1.9: Parapharyngeal Space
- Page ID
- 17603
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
ACCESS TO THE PARAPHARYNGEAL SPACE
Johan Fagan
The parapharyngeal space (PPS) extends from the skull base above, to the hyoid bone below, and contains fat, the carotid artery, internal jugular vein, and the lower cranial nerves and sympathetic nerve. Surgical resection of tumors of the PPS requires a good understanding of the anatomy, likely pathology (if not known), and surgical approaches.
Relevant Anatomy
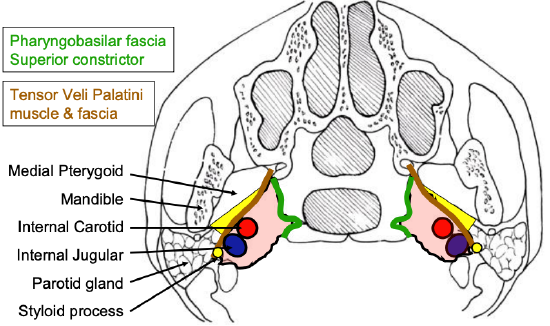
Figure 1: Schematic axial view of prestyloid (yellow) and poststyloid (pink) parapharyngeal spaces
The PPS extends as an inverted pyramid from the base of the skull superiorly, to the hyoid bone inferiorly. Figure 1 illustrates an axial view of the prestyloid (yellow) and poststyloid components of the PPS, separated by the styloid process, tensor veli palatini muscle and fascia stretching between (brown). The poststyloid space contains the internal carotid artery and the internal jugular vein, as well as the lower cranial nerves IX -XII, and the sympathetic trunk. It is confined medially by the pharyngobasilar fascia above, and the superior constrictor muscle of the pharynx.
Prestyloid PPS
Patients typically present with a mass in the lateral oropharynx, displacing the tonsil medially (Figure 2). The prestyloid PPS is bordered anterolaterally by the medial pterygoid muscle, and posterolaterally by the deep lobe of the parotid gland (Figures 1, 3). It extends from the hyoid bone inferiorly, to the skull base superiorly and contains mainly fat

Figure 2: Typical presentation of a prestyloid PPS mass
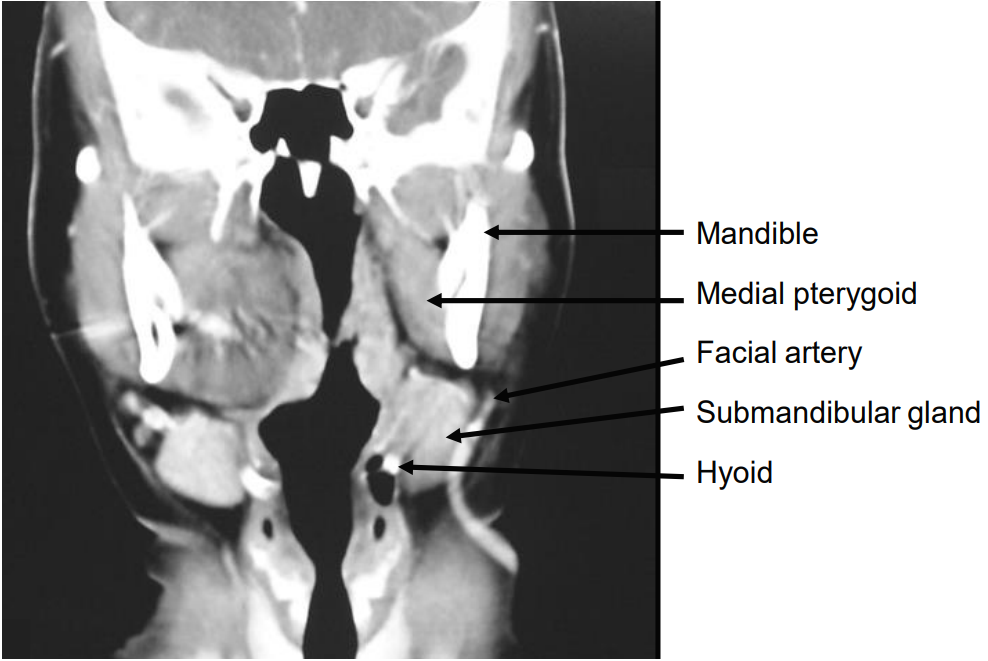
Figure 3: Anatomical relations of prestyloid PPS and contralateral pleomorphic adenoma, to medial pterygoid, submandibular salivary gland, and hyoid bone
Prestyloid tumors displace the PPS fat anteromedially (Figures 4, 5).
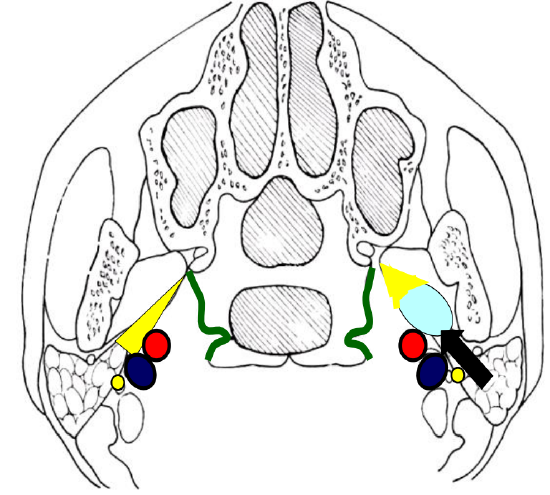
Figure 4: Direction of displacement of fat as seen on CT or MRI with prestyloid PPS mass (light blue)
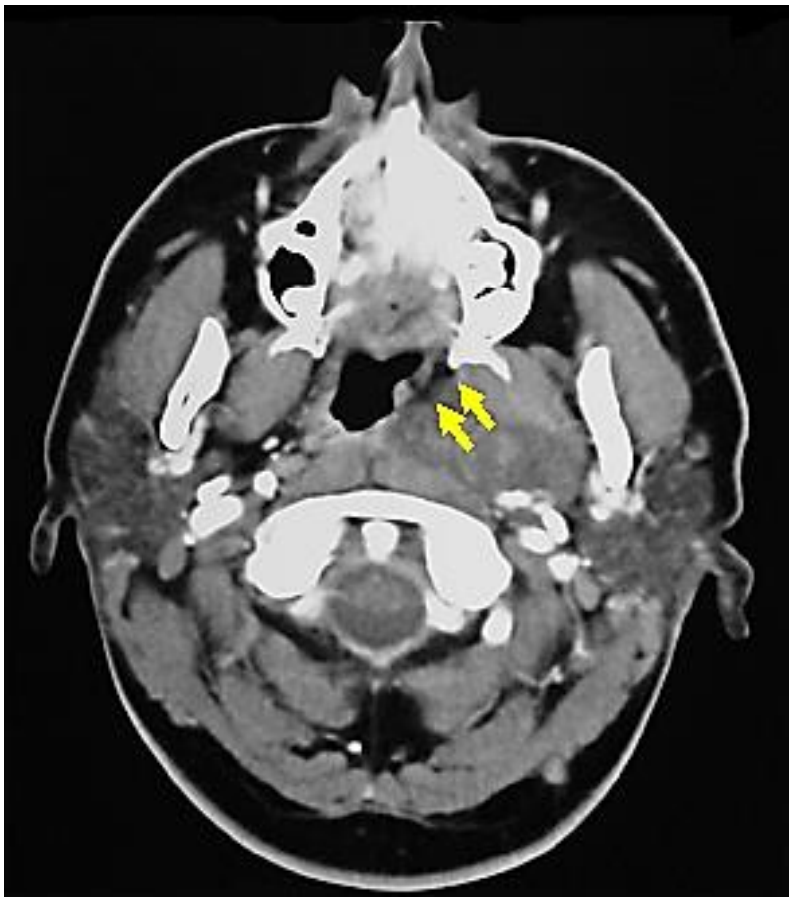
Figure 5: Pleomorphic adenoma of prestyloid PPS displacing fat anteromedially
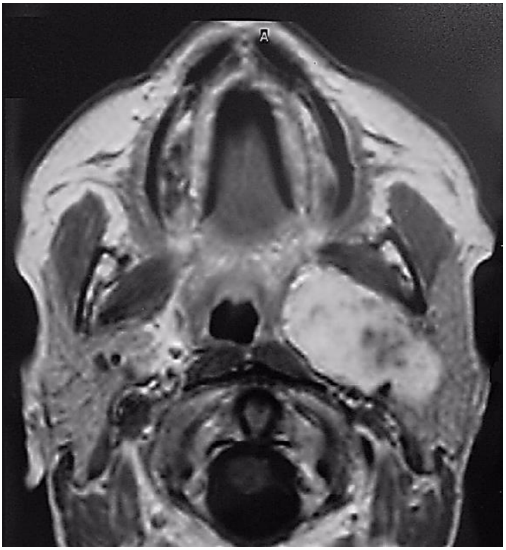
Figure 6: Dumbbell-type deep lobe parotid pleomorphic adenoma extension through stylomandibular tunnel into prestyloid PPS
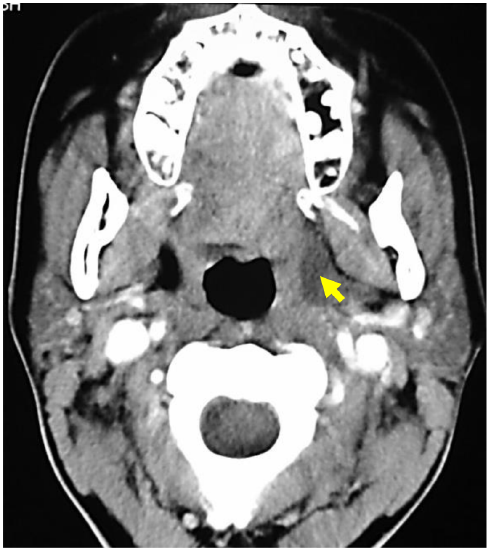
Figure 7: Ranula tracking along prestyloid PPS
Examples of masses commonly encountered in the prestyloid PPS include pleomorphic adenoma (Figures 3, 5), medial extension of a deep lobe parotid tumor (Figure 6) and a ranula that has tracked into the PPS (Figure 7).
Poststyloid PPS
Patients typically present with a mass extending into the upper lateral neck in the lateral oro- or nasopharynx, or with dysfunction of cranial nerves IX-XII, or Horner’s syndrome. The poststyloid PPS is confined medially by the pharyngobasilar fascia above, and the superior constrictor muscle of the pharynx. It contains the internal carotid artery and the internal jugular vein, as well as the lower cranial nerves IX -XII, and the sympathetic trunk. Unlike prestyloid masses, poststyloid tumors typically displace the PPS fat anterolaterally (Figures 8, 9).
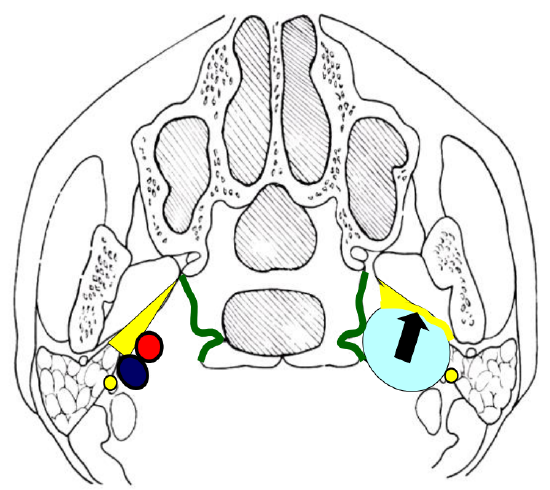
Figure 8: Direction of displacement of fat as seen on CT or MRI with poststyloid mass (light blue)
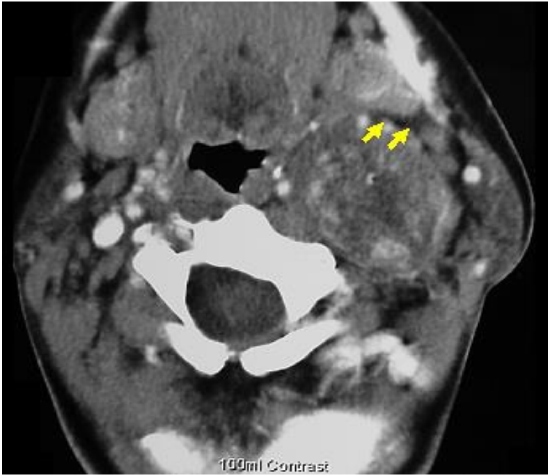
Figure 9: CT scan of poststyloid vagal schwannoma demonstrating direction of displacement of fat and medial displacement of carotid vessels
The most commonly encountered masses include carotid body tumors, or other paragangliomas e.g. of the vagus nerve and sympathetic trunk, and schwannomas (Figures 9, 10).
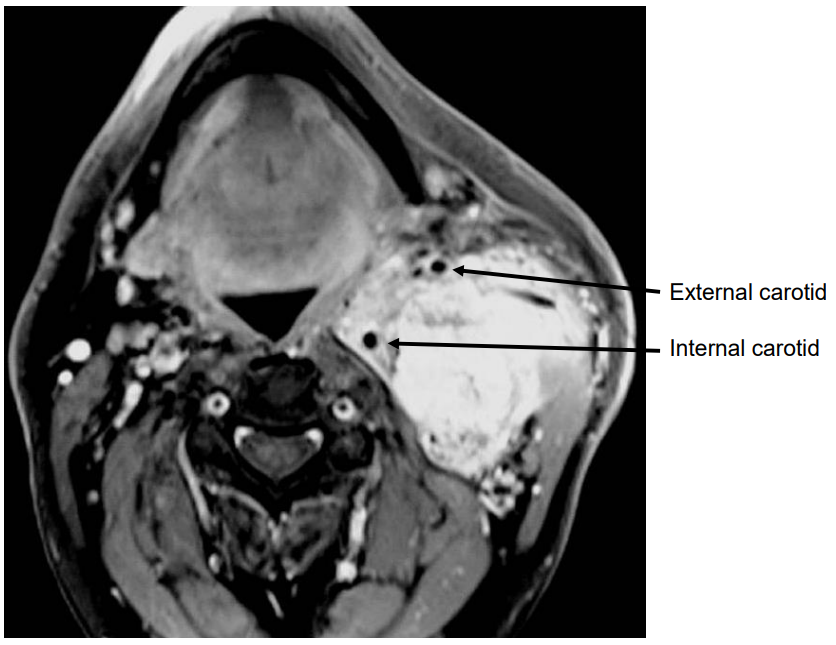
Figure 10: Carotid body tumor in poststyloid PPS, splaying the internal and external carotid arteries
Key Diagnostic Information
One should determine the following before embarking on surgery:
- Benign / malignant: This is generally determined by FNAC. The needle biopsy may be done transcervically or transorally. One should not be concerned about puncturing the internal carotid artery with a small needle
- Vascularity: A paraganglioma may be suspected on CT or MRI and confirmed angiographically. Vascular tumors may require preoperative embolisation and proximal vascular control, or one may elect to treat it with radiation
- Prestyloid / poststyloid: This is determined clinically and radiologically with CT / MRI as indicated previously. This information permits one to narrow down the differential diagnosis, to plan the best surgical approach, and to counsel preoperatively about possible sequelae
- Is a prestyloid mass originating from the parotid gland? This information might determine the surgical approach e.g. transcervical +/- total parotidectomy. It may be difficult to determine even radiologically whether a prestyloid pleomorphic adenoma simply represents ectopic salivary tissue, or is extending from the deep lobe of the parotid gland
- Internal & external carotid arteries: Particularly with poststyloid masses, knowledge of the position of the arteries is important in order to direct the surgery (Figure 10)
Surgical Approaches
Figure 11 presents a schematic summary of the surgical approaches to the PPS.
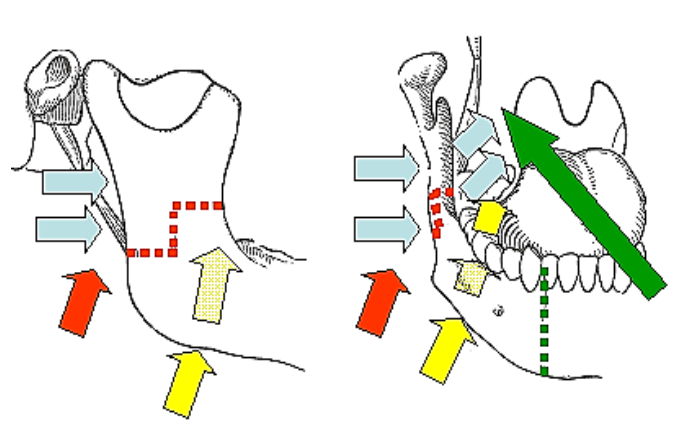
Figure 11: Approaches to PPS: transoral + mandibulotomy (green); transcervical submandibular (yellow), transparotid (blue), and transcervical + mandibulotomy (red)
Prestyloid surgical approaches
Masses in the prestyloid space are mostly benign, well defined, surrounded by fat, and unlike tumors of the poststyloid space, are generally not tethered to structures such as major nerves and vessels. They can therefore generally be removed by careful blunt dissection along the tumor capsule, avoiding tumor rupture (especially with pleomorphic adenomas that may seed). The tumors are situated anywhere between the hyoid bone and the skull base, but generally do not extend above the level of the hard palate or pterygoid plates and are situated on the medial aspect of the medial pterygoid muscle. They are readily accessed via a transcervical submandibular approach. Only rarely a transoral approach + mandibulotomy required. A large tumor arising from the deep lobe of the parotid may require a combined transcervical and transparotid approach.
Transcervical submandibular approach to prestyloid tumors
A horizontal skin crease incision is made at the level of the hyoid bone. The submandibular salivary gland (SSG) and digastric muscle are identified. The anterior facial vein is ligated and divided. The capsule of the SSG is incised. The SSG is mobilized in a subcapsular plane to protect the marginal mandibular nerve. The facial artery is identified posteroinferior to the gland where it emerges from behind the posterior belly of the digastric muscle (Figure 12).
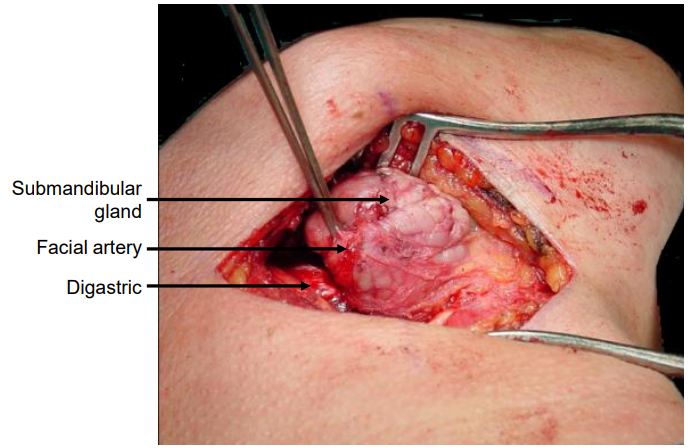
Figure 12: Exposure of left submandibular gland, digastric muscle and facial artery
The facial artery is then ligated and divided above the posterior belly of digastric. The submandibular gland is mobilized with gentle finger dissection in a posterior to anterior direction leaving the thin fascial layer over the ranine veins and the hypoglossal nerve intact (Figure 12). Additional mobility of the SSG may be achieved (if required) by dividing the facial artery and anterior facial vein above the SSG.
By retracting the posterior belly of digastric posteriorly, the mandible superiorly, and the submandibular gland anteriorly the surgeon can pass a finger /instrument directly into the prestyloid PPS (Figures 13, 14, 15).
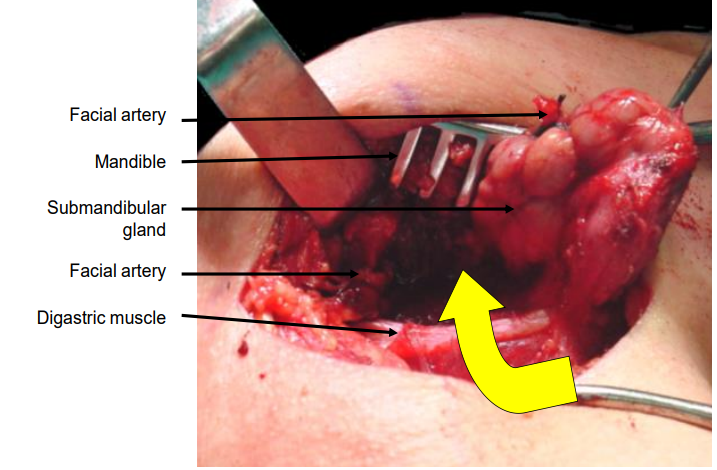
Figure 13: Displacement of submandibular gland for transcervical submandibular access to prestyloid PPS
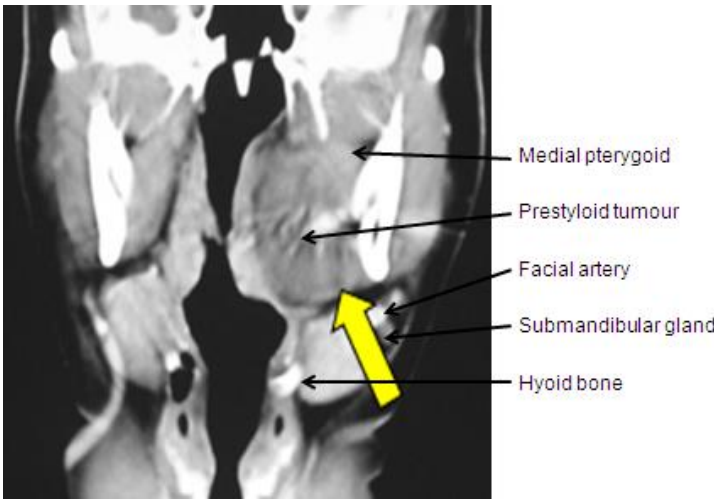
Figure 14: Access to prestyloid PPS mass via transcervical submandibular approach

Figure 15: Delivery of prestyloid PPS pleomorphic adenoma via transcervical submandibular approach
Transoral approach to prestyloid tumors
This approach is essentially the same as an extended tonsillectomy and may include a midline or paramedian mandibulotomy for additional access (Figures 11, 16). A disadvantage is that the neck is not opened, and the vessels not exposed in the event of injury to the major vessels requiring proximal vascular control.
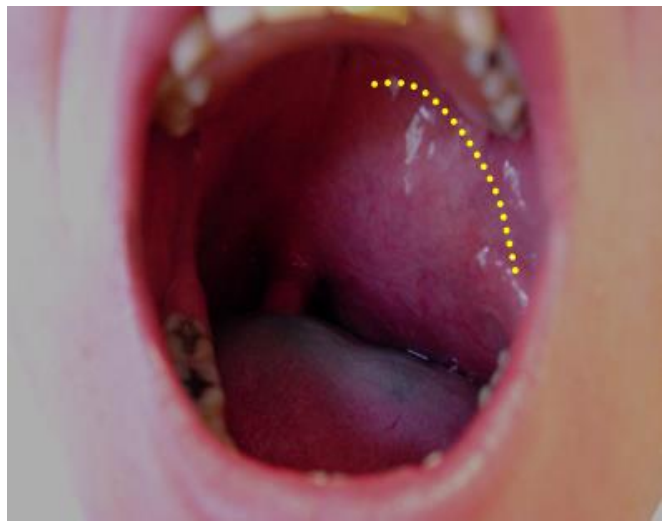
Figure 16: Transoral approach to access a prestyloid PPS mass
Combined transcervical submandibular and transparotid approaches to prestyloid tumors
Even large prestyloid tumors e.g. arising from the deep lobe of the parotid gland (Figure 17) may be resected via a combination of transparotid (see description below) and transcervical approaches.
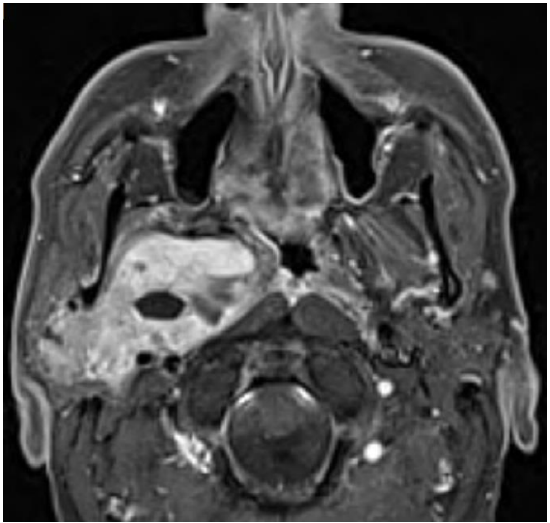
Figure 17: Pleomorphic adenoma arising from deep lobe of parotid extending into PPS resected by combined transcervical submandibular and transparotid approach
Poststyloid PPS surgical approaches
The principal challenges relating to resecting poststyloid masses are avoiding injury to the internal carotid artery, internal jugular vein and the lower cranial and sympathetic nerves. Access is restricted by the vertical ramus of the mandible, the parotid gland, the facial nerve and the styloid process with its muscular and ligamentous attachments.
Masses in the poststyloid space are mostly benign but unlike tumors of the prestyloid space, are generally tethered to/arise from major nerves and vessels. Resection requires good exposure of the mass and the major vessels and nerves via transcervical and/or transparotid approaches. Rarely a mandibulotomy of the vertical ramus of the mandible is required for additional exposure. Patients should be cautioned about the sequelae of vascular and lower cranial nerve injury, as well sympathetic trunk injury causing Horner’s and “1st Bite” syndromes. Preoperative embolisation of paragangliomas reduces intraoperative bleeding.
Transcervical approach to the poststyloid PPS (Figures 11, 18)
The transcervical approach is suitable for tumors extending up to about the level of the styloid process, such as smaller carotid body and glomus vagale tumors, as well as lower lying schwannomas. The upper neck is exposed via a transverse skin crease incision, the X, XI, and XII nerves are identified, as are the carotid bifurcation and the internal jugular vein. The mass is then removed using sharp dissection. The posterior belly of digastric is either retracted superiorly or divided to provide access deep to the parotid gland (Figure 18).
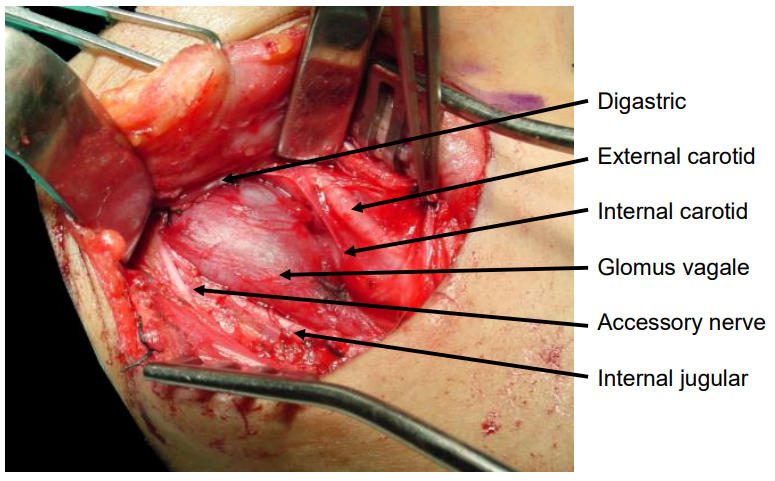
Figure 18: Transcervical resection of glomus vagale
Transparotid approach to the poststyloid PPS (Figures 11, 19, 20, 21, 22)
The transparotid approach is required for masses situated closer to the skull base. The superficial lobe of the parotid gland is elevated off the facial nerve, the nerve is freed from the deep lobe, and the deep parotid lobe is resected. This exposes the styloid process. Immediately medial to the styloid are the contents of the poststyloid PPS. Access can be further improved by excising the styloid process with a bone nibbler and retracting the mandible anteriorly (taking care to avoid excessive tension on the facial nerve), and inferiorly by dividing the posterior belly of the digastric.
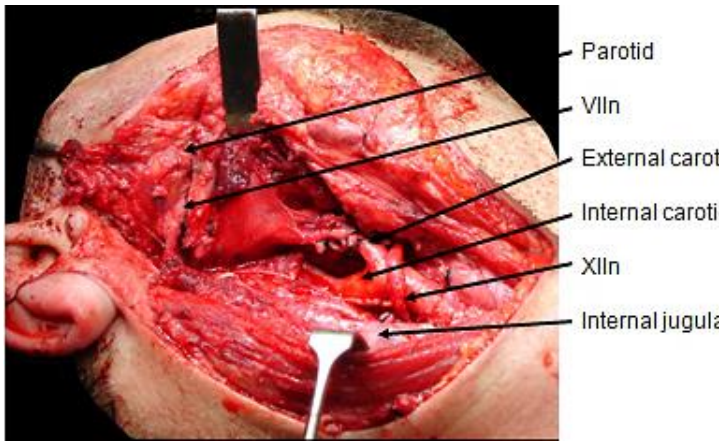
Figure 19: Operative field following resection of carotid body tumor shown in Figure 10
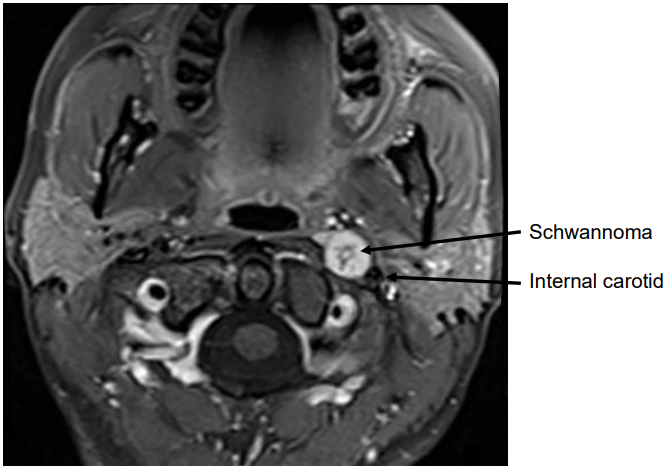
Figure 20: Schwannoma of poststyloid PPS located medial to internal carotid artery
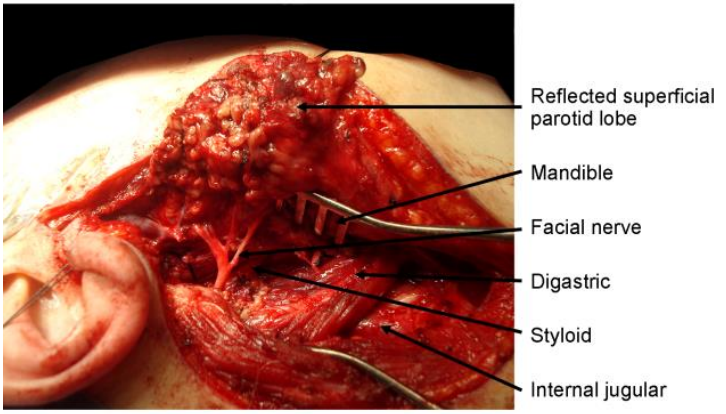
Figure 21: Transparotid access to poststyloid PPS in Figure 20
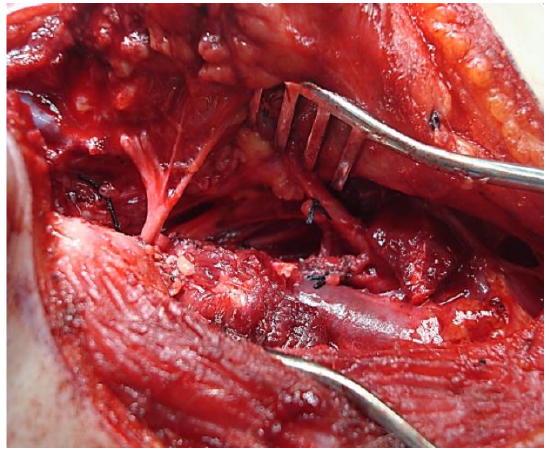
Figure 22: Additional access to poststyloid PPS in Figures 15 & 16 by transection of digastric muscle
Suggested reading
Kundiona I, Fagan JJ. Consequences and complications of surgery for tumors of the pre- versus poststyloid parapharyngeal spaces in 41 patients (our experience). Clin Otolaryngol. 2017 Aug;42(4):886-8
Author & Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za

The Open Access Atlas of Otolaryngology, Head & Neck Operative Surgery by Johan Fagan (Editor) johannes.fagan@uct.ac.za is licensed under a Creative Commons Attribution - Non-Commercial 3.0 Unported License