temporalis muscle can be rotated over the cavity and sutured to the sternocleidomastoid muscle (Figure 23). The canal can be oversewn and the pinna placed back in position. If the pinna is resected, a split skin graft can also be placed over the temporalis muscle: this usually works quite well if one can’t do a free flap (Figure 24).

Figure 25: Cervicofacial flap
- An alternative is to fashion an open mastoid cavity, but such a cavity will take a long time to heal and regular debridement in the office is required
- When the pinna is removed, local flaps (temporalis; cervicofacial (Figure 25), submental, supraclavicular (See clinical example), latissimus dorsi) or free flaps are required. The anterolateral thigh flap is a particularly useful flap as it provides both bulk and skin cover.
- Bone anchored hearing aids are an excellent choice for rehabilitation. Ideally it should be fitted at the time of the resection, as irradiation may compromise osseointegration. Although there may be some artifact with CT scans, most bone anchored hearing aid systems are MRI safe up to 3T with no adverse effects.
- Nonimplanted bone conduction hearing aids or even contralateral routing of sound hearing aids can also be used
Related procedures
Sleeve resection: This can be done for nonaggressive tumors of the cartilaginous EAC without bony invasion. However, patients rarely present early enough for it to be done.
Near-total temporal bone resection: This should be considered for tumors extending medial to the TM or into the mastoid. The resection involves removing the temporal bone leaving only the petrous apex attached to the clivus. The facial and vestibulocochlear nerves are sacrificed. The surgical technique involves a temporal craniotomy, transmastoid and transcervical approaches. If dura is involved, it can be resected with the specimen, but involvement of the brain implies the tumor should be considered incurable.
Total temporal bone resection: This involves en bloc resection of the temporal bone including the petrous apex and sigmoid sinus. There is no evidence that this improves survival and is not part of the authors’ practice.
Clinical Example

Figure 26: Extensive squamous cell carcinoma
This patient had extensive squamous carcinoma of the pinna extending into the ear canal and the parotid and nodal metastases. The incision was extended into the neck (“hockey stick”) for a modified radical neck dissection and parotidectomy (Figure 26). The facial nerve was intact and a superficial parotidectomy was done by retrograde dissection of the facial nerve.

Figure 27: Mastoid being exposed after neck dissection and superficial parotidectomy have been completed
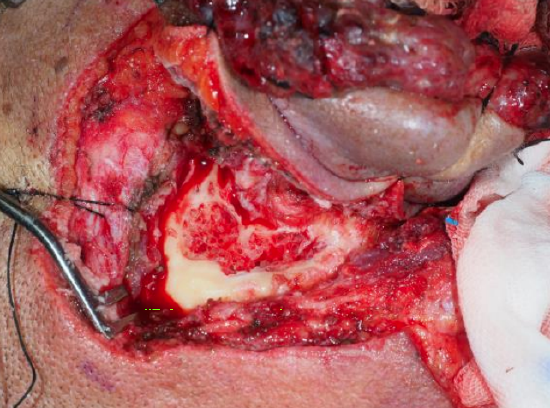
Figure 28: Commencement of cortical mastoidectomy
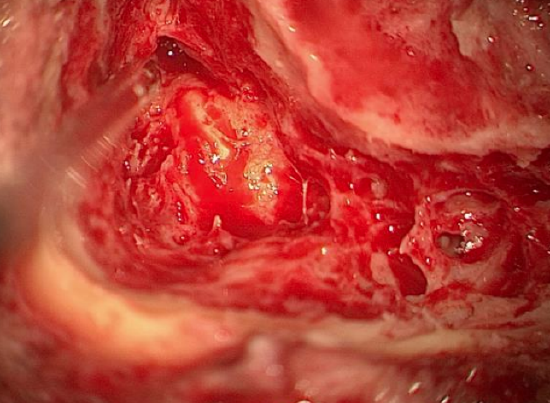
Figure 29: Cortical mastoidectomy with exposure of lateral semicircular canal
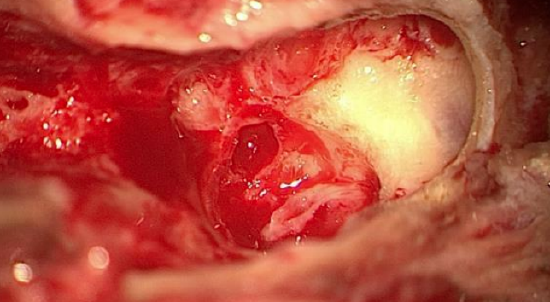
Figure 30: Mastoid tip drilled to expose digastric ridge
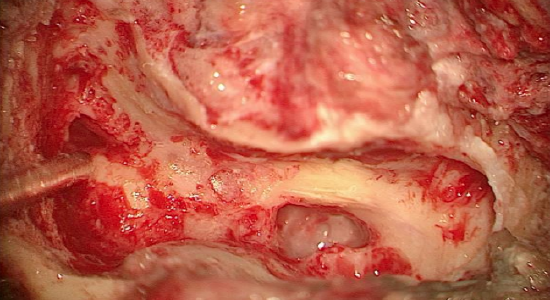
Figure 31: Mastoid segment of facial nerve exposed
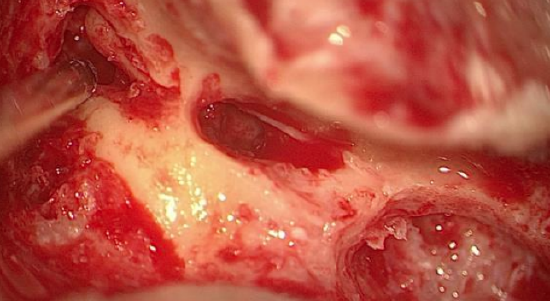
Figure 32: Posterior tympanotomy with chorda tympani visible; sucker tip points to incus
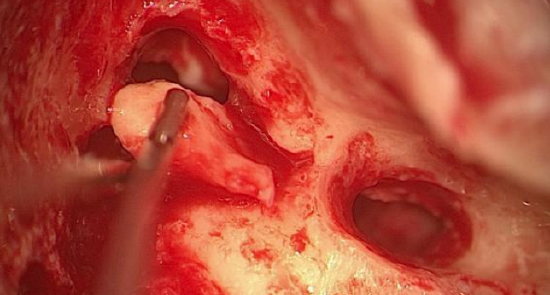
Figure 33: Incus being removed
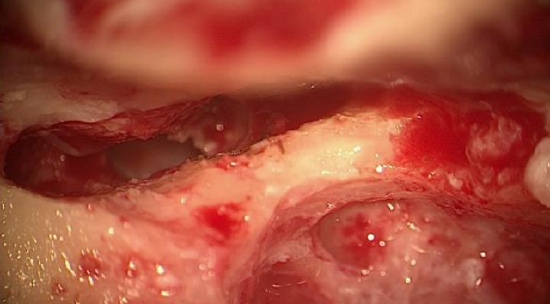
Figure 34: Completed extended posterior tympanotomy
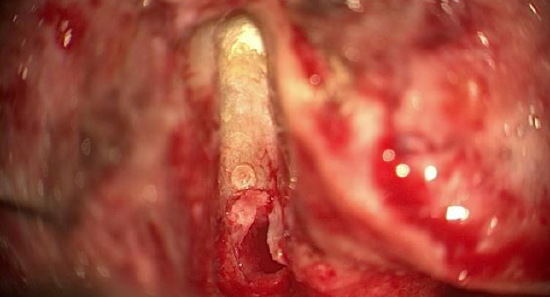
Figure 35: Drilling superiorly toward TMJ
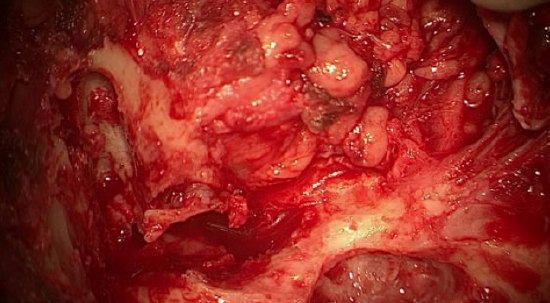
Figure 36: Drilling superiorly toward TMJ
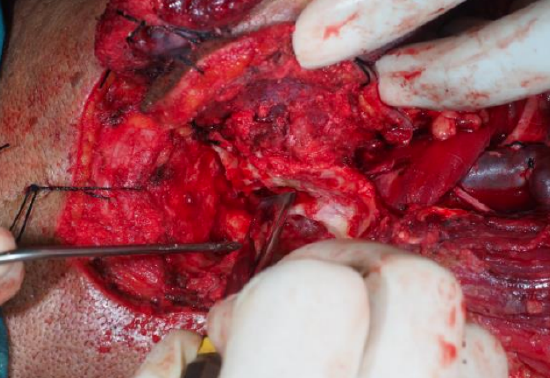
Figure 37: Osteotome used fracture anterior tympanic bone
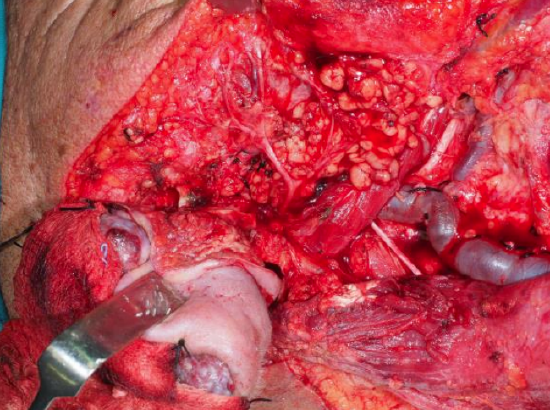
Figure 38: Before removal of specimen
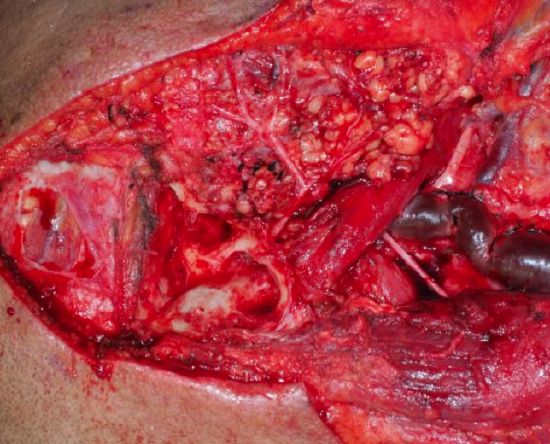
Figure 39: View of completed lateral temporal bone resection and superficial parotidectomy and neck dissection
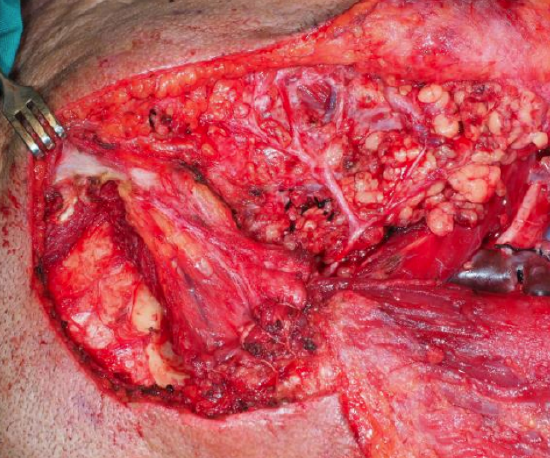
Figure 40: Temporalis muscle reflected over temporal bone defect
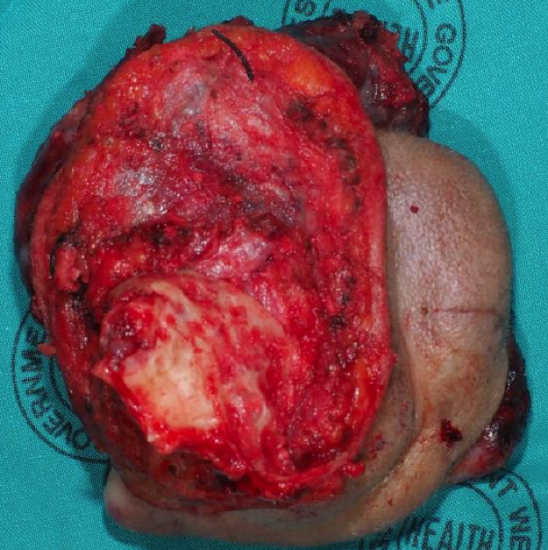
Figure 41: Medial view of specimen

Figure 42: Lateral view of specimen

Figure 43: Supraclavicular flap

Figure 44: Supraclavicular flap
References
- Ho B, Solares CA, Panizza B. Temporal bone resection. Operative Techniques in Otolaryngology, 2013;24:179-83
- Chung SJ and Pensak ML. Tumors of the temporal bone. In Neurotology 2nd edition, eds Jackler RK and Brackmann DE, 2005, Mosby Inc
- Arriaga MA and Leonetti JP. Malignancies of the temporal bone - limited temporal bone resection. In Otologic Surgery 3rd edition, editors Brackmann D, Shelton C, Arriaga M, 2009, Saunders
- Homer JJ, Lesser T, Moffat D et al. Management of lateral skull base cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016. 130(S2),S119-S124
Authors
Rajeev Mathew MBBS, MA, PhD, FRCS
Senior Registrar
ENT Surgery
St George’s Hospital NHS Foundation
Trust
Tooting, London
Rajeev.mathew@nhs.net
Tashneem Harris MBChB, FCORL, MMed (Otol)
Fisch Instrument Microsurgical Fellow
ENT Specialist
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
harristasneem@yahoo.com
Parag Patel MBBS, BSc (Hons), MSc, FRCS
Consultant ENT Surgeon
Clinical Lead for Skull Base Surgery
St George’s Hospital NHS Foundation
Trust
Tooting, London
Parag.patel2@nhs.net
Editor
Johan Fagan MBChB, FCS (ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


