5: Clinical Issues Across Assessment
- Page ID
- 16031
IN THIS CHAPTER
- Trauma-Informed Prevention and Treatment Objectives
- Treatment Issues
- Making Referrals to Trauma-Specific Services
Many clients in behavioral health treatment may have histories of trauma, so counselors should be prepared to help them address issues that arise from those histories. This chapter begins with a thorough discussion of trauma-informed prevention and treatment objectives along with practical counselor strategies. Specific treatment issues related to working with trauma survivors in a clinical setting are discussed as well, including client engagement, pacing and timing, traumatic memories, and culturally appropriate and gender-responsive services. The chapter ends with guidelines for making referrals to trauma-specific services.
Trauma-Informed Prevention and Treatment Objectives
Trauma-informed care (TIC) not only focuses on identifying individuals who have histories of trauma and traumatic stress symptoms; it also places considerable effort in creating an environment that helps them recognize the impact of trauma and determine the next course of action in a safe place. For some individuals, psychoeducation and development or reinforcement of coping strategies will be the most suitable and effective strategy, whereas others may request or warrant a referral for more trauma-specific interventions (see Part 1, Chapter 6, of this Treatment Improvement Protocol [TIP]). Although research is limited in the area of building resilience to prevent exacerbation of trauma symptoms and traumatic stress disorders, TIC also focuses on prevention strategies to avoid retraumatization in treatment, to promote resilience, and to prevent the development of trauma-related disorders. The following sections highlight key trauma-informed prevention and treatment objectives.
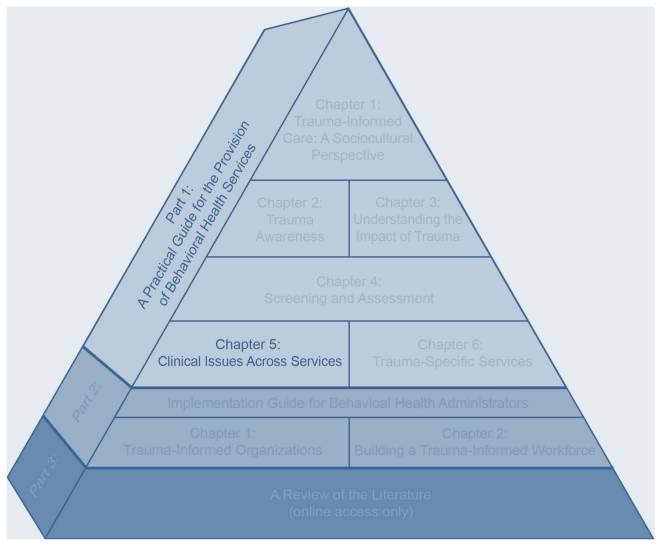
TIC Framework in Behavioral Health Services—Clinical Issues Across Services
Establish Safety
Beyond identifying trauma and trauma-related symptoms, the initial objective of TIC is establishing safety. Borrowing from Herman’s (1992) conceptualization of trauma recovery, safety is the first goal of treatment. Establishing safety is especially crucial at the outset of trauma-informed treatment and often becomes a recurrent need when events or therapeutic changes raise safety issues, such as a change in treatment staffing due to vacations.
In the context of TIC, safety has a variety of meanings. Perhaps most importantly, the client has to have some degree of safety from trauma symptoms. Recurring intrusive nightmares; painful memories that burst forth seemingly without provocation; feelings of sadness, anger, shame, or being overwhelmed; or not having control over sudden disconnections from others make moment-to-moment living feel unsafe. Clients might express feeling unsafe through statements such as, “I can’t control my feelings,” or, “I just space out and disconnect from the world for no reason,” or, “I’m afraid to go to sleep because of the nightmares.” The intense feelings that accompany trauma can also make clients feel unsafe. They may wake up in the morning feeling fine but become immobilized by depression as the day progresses. Clients with histories of trauma may experience panicky feelings of being trapped or abandoned. An early effort in trauma treatment is thus helping the client gain more control over trauma symptoms (and be able to label them as such) by learning more about the client and helping him or her develop new coping skills to handle symptoms when they arise and stay more grounded when flooded with feelings or memories.
Advice to Counselors: Strategies To Promote Safety
Strategy #1: Teach clients how and when to use grounding exercises when they feel unsafe or overwhelmed.
Strategy #2: Establish some specific routines in individual, group, or family therapy (e.g., have an opening ritual or routine when starting and ending a group session). A structured setting can provide a sense of safety and familiarity for clients with histories of trauma.
Strategy #3: Facilitate a discussion on safe and unsafe behaviors. Have clients identify, on paper, behaviors that promote safety and behaviors that feel unsafe for them today.
Strategy #4: Refer to Seeking Safety: A Treatment Manual for PTSD and Substance Abuse (Najavits, 2002a). This menu-based manual covers an array of treatment topics, including the core concept of safety. Each topic consists of several segments, including preparing for the session, session format, session content, handouts, and guidelines.
Strategy #5: Encourage the development of a safety plan. Depending on the type of trauma, personal safety can be an issue; work with the client to develop a plan that will help him or her feel in control and prepared for the unexpected. If the trauma was a natural or human-caused disaster, encourage thinking about how family and friends will respond and connect in the event of another crisis. If sexual abuse or rape was the event, encourage thinking about future steps that could help make the client safer. There is a delicate balance between preparation and the realization that one cannot prepare for all possible traumatic events. Nonetheless, an action plan can help the client regain a sense of environmental balance.
A second aspect is safety in the environment. Trauma reactions can be triggered by sudden loud sounds (e.g., television at high volume, raised voices), tension between people, certain smells, or casual touches that are perceived as invasions of physical boundaries. The vulnerability of exposing one’s history in the treatment setting can manifest in the client as feeling physically vulnerable and unsafe in the treatment environment. Sudden or inadequately explained treatment transitions, such as moving from one level of treatment to another or changing counselors, can also evoke feelings of danger, abandonment, or instability. Early in treatment, trauma survivors generally value routine and predictability. The counselor should recognize these needs and respond appropriately by offering information in advance, providing nonshaming responses to a client’s reactions to stimuli in his or her environment, and helping the client build a daily structure that feels safe.
A third aspect of safety is preventing a recurrence of trauma. People with histories of trauma and substance abuse are more likely to engage in high-risk behaviors and to experience subsequent traumas. Early treatment should focus on helping clients stop using unsafe coping mechanisms, such as substance abuse, self-harm, and other self-destructive behaviors, and replacing them with safe and healthy coping strategies. Helping clients learn to protect themselves in reasonable ways is a positive goal of treatment.
Prevent Retraumatization
A key objective in TIC is to prevent retraumatization generated by intervention and treatment practices and policies. Unfortunately, treatment settings and clinicians can unintentionally create retraumatizing experiences (for a review of traumas that can occur when treating serious mental illness, see Frueh et al., 2005). For instance, compassionate inquiry into a client’s history can seem similar to the interest shown by a perpetrator many years before. Direct confrontation by counselors about behaviors related to substance abuse can be seen, by someone who has been repeatedly physically assaulted, as provocation building up to assault. Counselor and program efforts to help clients constrain destructive behaviors can be interpreted as efforts to control and dominate the individual. Intrusive shaming or insensitive behavior demonstrated by another client in the program can threaten a trauma survivor whose boundaries have been disregarded in the past—thus making the experience of treatment feel dangerous rather than safe. Some staff and agency issues that can result in retraumatization include:
-
Disrespectfully challenging reports of abuse or other traumatic events.
-
Discounting a client’s report of a traumatic event.
-
Using isolation.
-
Using physical restraints.
-
Allowing the abusive behavior of one client toward another to continue without intervention.
-
Labeling intense rage and other feelings as pathological.
-
Minimizing, discrediting, or ignoring client responses.
-
Disrupting counselor–client relationships by changing counselors’ schedules and assignments.
-
Obtaining urine specimens in a nonprivate and/or disrespectful manner.
-
Having clients undress in the presence of others.
-
Being insensitive to a client’s physical or emotional boundaries.
-
Inconsistently enforcing rules and allowing chaos in the treatment environment.
-
Applying rigid agency policies or rules without an opportunity for clients to question them.
-
Accepting agency dysfunction, including a lack of consistent, competent leadership.
Advice to Counselors: Strategies To Prevent Retraumatization
Strategy #1: Be sensitive to the needs of clients who have experienced trauma regarding behaviors in the treatment setting that might trigger memories of the trauma.
Strategy #2: Do not ignore clients’ symptoms and demands when clients with trauma histories act out in response to triggered trauma memories; doing so may replicate the original traumatic experience.
Strategy #3: Be mindful that efforts to control and contain a client’s behaviors in treatment can produce an abnormal reaction, particularly for trauma survivors for whom being trapped was part of the trauma experience.
Strategy #4: Listen for specific triggers that seem to be driving the client’s reaction. An important step in recovery is helping the client identify these cues and thereby reach a better understanding of reactions and behaviors.
Provide Psychoeducation
Trauma-informed education informs clients about traumatic stress and trauma-related symptoms and disorders as well as the related consequences of trauma exposure. It focuses on giving information to clients to help normalize presenting symptoms, to highlight potential short-term and long-term consequences of trauma and various paths to recovery, and to underscore the message that recovery is possible. Education frequently takes place prior to or immediately following an initial screening as a way to prepare clients for hearing results or to place the screening and subsequent assessment findings in proper context. Education in and of itself, however, does not necessarily constitute a stand-alone treatment; rather, it can be conceptualized as a first step and/or component of more comprehensive treatment. Nonetheless, education may be a prevention and intervention strategy for individuals who have histories of trauma without current consequences or symptoms and/or those who have reported a resolution of past trauma(s). For example, some clients may have significantly delayed onset of traumatic stress symptoms. In this scenario, earlier education can enhance recognition of symptoms and ease the path of seeking treatment.
Advice to Counselors: Strategies To Implement Psychoeducation
Strategy #1: Remember that this may be the client’s first experience with treatment. It’s easy to use program or clinical jargon when you’re around it every day, but most individuals who seek help are unfamiliar with clinical language, how the program works, and treatment objectives. Psychoeducation begins with understanding the client’s expectations and reasons for seeking help, followed by educating the client and other family members about the program. Remember that this is all new for them.
Strategy #2: After obtaining acknowledgment of a trauma history, provide an overview of common symptoms and consequences of traumatic stress, regardless of whether the client affirms having trauma-related symptoms. It is equally important to educate the client on resilience factors associated with recovery from trauma (Wessely et al., 2008). A trauma-informed perspective provides a message that trauma reactions are normal responses to an abnormal situation.
Strategy #3: Develop a resource box that provides an array of printed or multimedia educational materials that address the program, specific symptoms and tools to combat trauma-related symptoms, treatment options and therapy approaches, advantages of peer support, and steps in developing specific coping strategies.
Strategy #4: Develop a rotating educational group that matches services and client schedules to complement treatment. Remember that education can play a pivotal role in enhancing motivation, in normalizing experiences, and in creating a sense of safety as individuals move further into treatment. For some survivors, education can be a powerful intervention or prevention strategy.
Some clients do not recognize the link between their current difficulties and their trauma histories; education can help them understand the possible origin of their difficulties. Psychoeducation presents trauma-related symptoms that follow a trauma as normal reactions. By identifying the source of clients’ current difficulties and framing them as normal thoughts, emotions, and behaviors in response to trauma, many trauma survivors report a reduction in the intensity of the difficulties or symptoms. Often, a client will express relief that his or her reactions are normal. You may find the U.S. Department of Veterans Affairs (VA) National Center on PTSD’s educational handouts on traumatic stress reactions useful.
Psychoeducation goes beyond the identification of traumatic stress symptoms and/or learning about the psychological, cognitive, and physical impacts of trauma. Numerous curricula are available that use psychoeducation as a first-line or complementary approach to trauma-specific therapies to enhance coping strategies in key areas, including safety, emotional regulation, help-seeking, avoidant behavior, and so forth. An example is S.E.L.F., a trauma-informed psychoeducational group curriculum with educational components related to trauma recovery in the following areas: creating Safety, regulating Emotions, addressing Loss, and redefining the Future (Bloom, Foderaro, & Ryan, 2006).
Case Illustration: Linda
Linda served as an Army nurse in an evacuation hospital in Vietnam. She reported her postdeployment adjustment as difficult and isolating but denied any significant symptoms of traumatic stress throughout her life. Four years ago, Linda sought treatment for alcohol dependence; during the intake, she recalls denying trauma-related symptoms. “I distinctly remember the session,” she recounts. “The counselor first took my history but then gave information on typical symptoms and reactions to trauma. I thought, ‘Why do I need to hear this? I’ve survived the worst trauma in my life.’ I didn’t see the value of this information. Then 3 weeks ago, I began to have recurrent nightmares, the same graphic type I occasionally had when I was in Vietnam. Since then, I’ve been very anxious, reliving horrible scenes that I’d experienced as a nurse and postponing going to bed in fear of having the dreams again. I didn’t understand it. I am 70 years old, and the war happened a long time ago. Then I began putting it together. Recently, the emergency helicopter flight pattern and approach to the area’s hospital changed. I began hearing the helicopter periodically in my living room, and it reminded me of Vietnam. I knew then that I needed help; I couldn’t stop shaking. I felt as if I was losing control of my emotions. I remembered how the intake counselor took the time to explain common symptoms of trauma. That’s why I’m here today.”
“This might not sound like a big deal, but for many people relationships have become all about getting: telling your problem story and then getting help with it. There is little, if any, emphasis placed on giving back. That’s a big deal!!! Service relationships are like a one-way street and both people’s roles are clearly defined. But in ‘regular’ relationships in your community, people give and take all the time. No one is permanently on the taking side or the giving side. This exchange contributes to people feeling ok about being vulnerable (needing help) as well as confident about what they’re offering. For many of us, being the role of ‘getter’ all the time has shaken our confidence, making us feel like we have nothing worthwhile to contribute. Peer support breaks that all down. It gets complicated somewhat when one of us is paid, but modeling this kind of relationship in which both of us learn, offers us the real practice we need to feel like a ‘regular’ community member as opposed to an ‘integrated mental patient’.”
(Mead, 2008, p.7)
Offer Trauma-Informed Peer Support
Living with a history of trauma can be isolating and consuming. The experience of trauma can reinforce beliefs about being different, alone, and marred by the experience. At times, behavioral health treatment for trauma-related effects can inadvertently reinforce these beliefs. Simply engaging in treatment or receiving specialized services (although warranted) can further strengthen clients’ beliefs that there is something wrong with them. Formalized peer support can enhance the treatment experience. Treatment plus peer support can break the cycle of beliefs that reinforce traumatic stress (e.g., believing that one is permanently damaged; that nobody could understand; that no one should or could tolerate one’s story). Peer support provides opportunities to form mutual relationships; to learn how one’s history shapes perspectives of self, others, and the future; to move beyond trauma; and to mirror and learn alternate coping strategies. Peer support defines recovery as an interactive process, not as a definitive moment wherein someone fixes the “problem.”
Advice to Counselors: Strategies To Enhance Peer Support
Strategy #1: Provide education on what peer support is and is not. Roles and expectations of peer support can be confusing, so providing clarification in the beginning can be quite useful. It is important to provide initial education about peer support and the value of using this resource.
Strategy #2: Use an established peer support curriculum to guide the peer support process. For example, Intentional Peer Support: An Alternative Approach (Mead, 2008) is a workbook that highlights four main tasks for peer support: building connections, understanding one’s worldview, developing mutuality, and helping each other move toward set desires and goals. This curriculum provides extensive materials for peer support staff members as well as for the individuals seeking peer support.
Normalize Symptoms
Symptoms of trauma can become serious barriers to recovery from substance use and mental disorders, including trauma-related ones. Counselors should be aware of how trauma symptoms can present and how to respond to them when they do appear. A significant step in addressing symptoms is normalizing them. People with traumatic stress symptoms need to know that their symptoms are not unique and that their reactions are common to their experience(s). Often, normalizing symptoms gives considerable relief to clients who may have thought that their symptoms signified some pervasive, untreatable mental disorder.
Advice to Counselors: Strategies To Normalize Symptoms
Strategy #1: Provide psychoeducation on the common symptoms of traumatic stress.
Strategy #2: Research the client’s most prevalent symptoms specific to trauma, and then provide education to the client. For example, an individual who was conscious and trapped during or as a result of a traumatic event will more likely be hypervigilant about exits, plan escape routes even in safe environments, and have strong reactions to interpersonal and environmental situations that are perceived as having no options for avoidance or resolution (e.g., feeling stuck in a work environment where the boss is emotionally abusive).
Strategy #3: First, have the client list his or her symptoms. After each symptom, ask the client to list the negative and positive consequences of the symptom. Remember that symptoms serve a purpose, even if they may not appear to work well or work as well as they had in the past. Focus on how the symptoms have served the client in a positive way (see Case Illustration: Hector). This exercise can be difficult, because clients as well as counselors often don’t focus on the value of symptoms.
Case Illustration: Hector
Hector was referred to a halfway house specializing in co-occurring disorders after inpatient treatment for methamphetamine dependence and posttraumatic stress disorder (PTSD). In the halfway house, he continued to feel overwhelmed with the frequency and intensity of flashbacks. He often became frustrated, expressing anger and a sense of hopelessness, followed by emotional withdrawal from others in the house. Normalization strategy #3 was introduced in the session. During this exercise, he began to identify many negative aspects of flashbacks. He felt that he couldn’t control the occurrence of flashbacks even though he wanted to, and he realized that he often felt shame afterward. In the same exercise, he was also urged to identify positive aspects of flashbacks. Although this was difficult, he realized that flashbacks were clues about content that he needed to address in trauma-specific treatment. “I realized that a flashback, for me, was a billboard advertising what I needed to focus on in therapy.”
Identify and Manage Trauma-Related Triggers
Many clients who have traumatic stress are caught off guard with intrusive thoughts, feelings, sensations, or environmental cues of the trauma. This experience can be quite disconcerting, but often, the individual does not draw an immediate connection between the internal or external trigger and his or her reactions. At other times, the trigger is so potent that the individual is unable to discern the present trigger from the past trauma and begins to respond as if the trauma is reoccurring. Key steps in identifying triggers are to reflect back on the situation, surroundings, or sensations prior to the strong reaction. By doing so, you and your client may be able to determine the connections among these cues, the past trauma(s), and the client’s reaction. Once the cue is identified, discuss the ways in which it is connected to past trauma. For some cues, there will be an obvious and immediate connection (e.g., having someone say “I love you” in a significant relationship as an adult and connecting this to an abuser who said the same thing prior to a sexual assault). Other cues will not be as obvious. With practice, the client can begin to track back through what occurred immediately before an emotional, physical, or behavioral reaction and then examine how that experience reminds him or her of the past.
Advice to Counselors: Strategies To Identify and Manage Trauma-Related Triggers
Strategy #1: Use the Sorting the Past From the Present technique for cognitive realignment (Blackburn, 1995) to help separate the current situation from the past trauma. Identify one trigger at a time, and then discuss the following questions with the client:
-
When and where did you begin to notice a reaction?
-
How does this situation remind you of your past history or past trauma?
-
How are your reactions to the current situation similar to your past reactions to the trauma(s)?
-
How was this current situation different from the past trauma?
-
How did you react differently to the current situation than to the previous trauma?
-
How are you different today (e.g., factors such as age, abilities, strength, level of support)?
-
What choices can you make that are different from the past and that can help you address the current situation (trigger)?
After reviewing this exercise several times in counseling, put the questions on a card for the client to carry and use outside of treatment. Clients with substance use disorders can benefit from using the same questions (slightly reworded) to address relapse triggers.
Strategy #2: After the individual identifies the trigger and draws connections between the trigger and past trauma, work with him or her to establish responses and coping strategies to deal with triggers as they occur. Initially, the planned responses will not immediately occur after a trigger, but with practice, the planned responses will move closer to the time of the trigger. Some strategies include an acronym that reflects coping strategies (Exhibit 1.5-1), positive self-talk generated by cognitive–behavioral covert modeling exercises (rehearsal of coping statements), breathing retraining, and use of support systems (e.g., calling someone).
Strategy #3: Self-monitoring is any strategy that asks a client to observe and record the number of times something happens, to note the intensity of specific experiences, or to describe a specific behavioral, emotional, or cognitive phenomenon each time it occurs. For individuals with histories of trauma, triggers and flashbacks can be quite frightening, intense, and powerful. Even if the client has had just one or two triggers or flashbacks, he or she may perceive flashbacks as happening constantly. Often, it takes time to recover from these experiences. Using self-monitoring and asking the client to record each time a trigger occurs, along with describing the trigger and its intensity level (using a scale from 1–10), clients and counselors will gain an understanding of the type of triggers present and the level of distress that each one produces. Moreover, the client may begin to see that the triggers don’t actually happen all the time, even though they may seem to occur frequently.
Exhibit 1.5-1 The OBSERVATIONS Coping Strategy
-
Take a moment to just Observe what is happening. Pay attention to your body, your senses, and your environment.
-
Focus on your Breathing. Allow your feelings and sensations to wash over you. Breathe.
-
Name the Situation that initiated your response. In what way is this situation familiar to your past? How is it different?
-
Remember that Emotions come and go. They may be intense now, but later they will be less so. Name your feelings.
-
Recognize that this situation does not define you or your future. It does not dictate how things will be, nor is it a sign of things to come. Even if it is familiar, it is only one event.
-
Validate your experience. State, at least internally, what you are feeling, thinking, and experiencing.
-
Ask for help. You don’t have to do this alone. Seek support. Other people care for you. Let them!
-
This too shall pass. Remember: There are times that are good and times that are not so good. This hard time will pass.
-
I can handle this. Name your strengths. Your strengths have helped you survive.
-
Keep an Open mind. Look for and try out new solutions.
-
Name strategies that have worked before. Choose one and apply it to this situation.
-
Remember you have survived. You are a Survivor!
Draw Connections
Mental health and substance abuse treatment providers have historically underestimated the effects of trauma on their clients for many reasons. Some held a belief that substance abuse should be addressed before attending to any co-occurring conditions. Others did not have the knowledge and training to evaluate trauma issues or were uncomfortable or reluctant to discuss these sensitive issues with clients (Ouimette & Brown, 2003). Similarly, in other behavioral health settings, clinicians sometimes address trauma-related symptoms but do not have experience or training in the treatment of substance abuse.
Advice to Counselors: Strategies To Help Clients Draw Connections
Strategy #1: Writing about trauma can help clients gain awareness of their thoughts, feelings, and current experiences and can even improve physical health outcomes (Pennebaker, Kiecolt-Glaser, & Glaser, 1988; Smyth, Hockemeyer, & Tulloch, 2008). Although this tool may help some people draw connections between current experiences and past traumas, it should be used with caution; others may find that it brings up too much intense trauma material (especially among vulnerable trauma survivors with co-occuring substance abuse, psychosis, and current domestic violence). Journal writing is safest when you ask clients to write about present-day specific targets, such as logging their use of coping strategies or identifying strengths with examples. Writing about trauma can also be done via key questions or a workbook that provides questions centered upon trauma experiences and recovery.
Strategy #2: Encourage clients to explore the links among traumatic experiences and mental and substance use disorders. Recognition that a mental disorder or symptom developed after the trauma occurred can provide relief and hope that the symptoms may abate if the trauma is addressed. Ways to help clients connect substance use with trauma histories include (Najavits, 2002b; Najavits, Weiss, & Shaw, 1997):
-
Identifying how substances have helped “solve” trauma or PTSD symptoms in the short term (e.g., drinking to get to sleep).
-
Teaching clients how trauma, mental, and substance use disorders commonly co-occur so that they will not feel so alone and ashamed about these issues.
-
Discussing how substance abuse has impeded healing from trauma (e.g., by blocking feelings and memories).
-
Helping clients recognize trauma symptoms as triggers for relapse to substance use and mental distress.
-
Working on new coping skills to recover from trauma and substance abuse at the same time.
-
Recognizing how both trauma and substance abuse often occur in families through multiple generations.
So too, people who have histories of trauma will often be unaware of the connection between the traumas they’ve experienced and their traumatic stress reactions. They may notice depression, anger, or anxiety, or they may describe themselves as “going crazy” without being able to pinpoint a specific experience that produced the trauma symptoms. Even if clients recognize the events that precipitated their trauma symptoms, they may not understand how others with similar experiences can have different reactions. Thus, a treatment goal for trauma survivors is helping them gain awareness of the connections between their histories of trauma and subsequent consequences. Seeing the connections can improve clients’ ability to work on recovery in an integrated fashion.
Teach Balance
You and your clients need to walk a thin line when addressing trauma. Too much work focused on highly distressing content can turn a desensitization process into a session whereby the client dissociates, shuts down, or becomes emotionally overwhelmed. On the other hand, too little focus by the client or counselor can easily reinforce avoidance and confirm the client’s internal belief that it is too dangerous to deal with the aftermath of the trauma. Several trauma-specific theories offer guidelines on acceptable levels of distress associated with the traumatic content that the therapy addresses. For example, some traditional desensitization processes start at a very low level of subjective distress, gradually working up through a hierarchy of trauma memories and experiences until those experiences produce minimal reactions when paired with some coping strategy, such as relaxation training. Other desensitization processes start at a higher level of intensity to provide more rapid extinction of traumatic associations and to decrease the risk of avoidance—a behavior that reinforces traumatic stress.
The Subjective Units of Distress Scale (SUDS) uses a 0–10 rating scale, with 0 representing content that causes no or minimal distress and 10 representing content that is exceptionally distressing and overwhelming. (Wolpe & Abrams, 1991)
Working with trauma is a delicate balancing act between the development and/or use of coping strategies and the need to process the traumatic experiences. Individuals will choose different paths to recovery; it’s a myth that every traumatic experience needs to be expressed and every story told. For some individuals, the use of coping skills, support, and spirituality are enough to recover. Regardless of theoretical beliefs, counselors must teach coping strategies as soon as possible. Retraumatization is a risk whenever clients are exposed to their traumatic histories without sufficient tools, supports, and safety to manage emotional, behavioral, and physical reactions.
Advice to Counselors: Strategy To Teach Balance
Strategy #1: Teach and use the SUDS in counseling. This scale can be useful from the outset as a barometer for the client and counselor to measure the level of distress during and outside of sessions. It provides a common language for the client and counselor, and it can also be used to guide the intensity of sessions. SUDS can tangibly show a client’s progress in managing experiences. Without a scale, it is more difficult to grasp that a distressing symptom or circumstance is becoming less and less severe without some repeated measure.
Build Resilience
Survivors are resilient! Often, counselors and clients who are trauma survivors focus on the negative consequences of trauma while failing to recognize the perseverance and attributes that have helped them survive. It is natural to focus on what’s not working rather than what has worked. To promote growth after trauma and establish a strengths-based approach, focus on building on clients’ resilience. Current resilience theories claim that building or reinforcing resilience prevents further development of trauma-related symptoms and disorders. The following Advice to Counselors box is adapted from the American Psychological Association’s 2003 statement on resilience.
Address Sleep Disturbances
Sleep disturbances are one of the most enduring symptoms of traumatic stress and are a particularly common outcome of severe and prolonged trauma. Sleep disturbances increase one’s risk of developing traumatic stress; they significantly alter physical and psychological processes, thus causing problems in daytime functioning (e.g., fatigue, cognitive difficulty, excessive daytime sleepiness). People with sleep disturbances have worse general health and quality of life. The cardiovascular and immune systems, among others, may be affected as well. Sleep disturbances can worsen traumatic stress symptoms and interfere with healing by impeding the brain’s ability to process and consolidate traumatic memories (Caldwell & Redeker, 2005).
Sleep disturbances vary among trauma survivors and can include decreased ability to stay asleep, frequent awakenings, early morning unintentional awakening, trouble falling asleep, poor quality of sleep, and disordered breathing during sleep (Caldwell & Redeker, 2005). Most traumatic stress literature focuses on nightmares, insomnia, and frequent awakenings. These disturbances are connected to two main symptoms of traumatic stress: hyperarousal (which causes difficulty in falling and remaining asleep) and reexperiencing the trauma (e.g., through recurrent nightmares).
Advice to Counselors: Strategies To Build Resilience
Strategy #1: Help clients reestablish personal and social connections. Access community and cultural resources; reconnect the person to healing resources such as mutual-help groups and spiritual supports in the community.
Strategy #2: Encourage the client to take action. Recovery requires activity. Actively taking care of one’s own needs early in treatment can evolve into assisting others later on, such as by volunteering at a community organization or helping military families.
Strategy #3: Encourage stability and predictability in the daily routine. Traumatic stress reactions can be debilitating. Keeping a daily routine of sleep, eating, work, errands, household chores, and hobbies can help the client see that life continues. Like exercise, daily living skills take time to take hold as the client learns to live through symptoms.
Strategy #4: Nurture a positive view of personal, social, and cultural resources. Help clients recall ways in which they successfully handled hardships in the past, such as the loss of a loved one, a divorce, or a major illness. Revisit how those crises were addressed.
Strategy #5: Help clients gain perspective. All things pass, even when facing very painful events. Foster a long-term outlook; help clients consider stress and suffering in a spiritual context.
Strategy #6: Help maintain a hopeful outlook. An optimistic outlook enables visions of good things in life and can keep people going even in the hardest times. There are positive aspects to everyone’s life. Taking time to identify and appreciate these enhances the client’s outlook and helps him or her persevere.
Strategy #7: Encourage participation in peer support, 12-Step, and other mutual-help programs.
Advice to Counselors: Strategies To Conduct a Sleep Intervention
Strategy #1: Conduct a sleep history assessment focused first on the client’s perception of his or her sleep patterns. Assess whether there is difficulty initiating or staying asleep, a history of frequent or early morning awakenings, physically restless sleep, sleepwalking, bedtime aversion, and/or disruptive physical and emotional states upon awakening (e.g., confusion, agitation, feeling unrested). Also determine total sleep time, pattern of nightmares, and use of medications, alcohol, and/or caffeine (see Moul, Hall, Pikonis, & Buysse, 2004, for a review of self-report measures).
Strategy #2: Use a sleep hygiene measure to determine the presence of habits that typically interfere with sleep (e.g., falling asleep while watching television). The National Sleep Foundation Web site (http://www.sleepfoundation.org) provides simple steps for promoting good sleep hygiene..
Strategy #3: Provide education on sleep hygiene practices. Introduce clients to the idea that practicing good sleep hygiene is one step toward gaining control over their sleep disturbances.
Strategy #4: Reassess sleep patterns and history during the course of treatment. Sleep patterns often reflect current client status. For example, clients who are struggling are more likely to have disturbed sleep patterns; sleep disturbances significantly influence clients’ mental health status.
Strategy #5: Use interventions such as nightmare rehearsals to target recurrent nightmares. There are numerous examples of imagery-based nightmare rehearsals. Clients may be instructed to rehearse repetitively the recurrent nightmare a few hours before bedtime. In this instruction, the client either rehearses the entire nightmare with someone or visualizes the nightmare several times to gain control over the material and become desensitized to the content. Other strategies involve imagining a change in the outcome of the nightmare (e.g., asking the client to picture getting assistance from others, even though his or her original nightmare reflects dealing with the experience alone).
Other sleep disturbances trauma survivors report include sleep avoidance or resistance to sleep (see Case Illustration: Selena), panic awakenings, and restless or unwanted body movements (e.g., hitting your spouse unintentionally in bed while asleep; Habukawa, Maeda, & Uchimura, 2010).
Case Illustration: Selena
Selena initially sought treatment for ongoing depression (dysthymia). During treatment, she identified being sexually assaulted while attending a party at college. At times, she blames herself for the incident because she didn’t insist that she and her girlfriends stay together during the party and on the way back to their dorm afterward. Selena reported that she only had two drinks that night: “I could never manage more than two drinks before I wanted to just sleep, so I never drank much socially.” She was assaulted by someone she barely knew but considered a “big brother” in the brother fraternity of her sorority. “I needed a ride home. During that ride, it happened,” she said. For years thereafter, Selena reported mild bouts of depression that began lasting longer and increasing in number. She also reported nightmares and chronic difficulty in falling asleep. In therapy, she noted avoiding her bed until she’s exhausted, saying, “I don’t like going to sleep; I know what’s going to happen.” She describes fear of sleeping due to nightmares. “It’s become a habit at night. I get very involved in playing computer games to lose track of time. I also leave the television on through the night because then I don’t sleep as soundly and have fewer nightmares. But I’m always exhausted.”
Build Trust
Some traumatic experiences result from trusting others (e.g., interpersonal trauma). In other cases, trust was violated during or after the traumatic experience, as in cases when help was late to arrive on the scene of a natural disaster. This lack of trust can leave individuals alienated, socially isolated, and terrified of developing relationships. Some feel that the trauma makes them different from others who haven’t had similar experiences. Sometimes, a client’s trust issues arise from a lack of trust in self—for instance, a lack of trust in one’s perceptions, judgment, or memories. People who have also experienced severe mental or substance use disorders may have difficulty trusting others because, during the course of their illness, they felt alienated or discriminated against for behaviors and emotions generated by or associated with the disorders.
Some client groups (e.g., gay, lesbian, and bisexual clients; people from diverse cultures; those with serious mental illness) evidence significant mistrust because their trust has been repeatedly violated in the past. Traumatic experiences then compound this mistrust. Mistrust can come from various sources, is usually unstated, and, if left unaddressed, can impede treatment. For example, some clients leave treatment early or do not engage in potentially beneficial treatments. Others avoid issues of trust and commitment by leaving treatment when those issues begin to arise.
Establishing a safe, trusting relationship is paramount to healing—yet this takes time in the counseling process. Counselors and other behavioral health professionals need to be consistent throughout the course of treatment; this includes maintaining consistency in the parameters set for availability, attendance, and level of empathy. Trust is built on behavior shown inside and outside of treatment; you should immediately address any behavior that may even slightly injure the relationship (e.g., being 5 minutes late for an appointment, not responding to a phone message in a timely manner, being distracted in a session).
Advice to Counselors: Strategies To Build Trust
Strategy #1: Clients can benefit from a support or counseling group composed of other trauma survivors. By comparing themselves with others in the group, they can be inspired by those who are further along in the recovery process and helpful to those who are not faring as well as they are. These groups also motivate clients to trust others by experiencing acceptance and empathy.
Strategy #2: Use conflicts that arise in the program as opportunities. Successful negotiation of a conflict between the client and the counselor is a major milestone (van der Kolk, McFarlane, & Van der Hart, 1996). Helping clients understand that conflicts are healthy and inevitable in relationships (and that they can be resolved while retaining the dignity and respect of all involved) is a key lesson for those whose relationship conflicts have been beset by violence, bitterness, and humiliation.
Strategy #3: Prepare clients for staff changes, vacations, or other separations. Some clients may feel rejected or abandoned if a counselor goes on vacation or is absent due to illness, especially during a period of vulnerability or intense work. A phone call to the client during an unexpected absence can reinforce the importance of the relationship and the client’s trust. You can use these opportunities in treatment to help the client understand that separation is part of relationships; work with the client to view separation in a new light.
Strategy #4: Honor the client–counselor relationship, and treat it as significant and mutual. You can support the development of trust by establishing clear boundaries, being dependable, working with the client to define explicit treatment goals and methods, and demonstrating respect for the client’s difficulty in trusting you and the therapeutic setting.
Support Empowerment
Strong feelings of powerlessness can arise in trauma survivors seeking to regain some control of their lives. Whether a person has survived a single trauma or chronic trauma, the survivor can feel crushed by the weight of powerlessness. Mental illness and substance abuse, too, can be disempowering; clients may feel that they’ve lost control over their daily lives, over a behavior such as drug use, or over powerful emotions such as fear, sadness, or anger. Empowerment means helping clients feel greater power and control over their lives, as long as such control is within safe and healthy bounds. A key facet of empowerment is to help clients build on their strengths. Empowerment is more than helping clients discover what they “should” do; it is also helping them take the steps they feel ready to take.
Case Illustration: Abby
Abby, a 30-year-old, nervous-looking woman, is brought by her parents to a community mental health clinic near their home in rural Indiana. During the intake process, the counselor learns that Abby is an Army Reservist who returned from 12 months of combat duty 3 years ago. The war experience changed her in many ways. Her deployment pulled her away from veterinary school as well as the strong emotional support of family, friends, and fellow classmates. She got along with her unit in Iraq and had no disciplinary problems. While there, she served as a truck driver in the Sunni Triangle. Her convoy was attacked often by small arms fire and was once struck by an improvised explosive device. Although Abby sustained only minor injuries, two of her close friends were killed. With each successive convoy, her level of fear and foreboding grew, but she continued performing as a driver.
Since returning to the United States, she has mostly stayed at home and has not returned to school, although she is helping out on the farm with various chores. Abby has isolated herself from both family members and lifelong friends, saying she doesn’t think others can understand what she went through and that she prefers being alone. She reports to her parents and the counselor that she is vaguely afraid to be in cars and feels most comfortable in her room or working alone, doing routine tasks, at home. Abby also says that she now understands how fragile life can be.
She has admitted to her parents that she drinks alcohol on a regular basis, something she did not do before her deployment, and that on occasion, she has experienced blackouts. Abby feels she needs a drink before talking with strangers or joining in groups of friends or family. She confided to her father that she isolates herself so that she can drink without having to explain her drinking to others.
The counselor recognizes Abby’s general sense of lacking internal control and feeling powerless over what will happen to her in the future. He adopts a motivational interviewing style to establish rapport and a working alliance with Abby. During sessions, the counselor asks Abby to elaborate on her strengths; he reinforces strengths that involve taking action in life, positive self-statements, and comments that deal with future plans. He also introduces Abby to an Iraq War veteran who came home quite discouraged about putting his life together but has done well getting reintegrated. The counselor urges Abby go to the local VA center so that she can meet and bond with other recently returned veterans. He also encourages Abby to attend Alcoholics Anonymous meetings, emphasizing that she won’t be pressured to talk or interact with others more than she chooses to.
The counselor continues to see Abby every week and begins using cognitive–behavioral techniques to help her examine some of her irrational fears about not being able to direct her life. He asks Abby to keep a daily diary of activities related to achieving her goals of getting back to school and reestablishing a social network. In each session, Abby reviews her progress using the diary as a memory aid, and the counselor reinforces these positive efforts. After 4 months of treatment, Abby re-enrolls in college and is feeling optimistic about her ability to achieve her career plans.
Advice to Counselors: Strategies To Support Empowerment
Strategy #1: Offer clients information about treatment; help them make informed choices. Placing appropriate control for treatment choices in the hands of clients improves their chances of success.
Strategy #2: Give clients the chance to collaborate in the development of their initial treatment plan, in the evaluation of treatment progress, and in treatment plan updates. Incorporate client input into treatment case consultations and subsequent feedback.
Strategy #3: Encourage clients to assume an active role in how the delivery of treatment services occurs. An essential avenue is regularly scheduled and structured client feedback on program and clinical services (e.g., feedback surveys). Some of the most effective initiatives to reinforce client empowerment are the development of peer support services and the involvement of former clients in parts of the organizational structure, such as the advisory board or other board roles.
Strategy #4: Establish a sense of self-efficacy in clients; their belief in their own ability to carry out a specific task successfully—is key. You can help clients come to believe in the possibility of change and in the hope of alternative approaches to achieving change. Supporting clients in accepting increasing responsibility for choosing and carrying out personal change can facilitate their return to empowerment (Miller & Rollnick, 2002).
Acknowledge Grief and Bereavement
The experience of loss is common after traumas, whether the loss is psychological (e.g., no longer feeling safe) or physical (e.g., death of a loved one, destruction of community, physical impairment). Loss can cause public displays of grief, but it is more often a private experience. Grieving processes can be emotionally overwhelming and can lead to increased substance use and other impulsive behaviors as a way to manage grief and other feelings associated with the loss. Even for people who experienced trauma years prior to treatment, grief is still a common psychological issue. Delayed or absent reactions of acute grief can cause exhaustion, lack of strength, gastrointestinal symptoms, and avoidance of emotions.
Risk factors of chronic bereavement (grief lasting more than 6 months) can include:
-
Perceived lack of social support.
-
Concurrent crises or stressors (including reactivation of PTSD symptoms).
-
High levels of ambivalence about the loss.
-
An extremely dependent relationship prior to the loss.
-
Loved one’s death resulting from disaster: unexpected, untimely, sudden, and shocking (New South Wales Institute of Psychiatry & Centre for Mental Health, 2000).
Advice to Counselors: Strategies To Acknowledge and Address Grief
Strategy #1: Help the client grieve by being present, by normalizing the grief, and by assessing social supports and resources.
Strategy #2: When the client begins to discuss or express grief, focus on having him or her voice the losses he or she experienced due to trauma. Remember to clarify that losses include internal experiences, not just physical losses.
Strategy #3: For a client who has difficulty connecting feelings to experiences, assign a feelings journal in which he or she can log and name each feeling he or she experiences, rate the feeling’s intensity numerically, and describe the situation during which the feeling occurred. The client may choose to share the journal in an individual or group session.
Strategy #4: Note that some clients benefit from developing a ritual or ceremony to honor their losses, whereas others prefer offering time or resources to an association that represents the loss.
Monitor and Facilitate Stability
Stability refers to an ongoing psychological and physical state whereby one is not overwhelmed by disruptive internal or external stimuli (Briere & Scott, 2006b). It’s common for individuals to have an increase in symptoms, distress, or impairment when dealing with the impact of their trauma or talking about specific aspects of their trauma. There is a thin line that the client and counselor need to negotiate and then walk when addressing trauma. Too much work focused on highly distressing content can turn a desensitization process into a session that causes the client to dissociate, shut down, or become emotionally overwhelmed. On the other hand, too little focus by the client or counselor can easily reinforce avoidance and confirm the client’s internal belief that it is too dangerous to deal with the aftermath of the trauma.
Advice to Counselors: Strategies To Monitor and Facilitate Stability
Strategy #1: If destabilization occurs during the intake process or treatment, stop exploring the material that triggered the reaction, offer emotional support, and demonstrate ways for the client to self-soothe.
Strategy #2: Seek consultation from supervisors and/or colleagues (e.g., to explore whether a new case conceptualization is needed at this point).
Strategy #3: Refer the client for a further assessment to determine whether a referral is necessary for trauma-specific therapy or a higher level of care, or use of multiple levels of care (e.g., intensive outpatient care, partial hospitalization, residential treatment).
Strategy #4: Focus on coping skills and encourage participation in a peer support program.
Strategy #5: When a client becomes agitated and distressed, carefully explore with the client what is causing this state. When such feelings arise because of current threats in the client’s life or environment, it is dangerous to halt or soothe away responses that act as warning signals (Pope & Brown, 1996). When a client is in a situation involving domestic violence, lives in a dangerous neighborhood, or has run out of money for food, he or she requires direct and concrete assistance rather than simple emotional support.
Source: Briere & Scott, 2006b.
Managing Destabilization
When a client becomes destabilized during a session, you can respond in the following manner: “Let’s slow down and focus on helping you be and feel safe. What can we do to allow you to take care of yourself at this moment? Then, when you feel ready, we can decide what to focus on next.”
Clients should have some psychological stability to engage in trauma-related work. An important distinction can be made between a normative increase in symptoms (e.g., the typical up-and-down course of traumatic stress reactions or substance abuse) and destabilization (dangerous, significant decrease in functioning). Signs of destabilization include (Green Cross Academy of Traumatology, 2007; Najavits, 2002b):
-
Increased substance use or other unsafe behavior (e.g., self-harm).
-
Increased psychiatric symptoms (e.g., depression, agitation, anxiety, withdrawal, anger).
-
Increased symptoms of trauma (e.g., severe dissociation).
-
Helplessness or hopelessness expressed verbally or behaviorally.
-
Difficulty following through on commitments (e.g., commitment to attend treatment sessions).
-
Isolation.
-
Notable decline in daily activities (e.g., self-care, hygiene, care of children or pets, going to work).
Treatment Issues
The treatment environment itself can significantly affect how clients experience traumatic stress and how the client responds to treatment. Some specific issues related to working with trauma survivors in a clinical setting are discussed in the following sections.
Client Engagement
A lack of engagement in treatment is the client’s inability to make progress toward treatment goals, deal with important topics in treatment, or complete treatment. Clients who have histories of trauma will express ambivalence about treatment similarly to others, except that clients who have traumatic stress can feel more “stuck” and perceive themselves as having fewer options. In addition, clients may be avoiding engagement in treatment because it is one step closer to addressing their trauma. You should attend to the client’s motivation to change, implement strategies that address ambivalence toward treatment, and use approaches that help clients overcome avoidant behavior.
Advice to Counselors: Strategies To Foster Engagement
Strategy #1: According to Mahalik (2001), the standard method of handling clients’ lack of engagement is exploring it with them, clarifying the situation through discussion with them, reinterpreting (e.g., from “can’t” to “won’t” to “willing”), and working through the situation toward progress.
Strategy #2: To improve engagement into treatment, try motivational interviewing and enhancement techniques. For additional information on such techniques, see TIP 35, Enhancing Motivation for Change in Substance Abuse Treatment (Center for Substance Abuse Treatment [CSAT], 1999b).
Pacing and Timing
Although your training or role as a counselor may prohibit you from providing trauma-specific services, you must still be prepared for the fact that clients are not as focused on when or where it is most appropriate to address trauma—they want relief, and most lay and professional people have been taught that the only path to recovery is disclosure. Some clients are reluctant to talk about anything associated with their histories of trauma. Other clients immediately want to delve into the memories of their trauma without developing a safe environment. The need to gain any relief for the traumatic stress pushes some individuals to disclose too quickly, without having the necessary support and coping skills to manage the intensity of their memories. Clients who enter treatment and immediately disclose past trauma often don’t return because the initial encounter was so intense or because they experienced considerable emotional distress for several days afterward and/or in anticipation of the next session.
Proper pacing of sessions, disclosure, and intensity is paramount. Clients who immediately disclose without proper safety nets are actually retraumatizing themselves by reliving the experience without adequate support—often placing themselves in the same circumstances that occurred during the actual traumas they experienced. Although you should not adamantly direct clients not to talk about what happened, it is important to discuss with the clients, even if you have to interrupt them empathically and respectfully, the potential consequences of disclosing too soon and too fast. Ask whether they have done this before, and then inquire about the outcome. Reinforce with clients that trauma heals when there are support, trust, and skills in place to manage the memories of the traumatic experiences. Ideally, disclosure begins after these elements are secured, but realistically, it is a balancing act for both the counselor and client as to when and how much should be addressed in any given session. Remember not to inadvertently give a message that it is too dangerous to talk about trauma; instead, reinforce the importance of addressing trauma without further retraumatization.
Advice to Counselors: Strategies To Establish Appropriate Pacing and Timing
Strategy #1: Frequently discuss and request feedback from clients about pacing and timing. Moving too quickly into discussion of the trauma can increase the risk of dissociation, overactivation of memories, and feeling overwhelmed.
Strategy #2: Use the SUDS as a barometer of intensity to determine the level of work.
Strategy #3: Slowly increase the speed of interventions and continually adjust the intensity of interventions; move in and out of very intense work, or use strategies that decrease the intensity when necessary. One approach that typically decreases the intensity of traumatic memories is to ask the individual to imagine that he or she is seeing the scene through a window or on a television screen. This helps decrease intensity and the risk of dissociation. It provides an opportunity for the client to view the trauma from a different perspective and a strategy to use outside of treatment to shift from reliving the trauma to observing it from a neutral position.
Strategy #4: Monitor clients to ensure that treatment does not overwhelm their internal capacities, retraumatize them, or result in excessive avoidance; make sure therapy occurs in the “therapeutic window” (Briere & Scott, 2006b).
Strategy #5: Be alert to signs that discussions of trauma, including screening, assessment, and intake processes, are going too fast. Mild to moderate signs are:
-
Missing counseling appointments after discussions of important material.
-
Periods of silence.
-
Dissociation.
-
Misunderstanding what are usually understandable concepts.
-
Redirecting the focus of the discussion when certain issues arise.
Strategy #6: Observe the client’s emotional state. Slow down; seek consultation if the client exhibits:
-
Persistent resistance to addressing trauma symptoms.
-
Repetitive flashbacks.
-
Increase in dissociation.
-
Regression.
-
Difficulty in daily functioning (e.g., trouble maintaining everyday self-care tasks).
-
Substance use relapses.
-
Self-harm or suicidal thoughts/behaviors (e.g., talking about suicide).
Strategy #7: Use caution and avoid (Briere, 1996b, p. 115):
-
Encouraging clients to describe traumatic material in detail before they can deal with the consequences of disclosure.
-
Using overly stressful interventions (e.g., intensive role-plays, group confrontation, guided imagery).
-
Confrontations or interpretations that are too challenging given the client’s current functioning.
-
Demanding that the client work harder and stop resisting.
Source: Strategies 1–6: Green Cross Academy of Traumatology, 2001. Adapted with permission.
Length of Treatment
Many factors influence decisions regarding the length of treatment for a given client. Severity of addiction, type of substance abused, type of trauma, age at which the trauma occurred, level of social support, and the existence of mental disorders all influence length of treatment. External factors, such as transportation and childcare, caps on insurance coverage, and limitations in professional resources, can also affect length of treatment. In general, longer treatment experiences should be expected for clients who have histories of multiple or early traumas, meet diagnostic criteria for multiple Axis I or Axis II diagnoses, and/or require intensive case management. Most of the empirically studied and/or manual-based models described in the next chapter are short-term models (e.g., lasting several months); however, ongoing care is indicated for clients with more complex co-occurring trauma disorders.
Traumatic Memories
One of the most controversial issues in the trauma field is the phenomenon of “recovered memories” or “traumatic amnesia” (Brewin, 2007). Practitioners working with traumatized individuals are particularly concerned about the possibility of new memories of the traumatic event emerging during the course of therapy and the possibility of these memories being induced by the clinician. Scientific reviews indicate that people can experience amnesia and delayed recall for some memories of a wide variety of traumas, including military combat and prisoner of war experiences, natural disasters and accidents, childhood sexual abuse, and political torture (Bowman & Mertz, 1996; Brewin, 2007; Karon & Widener, 1997; McNally, 2005). In some cases, the survivor will not remember some of what happened, and the counselor may need to help the client face the prospect of never knowing all there is to know about the past and accept moving on with what is known.
Legal Issues
Legal issues can emerge during treatment. A client, for instance, could seek to prosecute a perpetrator of trauma (e.g., for domestic violence) or to sue for damages sustained in an accident or natural disaster. The counselor’s role is not to provide legal advice, but rather, to offer support during the process and, if needed, refer the client to appropriate legal help (see Advice to Counselors box on p. 131). A legal matter can dominate the treatment atmosphere for its duration. Some clients have difficulty making progress in treatment until most or all legal matters are resolved and no longer act as ongoing stressors.
Advice to Counselors: Strategies To Manage Traumatic Memories
Strategy #1: Most people who were sexually abused as children remember all or part of what happened to them, although they do not necessarily fully understand or disclose it. Do not assume that the role of the clinician is to investigate, corroborate, or substantiate allegations or memories of abuse (American Psychiatric Association [APA], 2000b).
Strategy #2: Be aware that forgotten memories of childhood abuse can be remembered years later. Clinicians should maintain an empathic, nonjudgmental, neutral stance toward reported memories of sexual abuse or other trauma. Avoid prejudging the cause of the client’s difficulties or the veracity of the client’s reports. A counselor’s prior belief that physical or sexual abuse, or other factors, are or are not the cause of the client’s problems can interfere with appropriate assessment and treatment (APA, 2000b).
Strategy #3: Focus on assisting clients in coming to their own conclusions about the accuracy of their memories or in adapting to uncertainty regarding what actually occurred. The therapeutic goal is to help clients understand the impact of the memories or abuse experiences on their lives and to reduce their detrimental consequences in the present and future (APA, 2000b).
Strategy #4: Some clients have concerns about whether or not a certain traumatic event did or did not happen. In such circumstances, educate clients about traumatic memories, including the fact that memories aren’t always exact representations of past events; subsequent events and emotions can have the effect of altering the original memory. Inform clients that it is not always possible to determine whether an event occurred but that treatment can still be effective in alleviating distress.
Strategy #5: There is evidence that suggestibility can be enhanced and pseudomemories can develop in some individuals when hypnosis is used as a memory enhancement or retrieval strategy. Hypnosis and guided imagery techniques can enhance relaxation and teach self-soothing strategies with some clients; however, use of these techniques is not recommended in the active exploration of memories of abuse (Academy of Traumatology, 2007).
Strategy #6: When clients are highly distressed by intrusive flashbacks of delayed memories, help them move through the distress. Teach coping strategies and techniques on how to tolerate strong affect and distress (e.g., mindfulness practices).
Memories of Trauma
Points for counselors to remember are:
-
Some people are not able to completely remember past events, particularly events that occurred during high-stress and destabilizing moments.
-
In addition to exploring the memories themselves, it can be beneficial to explore how a memory of an event helps the client understand his or her feeling, thinking, and behaving in the present.
-
Persistently trying to recall all the details of a traumatic event can impair focus on the present.
Forgiveness
Clients may have all sorts of reactions to what has happened to them. They may feel grateful for the help they received, joy at having survived, and dedication to their recovery. At the other extreme, they may have fantasies of revenge, a loss of belief that the world is a good place, and feelings of rage at what has happened. They may hold a wide variety of beliefs associated with these feelings.
One issue that comes up frequently among counselors is whether to encourage clients to forgive. The issue of forgiveness is a very delicate one. It is key to allow survivors their feelings, even if they conflict with the counselor’s own responses. Some may choose to forgive the perpetrator, whereas others may remain angry or seek justice through the courts and other legal means. Early in recovery from trauma, it is best to direct clients toward focusing on stabilization and a return to normal functioning; suggest that, if possible, they delay major decisions about forgiveness until they have a clearer mind for making decisions (Herman, 1997). Even in later stages of recovery, it’s not essential for the client to forgive in order to recover. Forgiveness is a personal choice independent of recovery. Respect clients’ personal beliefs and meanings; don’t push clients to forgive or impose your own beliefs about forgiveness onto clients.
In the long-term healing process, typically months or years after the trauma(s), forgiveness may become part of the discussion for some people and some communities. For example, in South Africa, years after the bitter and bloody apartheid conflicts, a Truth and Reconciliation Commission was established by the Government. Public hearings created dialog and aired what had been experienced as a means, ultimately, to promote forgiveness and community healing. By addressing very difficult topics in public, all could potentially benefit from the discourse. Similarly, a parental survivor of the Oklahoma City bombing was, at first, bitter about his daughter’s early, unfair, and untimely death. Today, he gives talks around the world about the abolition of the death penalty. He sat with convicted bomber Timothy McVeigh’s father while the man’s son was executed in Indiana at a Federal prison several years after the bombing. For this man, forgiveness and acceptance helped him attain personal peace. Other trauma survivors may choose never to forgive what happened, and this, too, is a legitimate response.
Advice to Counselors: Strategies To Manage Legal Proceedings
Strategy #1: If you’re aware of legal proceedings, you can play a key role in helping your client prepare emotionally for their impact, such as what it might be like to describe the trauma to a judge or jury, or how to cope with seeing the perpetrator in court. When helping a client prepare, however, be careful not to provide legal advice.
Strategy #2: Help clients separate a successful legal outcome from a successful treatment outcome. If clients connect these two outcomes, difficulties can arise. For example, a client may discontinue treatment after his or her assailant is sentenced to serve prison time, believing that the symptoms will abate without intervention.
Strategy #3: If clients express interest in initiating a civil or criminal suit, encourage them to consider the ways in which they are and are not prepared for this, including their own mental states, capacity for resilience, and inevitable loss of confidentiality (Pope & Brown, 1996). Inform clients coping with legal issues that involvement in the legal process can be retraumatizing.
Strategy #4: Emphasize, for trauma survivors who are involved in legal proceedings against an assailant, that “not guilty” is a legal finding—it is based on the degree of available evidence and is not a claim that certain events in question did not occur. They should also receive, from an attorney or other qualified individual, information on:
-
The nature of the legal process as it pertains to the clients’ specific cases.
-
The estimated duration and cost of legal services, if applicable.
-
What to expect during police investigations.
-
Court procedures.
-
Full information on all possible outcomes.
-
What to expect during cross-examination.
Strategy #5: Counselors can be called on to assist with a legal case involving trauma. The court may require you to provide treatment records, to write a letter summarizing your client’s progress, or to testify at a trial. Always seek supervisory and legal advice in such situations and discuss with the client the possible repercussions that this might have for the therapeutic relationship. As a general rule, it is best practice to avoid dual roles or relationships.
Culturally and Gender Responsive Services
Culture is the lens through which reality is interpreted. Without an understanding of culture, it is difficult to gauge how individuals organize, interpret, and resolve their traumas. The challenge is to define how culture affects individuals who have been traumatized.
Increased knowledge of PTSD (Wilson & Tang, 2007), mental illness, and substance use disorders and recovery (Westermeyer, 2004) requires behavioral health practitioners to consider the complicated interactions between culture, personality, mental illness, and substance abuse in adapting treatment protocols. This section offers some general guidelines for working with members of cultures other than one’s own. Treatment for traumatic stress, mental illness, substance use disorders, and co-occurring trauma-related symptoms is more effective if it is culturally responsive.
The U.S. Department of Health and Human Services (2003) has defined the term “cultural competence” as follows:
Cultural competence is a set of values, behaviors, attitudes, and practices within a system, organization, program, or among individuals that enables people to work effectively across cultures. It refers to the ability to honor and respect the beliefs, language, interpersonal styles, and behaviors of individuals and families receiving services, as well as staff who are providing such services. Cultural competence is a dynamic, ongoing, developmental process that requires a long-term commitment and is achieved over time (p. 12).
Cultural competence is a process that begins with an awareness of one’s own culture and beliefs and includes an understanding of how those beliefs affect one’s attitudes toward people of other cultures. It is rooted in respect, validation, and openness toward someone whose social and cultural background is different from one’s own. For a thorough review of cultural competence, see the planned TIP, Improving Cultural Competence (Substance Abuse and Mental Health Services Administration [SAMHSA], planned c).
Cultural Competence
Cultural competence includes a counselor’s knowledge of:
-
Whether the client is a survivor of cultural trauma (e.g., genocide, war, government oppression, torture, terrorism).
-
How to use cultural brokers (i.e., authorities within the culture who can help interpret cultural patterns and serve as liaisons to those outside the culture).
-
How trauma is viewed by an individual’s sociocultural support network.
-
How to differentiate PTSD, trauma-related symptoms, and other mental disorders in the culture.
For more specific information on cultural competence in trauma therapy, see Brown (2008).
In some cultures, an individual’s needs take precedence over group needs (Hui & Triandis, 1986), and problems are seen as deriving from the self. In other cultures, however, complex family, kin, and community systems take precedence over individual needs. Considerable heterogeneity exists within and across most ethnic subcultures and across lines of gender, class, age, and political groups (CSAT, 1999b). Subcultures abound in every culture, such as gangs; populations that are homeless or use substances; orphaned or disenfranchised people; religious, ethnic, and sexual minorities; indigenous people; and refugee and immigrant populations. Some subcultures have more in common with similar subcultures in other countries than with their own cultures (e.g., nonheterosexual populations).
Trauma and substance abuse can themselves be a basis for affiliation with a subculture. De Girolamo (1993) reports that “disaster subcultures” exist within many cultures. These cultures of victimization, like all subcultures, have unique worldviews, codes of conduct, and perceptions of the larger society. In a disaster subculture, people are, to some extent, inured to disaster and heedless of warnings of impending disaster. For example, riverbank erosion in Bangladesh displaces thousands of people each year, yet few believe that it is a serious problem or that the displacement will be permanent (Hutton, 2000). Israelis who have lived with unpredictable violence for many years behave differently in public areas and have adapted to different norms than people who don’t commonly experience violence (Young, 2001).
Many people identify with more than one subculture. Some identify with a particular culture or subculture, but not with all of its values. Individual identities are typically a mosaic of factors, including developmental achievements, life experiences, behavioral health histories, traumatic experiences, and alcohol and illicit drug use; levels of acculturation and/or assimilation vary from one individual to the next as well.
Importance of the trauma aftermath
Counselors working in the immediate aftermath of trauma—whether individual, group, or community in nature—face many challenges. For example, survivors may be forced to adjust without access to other health services, employment, support, or insurance. In these instances, counselors must often work with individuals and communities coping with the trauma while struggling daily to meet basic needs. Research suggests that reestablishing ties to family, community, culture, and spiritual systems can not only be vital to the individual, but can also influence the impact of the trauma upon future generations. For example, Baker and Gippenreiter (1998) studied the descendants of people victimized by Joseph Stalin’s purge. They found that families who were able to maintain a sense of connection and continuity with grandparents affected by the purge experienced fewer negative effects than did those who were emotionally or physically severed from their grandparents. The researchers also found that whether the grandparents survived was less important than the connection the grandchildren managed to keep to their past. Ties to family and community can also have an adverse effect, especially if the family or community downplays the trauma or blames the victim. Counselors need to have a full understanding of available support before advocating a particular approach.
Treatment strategies
Many traditional healing ways have been damaged, forgotten, or lost—yet much wisdom remains. Drawing on the best traditional and contemporary approaches to human distress and defining culturally competent curricula regarding identity and healing (Huriwai, 2002; Wilson & Tang, 2007) both require respect and appreciation for the many ways in which various people characterize and resolve trauma and how they use addictive substances to bear the burdens of human distress.
Community-Based Treatment for Native American Historical Trauma
Key beliefs in community healing:
-
Clients carry childhood pain that has led to adult dysfunction.
-
Childhood pain must be confronted, confessed, and addressed, if relief is to be obtained.
-
Cathartic expression is the initial step in the healing journey toward a lifelong pursuit of introspection and self-improvement.
-
The healing journey entails reclamation of indigenous heritage, identity, spirituality, and practices to remedy the pathogenic effects of colonization and other sources of historical trauma.
Source: Gone, 2009.
It is not yet known how well existing PTSD treatments work for individuals who identify primarily with cultures other than mainstream American culture. It is possible that such treatments do work for clients of other cultures, though some cultural adaptation and translation may be required. For example, some PTSD treatments that have been used with subculture groups without adaptation other than language translation and that appear to be effective across cultures include eye movement desensitization and reprocessing (Bleich, Gelkopf, & Solomon, 2003) and Seeking Safety (Daouest et al., 2012).
Gender
Gender differences exist in traumatic stress, mental disorders, and substance use disorders. For example, women have higher rates of PTSD, whereas men have higher rates of substance abuse (Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Stewart, Ouimette, & Brown, 2002; Tolin & Foa, 2006). The types of interpersonal trauma experienced by men and by women are often different. A number of studies (Kimerling, Ouimette, & Weitlauf, 2007) indicate that men experience more combat and crime victimization and women experience more physical and/or sexual assault—implying that men’s traumas often occur in public, whereas the traumatization of women is more likely to take place in a private setting, such as a home. Men’s abusers are more often strangers. Those who abuse women, on the other hand, are more often in a relationship with them. Women (and girls) often are told, “I love you,” during the same time period when the abuse occurs. However, women now serve in the military and thus are increasingly subject to some of the same traumas as men and also to military sexual trauma, which is much more common for women to experience. Similarly, men can be subject to domestic violence or sexual abuse.
Working With Clients From Diverse Cultures: Trauma and Substance Abuse
-
In socially appropriate ways, educate clients, their loved ones, and possibly members of their extended community about the relationship between substance abuse and PTSD, how substance abuse is often used to cope with trauma, and what treatment entails.
-
Make serious efforts to connect clients to supportive and understanding people (preferably within culturally identified groups).
-
Help clients understand that many who have not experienced trauma or do not have substance use disorders will not understand the psychological, spiritual, and interpersonal insights that they have gained during their recovery processes.
In treatment, gender considerations are relevant in a variety of ways, including, but not limited to, the role and impact of societal gender stereotypes upon assessment processes, treatment initiation, and engagement of services (e.g., peer support systems); the selection and implementation of gender-specific and gender-responsive approaches for both men and women at each level of intervention; and the best selection of trauma-related interventions that account for gender-specific differences related to traumatic stress. For an extensive review and discussion of gender-specific and gender-responsive care for traumatic stress and substance use, see the TIP 51, Substance Abuse Treatment: Addressing the Specific Needs of Women (CSAT, 2009d), and TIP 56, Addressing the Specific Behavioral Health Needs of Men (SAMHSA, 2013a).
Beyond the complexities of gender considerations, one must also consider whether clients should be given the choice of working with a male or a female counselor. Some clients who have been traumatized have no preference, particularly if their trauma wasn’t associated with gender (e.g., a natural disaster, act of terrorism, fire, serious accident). If gender did play a role in trauma (e.g., childhood sexual abuse), clients can have strong fears of working with a counselor who is the same gender as the perpetrator. Many women who experienced sexual abuse (whose perpetrators are typically men) feel uncomfortable being treated by men because of the intense emotions that can be evoked (e.g., anger, fear). Men who experienced sexual abuse (whose perpetrators are also typically men) can feel uncomfortable for the same reasons, or they may feel shame when talking to men due to feelings evoked about masculinity, homosexuality, and so forth. However, not all clients with trauma histories prefer female therapists.
Discuss with clients the possible risks (e.g., initial emotional discomfort) and benefits of being treated by a woman or man (e.g., developing a therapeutic relationship with a man might challenge a client’s belief that all men are dangerous), and, if possible, let them then choose the gender of their counselor. Tell them that if they experience initial emotional discomfort, and the discomfort does not decrease, they can switch to a counselor of the opposite gender. For group therapy that focuses on trauma, similar considerations apply. Generally, gender-specific groups are recommended when possible, but mixed-gender groups also work. Gender also comes into play in substance abuse treatment. Research and clinical observation indicate that significant gender differences occur in many facets of substance abuse and its treatment. For example, men and women experience different physical repercussions of substance use (e.g., women have more health problems), different trajectories (e.g., women become addicted more quickly), and different treatment considerations (e.g., traditional substance abuse treatment was designed for men).
Sexual orientation
Lesbian, gay, bisexual, and transgender (LGBT) clients face specific issues in behavioral health treatment settings, including histories of abuse and discrimination relating to sexual orientation, homophobia in treatment on the part of counselors or other clients, potential difficulty addressing traumatic experiences related to their sexuality or sexual orientation, and often, a significant lack of trust toward others. LGBT people sometimes think that others can’t understand them and their specific needs and thus are reluctant to engage in treatment programs in which the clientele is predominantly heterosexual. Some clients react with judgment, anger, or embarrassment when an LGBT client attempts to describe sexual trauma relating to homosexual behavior, making it even harder for LGBT clients to describe their experiences.
Often, individual counseling can address issues the LGBT client isn’t comfortable discussing in group treatment. “Providing one-on-one services may decrease the difficulty of mixing heterosexual and LGBT clients in treatment groups and decrease the likelihood that hetero-sexism or homophobia will become an issue” (CSAT, 2001, p. 56). For more on treating LGBT individuals, see A Provider’s Introduction to Substance Abuse Treatment for Lesbian, Gay, Bisexual, and Transgender Individuals (CSAT, 2001).
Making Referrals to Trauma-Specific Services
Many people who experience trauma do not exhibit persistent traumatic stress symptoms. In fact, people do recover on their own. So how do you determine who is at higher risk for developing more persistent symptoms of traumatic stress, trauma-related disorders, and traumatic stress disorders? One main factor is the severity of symptoms at the time of screening and assessment. Other factors, beyond trauma characteristics and pretrauma individual characteristics, to consider in making referrals include (Ehlers & Clark, 2003):
-
Cognitive appraisals that are excessively negative regarding trauma sequelae, including consequences, changes after the event(s), responses of other people to the trauma, and symptoms.
-
Acknowledgment of intrusive memories.
-
Engagement in behaviors that reinforce or prevent resolution of trauma, including avoidance, dissociation, and substance use.
-
History of physical consequences of trauma (e.g., chronic pain, disfigurement, health problems).
-
Experiences of more traumas or stressful life events after the prior trauma.
-
Identification of co-occurring mood disorders or serious mental illness.
The next chapter provides an overview of trauma-specific services to complement this chapter and to provide trauma-informed counselors with a general knowledge of trauma-specific treatment approaches.

