11.2: Patent Ductus Arteriosus
- Page ID
- 42786
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Case report
Introduction
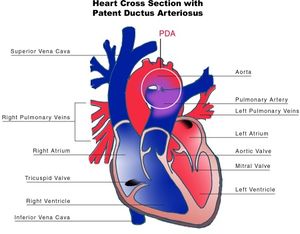
The ductus arteriosus (DA) is a fetal vascular connection between the main pulmonary artery and the descending aorta that diverts blood away from the pulmonary bed (Figure 11.2.1). After birth, the DA undergoes active constriction and eventual obliteration. A patent ductus arteriosus (PDA) occurs when the ductus fails to completely close postnatally.
The incidence of PDA has increased dramatically over the last two decades. This is due to the improved survival rate of premature infants, because the incidence of PDA significantly increases in infants born before 30 weeks gestation.
The reported incidence of an isolated PDA among term infants ranges from 0.03 to 0.08 percent.
There is a female predominance for PDA with a 2:1 female to male ratio in most case series of term infants. The incidence of PDA is also greater in infants born at high altitude compared to those born at sea level, and in infants with congenital rubella.
PDA may present with other congenital heart lesions, especially those associated with hypoxemia. PDA should be considered when the clinical features of left-to-right shunt seem out of proportion to the particular lesion being considered.
Evaluation
The clinical manifestations of a PDA are determined by the degree of left-to-right shunting, which is dependent upon the size and length of the PDA, and the difference between pulmonary and systemic vascular resistances.
The hemodynamic consequences of the PDAs can be categorized by the degree of left-to-right shunting based upon the pulmonary to systemic flow ratio (Qp:Qs) [21].
- Small — Qp:Qs <1.5 to 1
- Moderate — Qp:Qs between 1.5 and 2.2 to 1
- Large — Qp:Qs >2.2 to 1
Typical findings during physical examination are a continuous murmur and a low diastolic blood pressure. In small shunts the ECG and chest x-ray are normal. In larger left-to-right shunts signs of left atrial and left ventricular overload might be present.
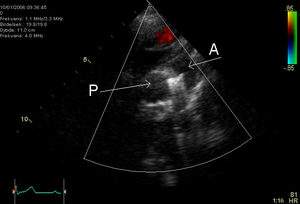
Echocardiography is a very sensitive and specific method to identify the left-to-right shunt.
Treatment and outcome
Patients with an open PDA have an increased risk of infectious endarteritis, heart failure, pulmonary hypertension and most of these patients become symptomatic in adulthood. Patients with a non-restrictive PDA rarely reach adulthood, unless the pulmonary vascular resistance increases leading to a decrease in left ventricular overload. This hemodynamic state is known as Eisenmenger syndrome in which the shunt is reversed and there is cyanosis present. Patients in who the ductus is closed in childhood have a normal life expectancy.
In patients with a PDA, the primary management decision is whether to actively close the PDA, or to conservatively observe and monitor the patient's cardiac status on a regular basis.
PDA closure is recommended for patients with a significant left-to-right shunt who are symptomatic, have evidence of left-sided volume overload or have reversible pulmonary arterial hypertension. Closure results in resolution of symptoms and a decrease in the likelihood or severity of PAH, and the development of irreversible pulmonary vascular disease (Eisenmenger syndrome).
PDA closure is not recommended in patients with severe and irreversible PAH because of the procedural risk, the fact that closure does not improve survival, and right to left ductal shunting may be necessary to maintain cardiac output during episodes of increasing pulmonary vascular resistance.
Interventions for PDA closure include: pharmacological treatment which is used exclusively in premature infants, surgical ligation or percutaneous catheter occlusion. Surgical closure has a low mortality (<1%) in children and young adults. In adult patients the perioperative risk is increased (around 3%) due to a higher rate of complications like bleeding, heart failure in a compromised left ventricular function and damage to the recurrent laryngeal nerve or phrenic nerve.
Percutaneous PDA occlusion was first introduced in 1967 and provides an alternative to surgical ligation. Many different techniques have been developed, however the two techniques most commonly used are coils or occlusion devices. Both techniques lead to a full occlusion of the PDA and normalization of left ventricular hemodynamics.


