1.14: Surgical Closure Technique Tracheoesophageal Fistulae
- Page ID
- 17624
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
SURGICAL CLOSURE TECHNIQUE OF TRACHEOESOPHAGEAL FISTULAE (TOF)
Zenon Yeung, Johan Fagan
Tracheoesophageal fistula (TOF) speech is the optimal method for postlaryngectomy speech rehabilitation (Figures 1-3).
Advantages include:
- No external device required
- Doesn’t rely on a battery
- More natural, intelligible voice
- Uses patient’s tidal volume ~500mL as energy, and therefore allows the patient to speak louder with a more sustained voice without any pauses
However, problems do arise from time-to-time with the TOF and tracheoesophageal voice prosthesis1,2
- Enlarging fistula around prosthesis causing leakage of saliva and food and aspiration pneumonia (Figure 4)
- Leakage of saliva and food through the prosthesis
- Granulations around the prosthesis
- Failure of tracheoesophageal speech due to pharyngoesophageal segment spasm
- Fungal colonization of the prosthesis causing it to leak
- Dislodgement and aspiration of the prosthesis into the tracheobronchial tree
- Obstructed swallowing secondary to the prosthesis
- Failure of tracheoesophageal speech because of lack of motivation and cost of the prostheses
When the fistula enlarges with leakage of saliva and food around the prosthesis, or a decision is made to discontinue fistula speech and the TOF is no required, the TOF needs to be allowed to close or be closed.
Risk factors for an enlarging TOF include3
- Local infection
- Erosion by a feeding tube
- Ventilatory cuff injury
- Tracheal or esophageal malignancy
- Caustic or foreign body ingestion
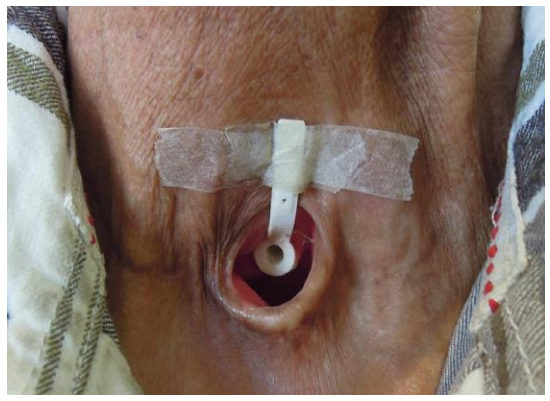
Figure 1: Voice prosthesis in situ

Figure 2: Occluding tracheostomy for voicing
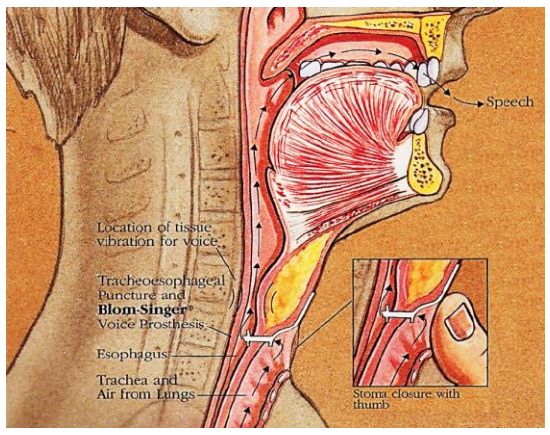
Figure 3: Mechanism of fistula speech (Adapted from Current Status of Voice Restoration Following Total Laryngectomy)
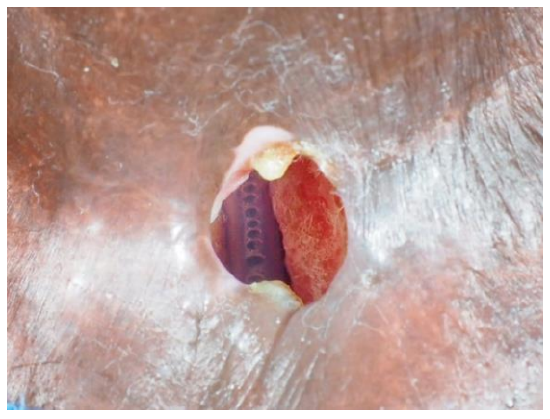
Figure 4: Very large TOF with the nasogastric feeding tube visible in the esophagus
Conservative management
- Most enlarged TOFs causing salivary leaks respond to conservative measures to shrink the diameter of the fistula such as reducing the size of the prosthesis or replacing it with a smaller sized urinary catheter
- Some patients may have to abandon tracheoesophageal speech because of continued leakage with aspiration, or failed phonation.2 In such cases the prosthesis is removed and the patient is fed via a nasogastric feeding tube until the fistula seals spontaneously, usually within 2 weeks after removal of the prosthesis
- If the fistula remains patent but is small, silver nitrate or electrical cauterization may be applied to the fistula4
- Alternative methods include
- Insertion a silicone septal button5
- Purse-string suture around the TOF
- Fat6 / collagen / Teflon injection around the TOF7
Surgical closure of TOF
If above conservative treatments fail, or there is a very large TOF as in Figure 4, surgical closure of a TOF becomes necessary. Repuncture with placement of a new tracheoesophageal prosthesis is possible sometime after closure of the problematic fistula. Candidates for surgical closure should also be counseled about alternative methods of voice rehabilitation e.g. esophageal speech and electrolarynx.
When planning closure of a TOF, assess the size of the stoma for the presence of stomal stenosis so that stomaplasty can be performed at the time of closure of the TOF.
TOFs are notoriously difficult to close, and the success rate is highly variable7 due to the poor blood supply of the irradiated and fibrotic tissue. Various methods of TOF closure have been reported:
- Layered closure
- Muscle rotation flaps (Sternocleidomastoid, pectoralis major)
- Free or pedicled fasciocutaneous flaps (radial forearm free flap3, deltopectoral8, supraclavicular flaps)
However, use of flaps is limited by the bulkiness of the flaps
The method described below is simple and does not require any flaps, unless closure of the esophageal defect will result in esophageal stenosis and requires reconstruction with a flap for that reason.
Surgical steps
- The procedure is performed under general anesthesia with intermittent apnea
- Intubate the patient via the tracheostoma with a small armored endotracheal tube
- Insert a nasogastric tube
- Prepare and drape to leave the neck exposed from the mandible down to the upper chest
- Local anesthetic with adrenaline is injected around edge of the tracheostoma
- Make a circumferential incision around the stoma with a 15 blade (Figure 5)
- Dissect 360 degrees along the wall of the trachea for a few centimeters, using electrocautery and dissecting scissors (Figure 5)
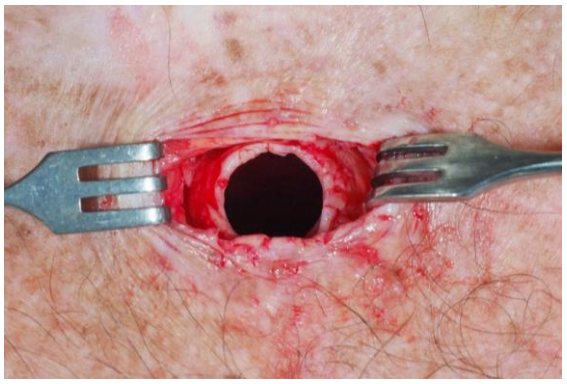
Figure 5: Tracheostoma incised circumferentially and for a few centimeters along the wall of the trachea
- Posteriorly, dissect carefully with scissors in a plane between the membranous part of the trachea and the anterior wall of the esophagus (Figure 6)
- Avoid accidentally opening into the esophagus
- Continue the dissection inferiorly beyond the TOF (Figure 6); dense fibrosis between the trachea and esophagus can make identification of the TOF difficult
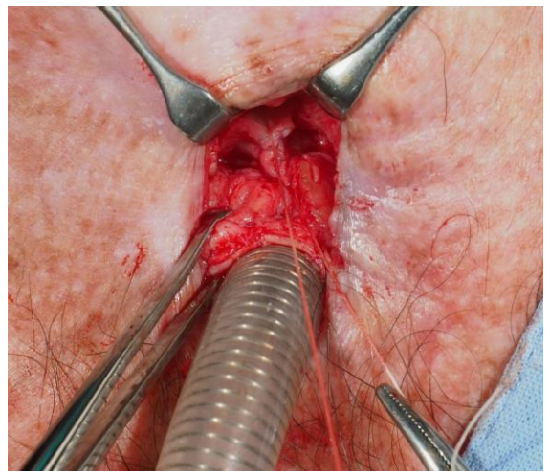
Figure 6: TOF identified and divided. The esophageal defect is being closed with 3-0 Vicryl sutures
- With the fistula identified, it is divided. Leakage of saliva or mucus may be seen from the esophageal side
- Oversew the esophageal mucosa with interrupted 3-0 absorbable Vicryl
- Resect the proximal trachea beyond the TOF
- Mobilize the trachea so that it comfortably reaches the skin surface (Figure 7)
- Suture the trachea to the skin edge with 2-0 Vicryl or Nylon stitches using a modified mattress technique
- No drain is required

Figure 7: Trachea is mobilized and proximal tracheal rings are resected inferior to the level of the TOF

Figure 5: Tracheostoma is closed with 2-0 Vicryl or Nylon stitches using modified mattress sutures
Postoperative Care
- Patient is kept nil by mouth for 5-7 days, and fed via the NGT
- A secondary TOF can be made once the wounds have healed and matured, not sooner than a month after surgery
- Reinserting a prosthesis too soon may result in the prosthesis having to be replaced with a shorter length prosthesis as the scar matures
Case of exposed common carotid artery
This case illustrates the proximity of the common carotid artery to the trachea, and the need to maintain a dissection plane on the tracheal wall. The patient had a very large tracheoesophageal fistula that had developed spontaneously some years after surgery and radiation therapy (Figures 4, 6). During the dissection the common carotid artery was noted to be covered by only a thin layer of scar tissue in the left lateral wall of the tracheostoma with the tracheal rings having resorbed (Figure 7). The trachea was stuck down and fibrotic, and mobilizing the trachea was not possible.

Figure 6: Large tracheoesophageal fistula with nasogastric tube visible in the midline
The carotid artery was carefully exposed over a length of 3 cm (Figure 7). The esophageal fistula was repaired with 3-0 Vicryl.
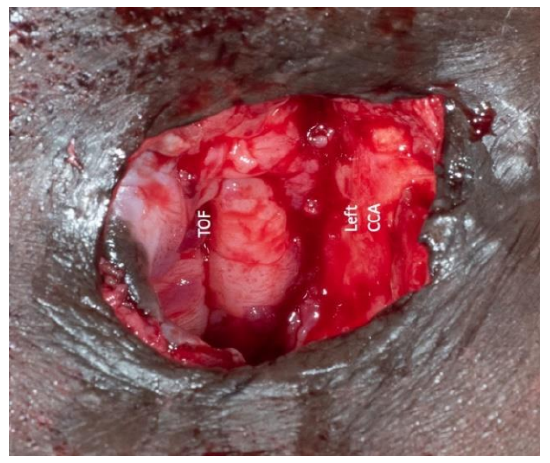
Figure 7: After dissecting the trachea around the stoma, we noted a medialized left common carotid artery (CCA) situated in the lateral wall of the tracheostoma
A supraclavicular flap was designed (Figures 8-10) and tunneled into the stoma to cover and isolate the carotid from the tracheostoma to avoid carotid artery blowout in the future.

Figure 8: Supraclavicular flap design

Figure 9: Raised supraclavicular island flap
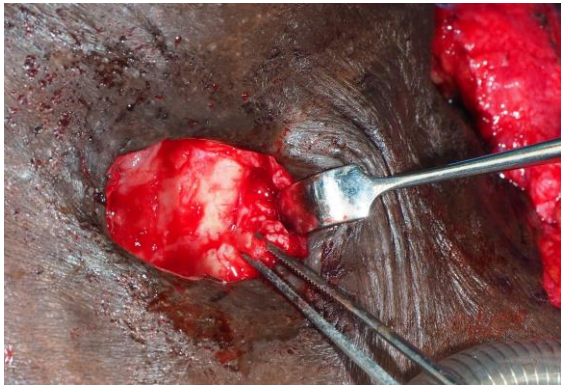
Figure 10: Exposed common carotid artery before flap inset

Figure 11: Supraclavicular flap inset to cover the exposed common carotid and overlay the oesophageal repair
References
- Myers EN. Closure of Tracheoesophageal Fistula. Ch 51 - Operative Otolaryngology, Head and Neck Surgery 2 nd Ed. (2008) ISBN: 9780323248013
- Stafford FW. Current indications and complications of tracheoesophageal puncture for voice restoration after laryngectomy. Curr Opin Otolaryngol Head Neck Surg. 2003;11(2):89-95
- Wreesmann VB, Smeele LE, Hilgers FJ, Lohuis PJ. Closure of tracheoesophageal fistula with prefabricated revascularized bilaminar radial forearm free flap. Head Neck. 2009;31(6):838-42
- Hosal SA, Myers EN. How I do it: closure of tracheoesophageal puncture site. Head Neck. 2001;23(3):214-6
- Schmitz S, Van Damme JP, Hamoir M. A simple technique for closure of persistent tracheoesophageal fistula after total laryngectomy. Otolaryngol Head Neck Surg. 2009;140(4):601-3
- Perie S, Ming X, Dewolf E, St Guily JL. Autologous fat injection to treat leakage around tracheoesophageal puncture. Am J Otolaryngol. 2002;23(6):345-50
- Moerman M, Vermeersch H, Heylbroeck P. A simple surgical technique for tracheoesophageal fistula closure. Eur Arch Otorhinolaryngol. 2004;261 (7):381-5
- Murono S, Ishikawa E, Nakanishi Y, et al. Closure of tracheoesophageal fistula with prefabricated deltopectoral flap. Asian J Surg. 2016;39(4):243-6
Author
Wing Chi Zenon Yeung MBChB (CUHK),
FHKCORL, FHKAM, FRCSEd (ORL)
Associate Consultant
United Christian Hospital and Tseung
Kwan O Hospital, Hong Kong SAR
Honorary Clinical Assistant Professor
Department of Otorhinolaryngology, Head and Neck Surgery
The Chinese University of Hong Kong
Hong Kong SAR
dr.zenon.yeung@gmail.com
Author & Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za

The Open Access Atlas of Otolaryngology, Head & Neck Operative Surgery by Johan Fagan (Editor) johannes.fagan@uct.ac.za is licensed under a Creative Commons Attribution - Non-Commercial 3.0 Unported License