14.3: Common Integumentary Conditions
- Page ID
- 44630
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Now that we have reviewed the anatomy of the integumentary system, let’s review common conditions that you may find during a routine integumentary assessment.
Acne
Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands, such as the face and back. It is most common during puberty due to associated hormonal changes that stimulate the release of sebum. An overproduction and accumulation of sebum, along with keratin, can block hair follicles. Acne results from infection by acne-causing bacteria and can lead to potential scarring.[1] See Figure \(\PageIndex{1}\)[2] for an image of acne.

Lice and Nits
Head lice are tiny insects that live on a person’s head. Adult lice are about the size of a sesame seed, but the eggs, called nits, are smaller and can appear like a dandruff flake. See Figure \(\PageIndex{2}\)[3] for an image of very small white nits in a person’s hair. Children ages 3-11 often get head lice at school and day care because they have head-to-head contact while playing together. Lice move by crawling and spread by close person-to-person contact. Rarely, they can spread by sharing personal belongings such as hats or hair brushes. Contrary to popular belief, personal hygiene and cleanliness have nothing to do with getting head lice. Symptoms of head lice include the following:
- Tickling feeling in the hair
- Frequent itching, which is caused by an allergic reaction to the bites
- Sores from scratching, which can become infected with bacteria
- Trouble sleeping due to head lice being most active in the dark
A diagnosis of head lice usually comes from observing a louse or nit on a person’s head. Because they are very small and move quickly, a magnifying lens and a fine-toothed comb may be needed to find lice or nits. Treatments for head lice include over-the-counter and prescription shampoos, creams, and lotions such as permethrin lotion.[4]

Burns
A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can lead to a massive loss of fluid due to loss of the skin’s protection. Burned skin is also extremely susceptible to infection due to the loss of protection by intact layers of skin.
Burns are classified by the degree of their severity. A first-degree burn, also referred to as a superficial burn, only affects the epidermis. Although the skin may be painful and swollen, these burns typically heal on their own within a few days. Mild sunburn fits into the category of a first-degree burn. A second-degree burn, also referred to as a partial thickness burn, affects both the epidermis and a portion of the dermis. These burns result in swelling and a painful blistering of the skin. It is important to keep the burn site clean to prevent infection. With good care, a second degree burn will heal within several weeks. A third-degree burn, also referred to as a full thickness burn, extends fully into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns that require immediate medical attention. A fourth-degree burn, also referred to as a deep full thickness burn, is even more severe, affecting the underlying muscle and bone. Third- and fourth-degree burns are usually not as painful as second degree burns because the nerve endings are damaged. Full thickness burns require debridement (removal of dead skin) followed by grafting of the skin from an unaffected part of the body or from skin grown in tissue culture.[5] See Figure \(\PageIndex{3}\)[6] for an image of a patient recovering from a second-degree burn on the hand.

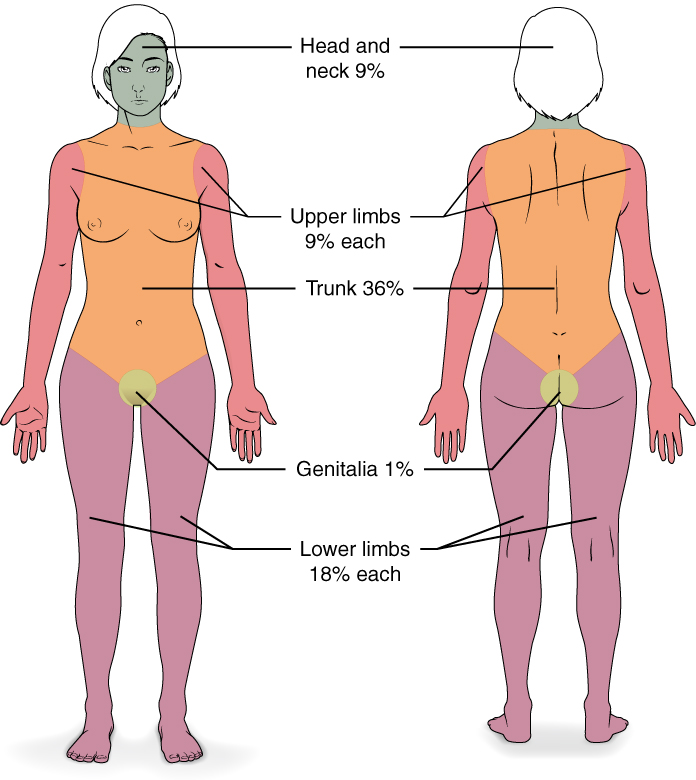
Severe burns are quickly measured in emergency departments using a tool called the “rule of nines,” which associates specific anatomical locations with a percentage that is a factor of nine. Rapid estimate of the burned surface area is used to estimate intravenous fluid replacement because patients will have massive fluid losses due to the removal of the skin barrier.[7] See Figure \(\PageIndex{4}\)[8] for an illustration of the rule of nines. The head is 9% (4.5% on each side), the upper limbs are 9% each (4.5% on each side), the lower limbs are 18% each (9% on each side), and the trunk is 36% (18% on each side).
Scars
Most cuts and wounds cause scar formation. A scar is collagen-rich skin formed after the process of wound healing. Sometimes there is an overproduction of scar tissue because the process of collagen formation does not stop when the wound is healed, resulting in the formation of a raised scar called a keloid.[9] Keloids are more common in patients with darker skin color. See Figure \(\PageIndex{5}\)[10] for an image of a keloid that has developed from a scar on a patient’s chest wall.

Skin Cancer
Skin cancer is common, with one in five Americans experiencing some type of skin cancer in their lifetime. Basal cell carcinoma is the most common of all cancers that occur in the United States and is frequently found on areas most susceptible to long-term sun exposure such as the head, neck, arms, and back. Basal cell carcinomas start in the epidermis and become an uneven patch, bump, growth, or scar on the skin surface. Treatment options include surgery, freezing (cryosurgery), and topical ointments.[11]
Squamous cell carcinoma presents as lesions commonly found on the scalp, ears, and hands. If not removed, squamous cell carcinomas can metastasize to other parts of the body. Surgery and radiation are used to cure squamous cell carcinoma. See Figure \(\PageIndex{6}\)[12] for an image of squamous cell carcinoma.[13]

Melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the pigment-producing cells in the epidermis. A melanoma commonly develops from an existing mole. See Figure \(\PageIndex{7}\)[14] for an image of a melanoma. Melanoma is the most fatal of all skin cancers because it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface. Treatment includes surgical excision and immunotherapy.[15]

Fungal (Tinea) Infections
Tinea is the name of a group of skin diseases caused by a fungus. Types of tinea include ringworm, athlete’s foot, and jock itch. These infections are usually not serious, but they can be uncomfortable because of the symptoms of itching and burning. They can be transmitted by touching infected people, damp surfaces such as shower floors, or even from pets.[16] Ringworm (tinea corporis) is a type of rash that forms on the body that typically looks like a red ring with a clear center, although a worm doesn’t cause it. Scalp ringworm (tinea capitals) causes itchy, red patches on the head that can leave bald spots. Athlete’s foot (tinea pedis) causes itching, burning, and cracked skin between the toes. Jock itch (tinea cruris) causes an itchy, burning rash in the groin area. Fungal infections are often treated successfully with over-the-counter creams and powders, but some require prescription medicine such as nystatin. See Figure \(\PageIndex{8}\)[17] for an image of a tinea in a patient’s groin.[18]

Impetigo
Impetigo is a common skin infection caused by bacteria in children between the ages two and six. It is commonly caused by Staphylococcus (staph) or Streptococcus (strep) bacteria. See Figure \(\PageIndex{9}\)[19] for an image of impetigo. Impetigo often starts when bacteria enter a break in the skin, such as a cut, scratch, or insect bite. Symptoms start with red or pimple-like sores surrounded by red skin. The sores fill with pus and then break open after a few days and form a thick crust. They are often itchy, but scratching them can spread the sores. Impetigo can spread by contact with sores or nasal discharge from an infected person and is treated with antibiotics.

Edema
Edema is caused by fluid accumulation within the tissues often caused by underlying cardiovascular or renal disease. Read more about edema in the “Basic Concepts” section of the “Cardiovascular Assessment” chapter.
Lymphedema
Lymphedema is the medical term for a type of swelling that occurs when lymph fluid builds up in the body’s soft tissues due to damage to the lymph system. It often occurs unilaterally in the arms or legs after surgery has been performed that injured the regional lymph nodes. See Figure \(\PageIndex{10}\)[20] for an image of lower extremity edema. Causes of lymphedema include infection, cancer, scar tissue from radiation therapy, surgical removal of lymph nodes, or inherited conditions. There is no cure for lymphedema, but elevation of the affected extremity is vital. Compression devices and massage can help to manage the symptoms. See Figure \(\PageIndex{11}\)[21] for an image of a specialized compression dressing used for lymphedema. It is also important to remember to avoid taking blood pressure on a patient’s extremity with lymphedema.[22]


Jaundice
Jaundice causes skin and sclera (whites of the eyes) to turn yellow. See Figure \(\PageIndex{12}\)[23] for an image of a patient with jaundice visible in the sclera and the skin. Jaundice is caused by too much bilirubin in the body. Bilirubin is a yellow chemical in hemoglobin, the substance that carries oxygen in red blood cells. As red blood cells break down, the old ones are processed by the liver. If the liver can’t keep up due to large amounts of red blood cell breakdown or liver damage, bilirubin builds up and causes the skin and sclera to appear yellow. New onset of jaundice should always be reported to the health care provider.
Many healthy babies experience mild jaundice during the first week of life that usually resolves on its own, but some babies require additional treatment such as light therapy. Jaundice can happen at any age for many reasons, such as liver disease, blood disease, infections, or side effects of some medications.[24]

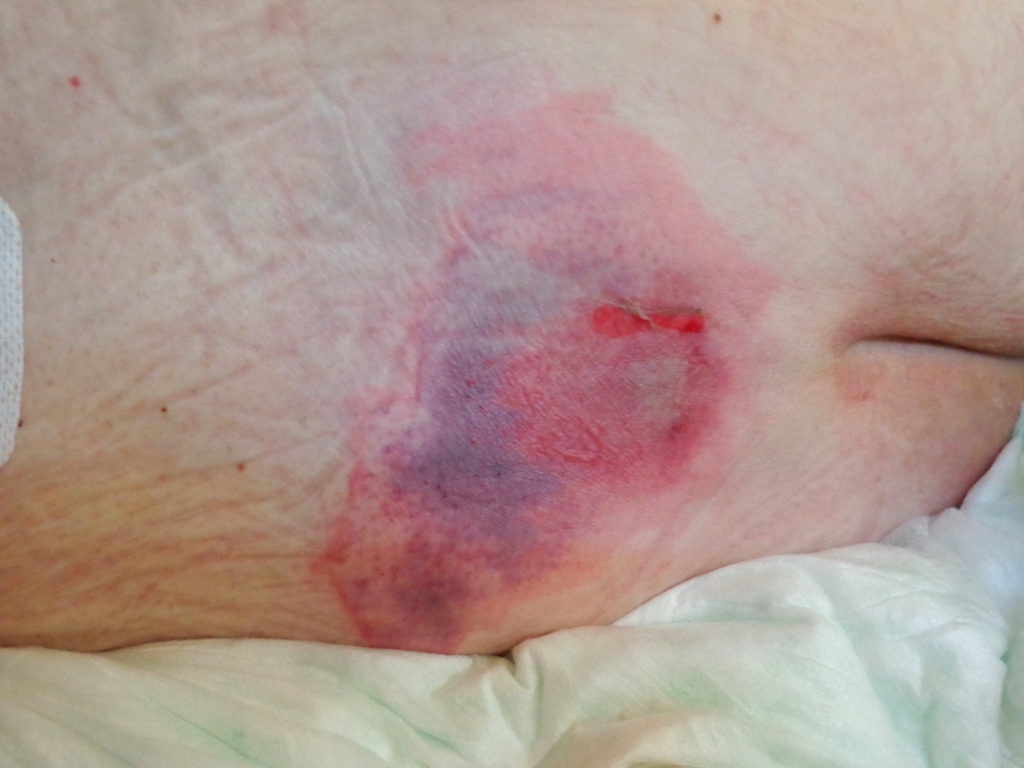
Pressure Injuries
Pressure injuries also called bedsores, form when a patient’s skin and soft tissue press against a hard surface, such as a chair or bed, for a prolonged period of time. The pressure against a hard surface reduces blood supply to that area, causing the skin tissue to become damaged and become an ulcer. Patients are at high risk of developing a pressure injury if they spend a lot of time in one position, have decreased sensation, or have bladder or bowel leakage.[25] See Figure \(\PageIndex{13}\)[26] for an image of a pressure ulcer injury on a bed-bound patient’s back. Read more information about assessing and caring for pressure injury in the “Wound Care” chapter.
Petechiae
Petechiae are tiny red dots caused by bleeding under the skin that may appear like a rash. Large petechiae are called purpura. An easy method used to assess for petechiae is to apply pressure to the rash with a gloved finger. A rash will blanch (i.e., whiten with pressure) but petechiae and purpura do not blanch. See Figure \(\PageIndex{14}\)[27] for an image of petechiae and purpura. New onset of petechiae should be immediately reported to the health care provider because it can indicate a serious underlying medical condition.[28]

- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- “Acne vulgaris on a very oily skin.jpg” by Roshu Bangal is licensed under CC BY-SA 4.0↵
- “Fig.5. Louse nites.jpg” by KostaMumcuoglu at English Wikipedia is licensed under CC BY-SA 3.0↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Aug 17]. Head lice; [reviewed 2016, Sep 9; cited 2020, Sep 18]. https://medlineplus.gov/headlice.html↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- “1Veertje hand-burn-do8.jpg” by 1Veertje is licensed under CC BY-SA 3.0↵
- This work is a derivative of StatPearls by Moore, Waheed, and Burns and is licensed under CC BY 4.0↵
- “513 Degree of burns.jpg” by OpenStax is licensed under CC BY 3.0↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- “Keloid-Butterfly, Chest Wall.JPG” by Htirgan is licensed under CC BY-SA 3.0↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- “Squamous cell carcinoma (3).jpg” by unknown photographer, provided by National Cancer Institute is licensed under CC0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/5-4-diseases-disorders-and-injuries-of-the-integumentary-system↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- “Melanoma (2).jpg” by unknown photographer, provided by National Cancer Instituteis in the Public Domain. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/5-4-diseases-disorders-and-injuries-of-the-integumentary-system↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Aug 17]. Tinea infections; [reviewed 2016, Apr 4; cited 2020, Sep 18]. https://medlineplus.gov/tineainfections.html#:~:text=Tinea%20is%20the%20name%20of,or%20even%20from%20a%20pet↵
- “Tinea cruris.jpg” by Robertgascoin is licensed under CC BY-SA 3.0↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Aug 17]. Tinea infections; [reviewed 2016, Apr 4; cited 2020, Sep 18]. https://medlineplus.gov/tineainfections.html#:~:text=Tinea%20is%20the%20name%20of,or%20even%20from%20a%20pet↵
- “Impetigo2020.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0↵
- "Lymphedema_limbs.JPG" by medical doctors is licensed under CC BY-SA 4.0↵
- "Adaptive_Kompressionsbandage_mit_Fußteil.jpg" by Enteris in the Public Domain↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Aug 27]. Lymphedema; [reviewed 2019, Jan 22; cited 2020, Sep 18]. https://medlineplus.gov/lymphedema.html↵
- “Cholangitis Jaundice.jpg” by Bobjgalindo is licensed under CC BY-SA 4.0↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2019, Oct 22]. Jaundice; [reviewed 2016, Aug 31; cited 2020, Sep 18]. https://medlineplus.gov/jaundice.html↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Preventing pressure ulcers; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/patientinstructions/000147.htm↵
- “Decubitus 01.jpg” by AfroBrazilian is licensed under CC BY-SA 3.0↵
- “Purpura.jpg” by User:Hektor is licensed under CC BY-SA 3.0↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Bleeding into the skin; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/003235.htm↵


