1.21: Neck Dissection Using the Fascial Plane Technique
- Page ID
- 17638
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
NECK DISSECTION USING THE FASCIAL PLANE TECHNIQUE
Patrick J Bradley & Javier Gavilán
The importance of identifying the presence of metastatic neck disease with head and neck cancer is recognized as a prominent factor determining patients’ prognosis. The current available techniques to identify disease in the neck all have limitations in terms of accuracy; thus, elective neck dissection is the usual choice for management of the clinically N0 neck (cN0) when the risk of harboring occult regional metastasis is significant (≥20%)1. Methods available to identify the N+ (cN+) neck include imaging (CT, MRI, PET), ultrasound-guided fine needle aspiration cytology (USGFNAC), and sentinel node biopsy, and are used depending on resource availability, for the patient as well as the local health service. In many countries, certainly in Africa and Asia, these facilities are not available or affordable. In such circumstances patients with head and neck cancer whose primary disease is being treated surgically should also have the neck treated surgically.
Employing fascial planes as a concept to perform excision of neck nodal areas is based on specific anatomic concepts regarding the relationship between the lymphatic structures and their distribution within the tissues of the neck2-4. It is crucial that the anatomical description of the fascial layers is reviewed as its understanding is essential to understand the rationale and surgical technique of the procedure.
This technique for performing a neck dissection was proposed by Osvaldo Suárez, an Argentinean professor of anatomy and otolaryngologist, in the early 1960s; he proposed the term “vaciamento ganglionar functional” or “functional neck dissection”2,3. While he himself only published his work in Spanish, this procedure was popularized in the English world in the mid-20th century by Etore Bocca, an Italian otolaryngologist, and his colleagues5.
Fascial compartments allow the removal of cervical lymphatic tissue by separating and removing the fascial walls of these “containers” along with their contents from the underlying vascular, glandular, neural, and muscular structures.
Anatomical basis
The basic understanding of fascial planes in the neck is that there are two distinct fascial layers, the superficial cervical fascia, and the deep cervical fascia (Figures 1A-C).
Superficial cervical fascia
The superficial cervical fascia is a connective tissue layer lying just below the dermis. Surgically it is indistinct from the fatty tissue that surrounds it. The neck is one of the few places where it splits to surround the muscles of facial expression. The space deep to this layer contains fat, neurovascular bundles and lymphatics. It does not constitute part of the deep neck space system.
Deep cervical fascia(Figures 1A-C)
The deep cervical fascia encloses the deep neck spaces and is further divided into 3 layers, the superficial, middle and deep layers of the deep cervical fascia.
Superficial layer of deep cervical fascia(Figure 1A)
The superficial layer of the deep cervical fascia arises posteriorly from the vertebral spinous processes and ligamentum nuchae. It surrounds the entire neck, splitting to enclose the trapezius muscle, the omohyoid muscle, parotid gland, sternocleidomastoid muscle and the strap muscles. Anteriorly this fascia is attached to the hyoid bone. The inferior attachments of the fascia are the acromion of the scapula, the clavicle and the sternum. The fascia remains split in two layers until it attaches to the sternum; thus, the superficial layer attaches to the anterior surface of the sternum and posterior layer to the posterior surface of the sternum.
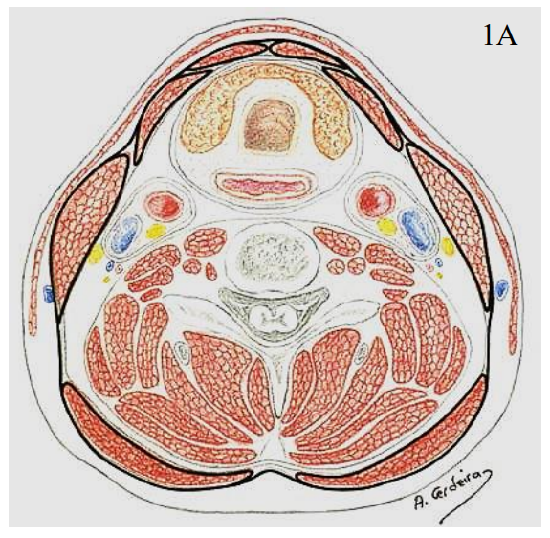
Figure 1A: Horizontal cross-section of neck at level of 6 th cervical vertebra showing superficial layer of deep cervical fascia
Deep layer of deep cervical fascia (Figure 1B)
The deep layer of the deep cervical fascia is also called “pre-vertebral fascia” because it constitutes a prominent layer just in front of the vertebral column. This fascia also arises posteriorly from the transverse and spinous processes of the cervical vertebrae and the ligamentum nuchae. It passes laterally around the prevertebral and postvertebral muscles and covers the scalene muscles anteriorly, then passes in front of the vertebral body and forms a thick layer from which it receives its name. This thick fascial layer forms the floor of the posterior triangle of the neck, and anterior to the vertebral bodies, it provides a base on which the pharynx, esophagus, and other cervical structures glide during swallowing and neck movements.
The cervical plexus emerges from between the scalene muscle bundles. The phrenic nerve crosses obliquely on the anterior surface of the anterior scalene muscle from lateral to medial and lies deep to the prevertebral fascia. The cervical and brachial nerve plexuses and the sympathetic trunk are invested by the prevertebral fascia, which forms the floor of the lateral triangle of the neck. The consequences of elevating the prevertebral fascia during neck dissection, beyond merely increasing the devastation wrought by the surgical exercise, can be severe. If this fascia is raised, there is risk of injuring what lies deep in the fascia, notably the cervical and brachial plexus, the sympathetic trunk, and the phrenic nerve.
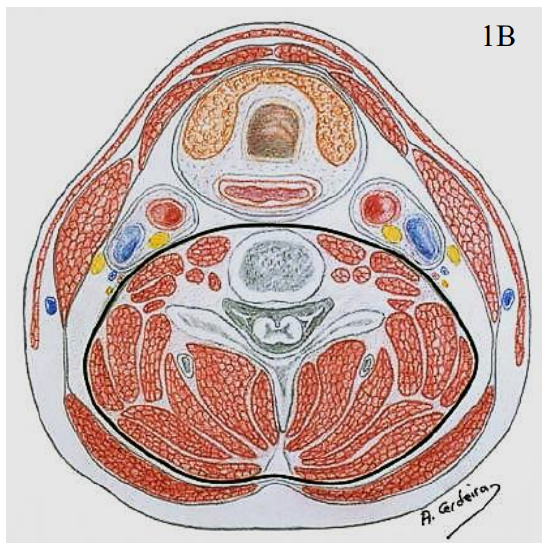
Figure 1B: Horizontal cross-section of neck at level of 6th cervical vertebra showing deep layer of deep cervical fascia
Middle layer of deep cervical fascia (Figure 1C)
The middle layer of the deep cervical fascia or “pretracheal fascia” has two divisions, muscular and visceral. The muscular division surrounds the strap muscles (sternohyoid, sternothyroid, thyrohyoid, omohyoid) and the adventitia of the great vessels. The visceral division surround the constrictor muscles of the pharynx and esophagus to create the buccopharyngeal fascia and the anterior wall of the retropharyngeal space. Both the muscular and visceral divisions contribute to the carotid sheath. The middle layer also envelopes the larynx, trachea, and thyroid gland. It attaches to the base of the skull superiorly and extends inferiorly as low as the pericardium via the carotid sheath.
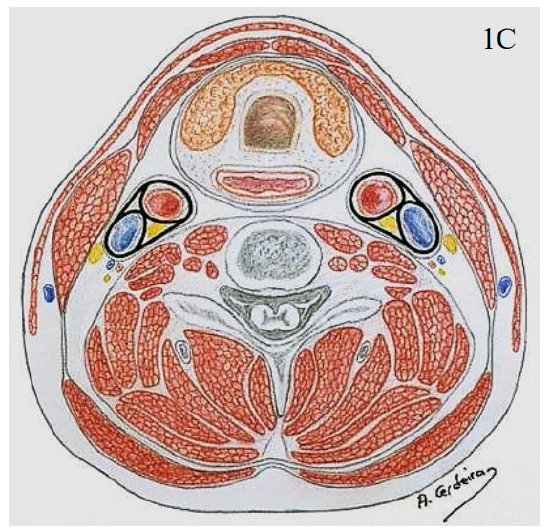
Figure 1C: Horizontal cross-section of neck at level of 6th cervical vertebra showing carotid sheaths
Indications for fascial plane technique
To ensure oncologic safety, fascial plane surgery requires that all nodal disease be confined within lymphatic tissues
- Ideally suited to N0 necks at high risk of harbouring occult metastases e.g oral cavity, oropharynx, and supraglottis
- Can be performed simultaneously on both sides of the neck without increasing morbidity
- May be considered when nodes measure < 2.5-3.0 cm in greatest diameter, and are discrete and mobile (with caution)
- Small aggregated or matted nodes that are mobile (with caution)
Contraindications
- Large nodes > 3.0 cm (usually fixed)
- Previously treated neck, either surgically or non-surgically
Should a surgeon be concerned that nodal disease is exhibiting aggressive features e.g. soft tissue invasion or fixity, then the procedure should be converted to a “modified radical neck dissection”.
Surgical technique
The technique described below encompasses all the cervical levels and aims to preserve major non-lymphatic structures. To facilitate teaching, the surgical steps are sequentially detailed. However, depending on the clinical situation, the operation may be modified so that only the cervical levels most at risk of harboring metastases are included in the dissection.
The operation is performed under general anesthesia, with the patient in the supine position and the neck fully extended. Elevating the upper half of the operating table to 30º reduces bleeding.
The surgery is best performed by dissecting along the fascial planes with a scalpel; the fascial planes of the neck are mainly avascular and can be easily followed with the scalpel. It is essential that an assistant apply firm countertraction on the tissues to permit easy, speedy and effective surgical forward progressive progress to be achieved.
Incisions and flaps
The placement and type of skin incision(s) depend on the site of the primary tumor and whether the primary tumor and the neck are to be addressed synchronously, or whether the neck dissection is being performed alone, and whether the neck dissection is to be unilateral or bilateral. Naturally the personal bias of the surgeon should also be considered.
After the skin incision, subplatysmal skin flaps are elevated, preserving the superficial layer of the cervical fascia. The limits of tissue elevation are similar to those of the classic radical neck dissection (Figures 2A, B).
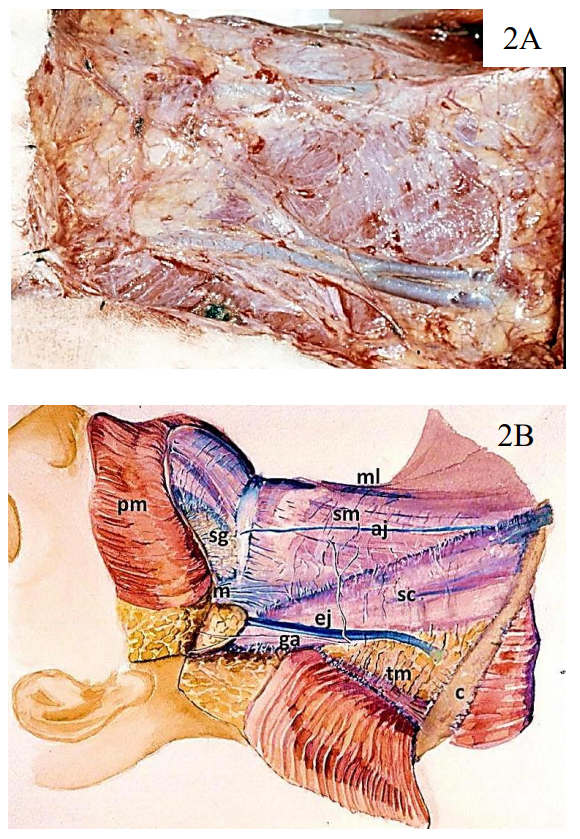
Figure 2: (A) Surgical view of right neck after skin flaps have been elevated. (B) Boundaries and anatomic landmarks of a complete right sided neck dissection (ml: Midline; bm: Inferior border of mandible; c: Clavicle; tm: Trapezius muscle; ga: Greater auricular nerve; sc: Sternocleidomastoid muscle; sm: Strap muscles; pm: Platysma muscle; ej: External jugular vein; aj: Anterior jugular vein; sg: Submandibular gland
Dissecting the sternocleidomastoid (SCM) muscle
This step completely unwraps the SCM from its surrounding superficial layer of deep cervical fascia. Before approaching the fascia of the SCM muscle, the external jugular vein is ligated and divided. Dissection of the SCM commences with a longitudinal incision in the fascia along the entire length of the muscle (Figure 3).
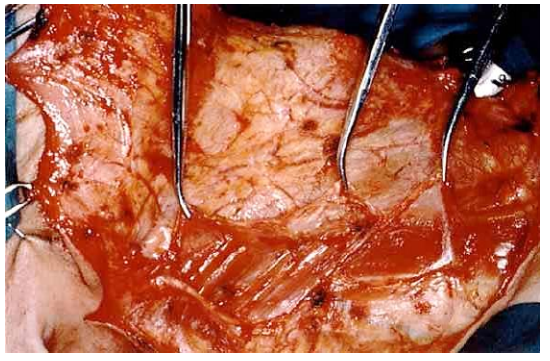
Figure 3: Longitudinal incision over the entire length of the posterior border of the SCM muscle. The fascia is being retracted anteriorly with hemostats
This incision is placed near the posterior border of the muscle. With the application of several hemostats the fascia is retracted anteriorly while the surgeon carries out the subfascial dissection toward the anterior margin of the muscle. Fascial retraction should be performed with extreme care since the thin superficial layer of the cervical fascia is the only tissue now included in the specimen (Figure 4).

Figure 4: The fascia dissected from the SCM muscle
When the dissection reaches the anterior border of the SCM, the muscle is retracted posteriorly to continue the dissection over its medial surface (Figures 5 A, B).
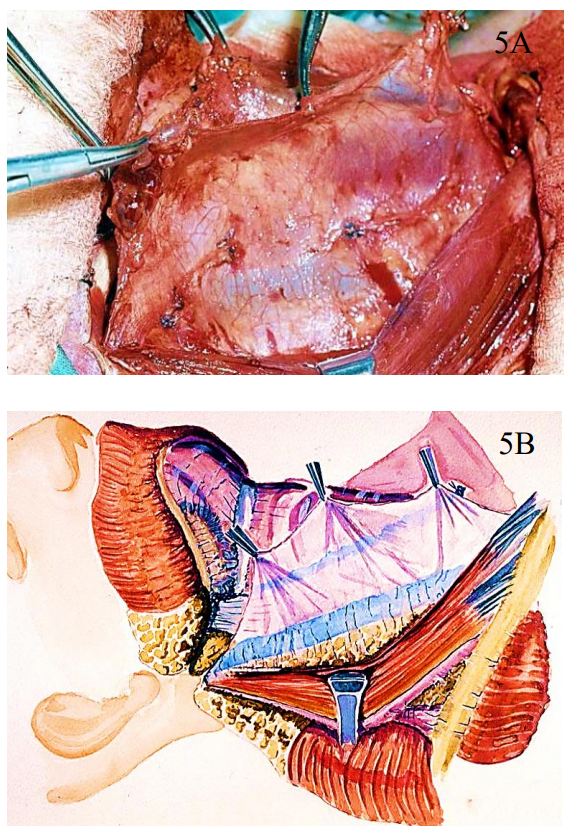
Figure 5: (A) Dissection of SCM muscle continues over its medial surface. (B) The contents of the carotid sheath can be seen shining through the fascia
As the deep medial surface of the muscle is approached, small perforating vessels are identified entering the muscle through the fascia. These are cauterised sequentially, allowing the surgeon to continue mobilizing the entire medial surface of the SCM muscle. Attention and care needs to be increased when dissecting the upper half of the SCM muscle where the spinal accessory nerve (SAN) enters the muscle, approximately at the junction of the upper and middle thirds of the muscle. The transverse process of the atlas serves as a useful anatomic landmark to locate the SAN (Figure 6).
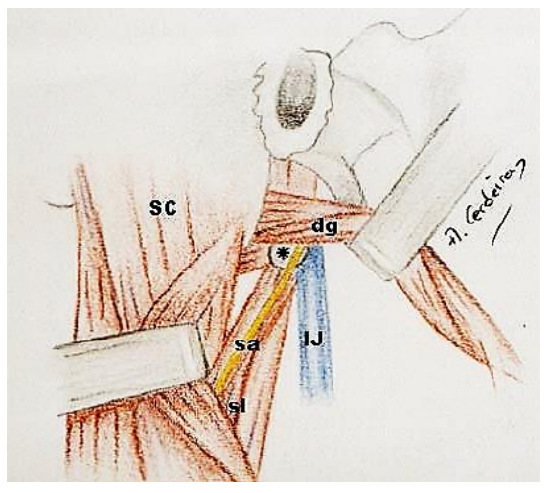
Figure 6: Anatomic landmarks to locate the spinal accessory nerve in its course between the internal jugular vein and the SCM muscle on the right side. (*: Transverse process of atlas; sa: Spinal accessory nerve; IJ: Internal jugular vein; dg: Digastric muscle; sl: Splenius capitis and levator scapulae muscles; SC: SCM muscle
As the dissection progresses posteriorly along the entire length of the SCM muscle, the internal jugular vein is seen through the fascia of the carotid sheath (Figure 5). The use of wet sponges aid to identify the fascia that still covers the posterior border of the SCM muscle. This fascia must be dissected posteriorly and slightly medially underneath the muscle, to meet the anterior dissection. This maneuver completely releases the muscle from its surrounding fascia.
Including the posterior triangle of the neck in the dissection requires a combined approach, both posterior and anterior to the SCM muscle (Figure 7).
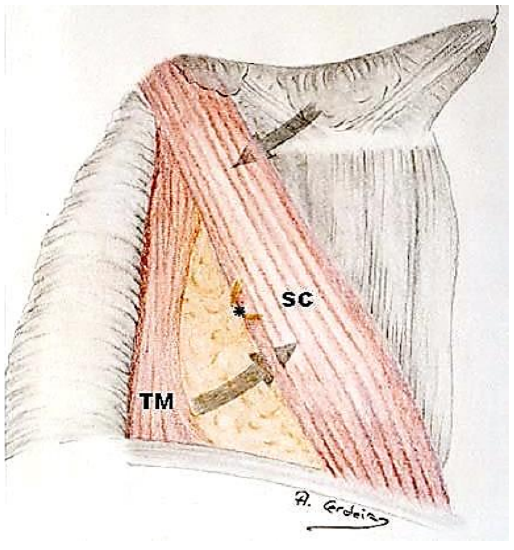
Figure 7: Schematic view of the approach to the neck for a complete neck dissection. Above Erb’s point the operation is performed anterior to the SCM muscle. The lower part of the posterior triangle is approached posterior to the SCM muscle. (SC: Sternocleidomastoid muscle; TM: Trapezius muscle; *: Erb’s point
In the upper half of the neck (above Erb’s point) the dissection is performed anterior to the SCM muscle, whereas in the lower half of the neck (below Erb’s point) the dissection is performed posterior to SCM muscle. The tissue dissected from the lower half of the neck (supraclavicular fossa) is then be passed beneath the SCM muscle to join the main part of the specimen. When the posterior triangle is not included in the resection, the whole dissection can be performed from anterior to the SCM muscle.
Dissecting the submandibular triangle
The next step is to resect the submental and submandibular lymph nodes (Levels 1a, b). This level is at risk in patients with cancers of the oral cavity and oropharynx, but is unlikely to be involved in patients with larynx, hypopharynx and thyroid cancers. The submandibular gland does not need to be resected as, unlike the parotid gland, there are no lymph nodes within the substance of the gland 6.
After the flaps have been raised the submandibular gland is visible through the superficial layer of cervical fascia in the upper part of the surgical field. The fascia is incised at the level of the lower border of the submandibular gland from the midline to the tail of the parotid gland as for a gland removing procedure. Then the facial vein is ligated and divided, and is reflected upwards by the superior ligature to displace and preserve the marginal mandibular branch of the facial nerve (Figure 8).
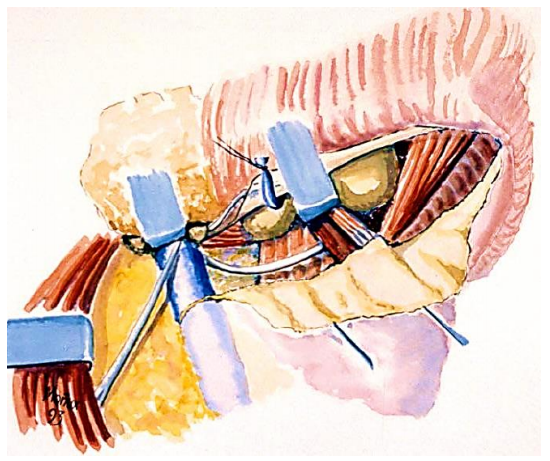
Figure 8: Protecting the marginal mandibular branch of the facial nerve by elevating the distal stump of the ligated facial vein over the mandible
The retromandibular vein and the external jugular vein are ligated and divided. Now, instead of including the submandibular gland within the specimen, its fascia is reflected inferiorly while the gland is retracted superiorly (Figure 9).
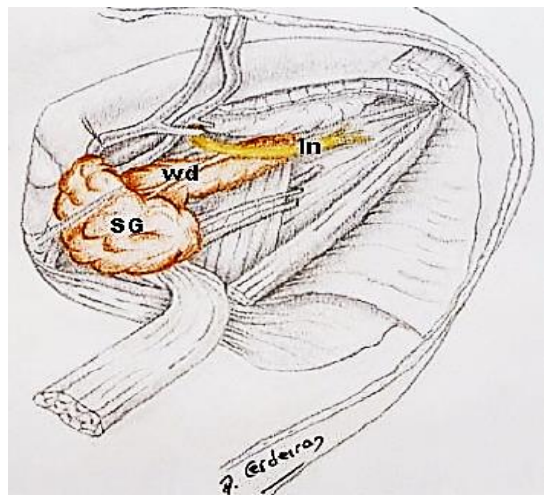
Figure 9: Anatomic relations of the lingual nerve in the submandibular triangle. (ln: Lingual nerve; SG: Submandibular gland; wd: Wharton’s duct)
The fibrofatty tissue containing the submandibular nodes is grasped and dissected off the submandibular triangle preserving the gland. The dissection may be continued medially to include the submental nodes but this is seldom required in tumors that allow preservation of the submandibular gland.
The dissection is continued over the digastric and stylohyoid muscles. These muscles are retracted superiorly and the fascial sheath is easily dissected from the subdigastric and upper jugular spaces.
The hypoglossal nerve is identified (Figure 10) and the dissection is continued along the nerve, carefully dividing and ligating the lingual veins as they may be a troublesome source of bleeding.
The specimen is reflected inferiorly and the fascia over the digastric and stylohyoid muscles is incised from the midline to the tail of the parotid gland. Following the posterior belly of the digastric muscle the stylomandibular ligament is transsected (Figure 11a).
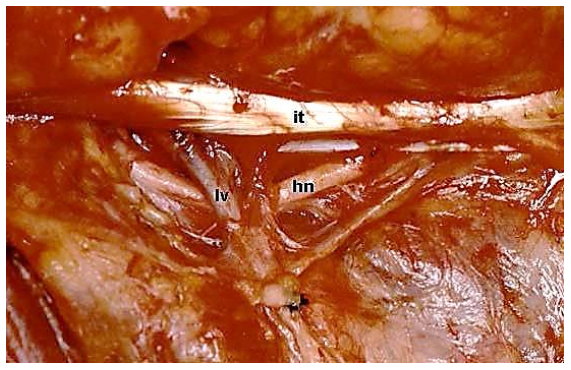
Figure 10: The hypoglossal nerve is identified underneath the intermediate tendon of the digastric muscle. A lingual vein can be seen crossing superficial to the nerve (hn: Hypoglossal nerve; it: Intermediate tendon of the digastric muscle; lv: Lingual vein crossing hypoglossal nerve)
At this level, the retromandibular vein, the posterior auricular vein and the external jugular vein are identified, ligated and divided according to their anatomical distributions. Depending on the lower extension of the tail of the parotid gland, part of the gland may also be included in the resection. This facilitates visualisation of the upper jugular nodes as well as includes in the specimen the infraparotid lymph nodes.
The dissected tissue is finally retracted inferiorly and dissected free from the subdigastric and upper jugular spaces. The specimen at this stage includes the submental and submandibular lymph nodes (Level I), and the uppermost jugular nodes (Level IIa).
Dissecting spinal accessory nerve (SAN)
The SAN runs within the “soft tissue” of the neck, so that one must divide the tissue overlying the nerve, rather than to follow a fascial plane. Dissecting the SAN is usually performed with scissors rather than a scalpel because of the loose consistency of the tissue in this area and the restricted access. The SCM muscle is retracted posteriorly and the posterior belly of the digastric muscle is retracted superiorly with a retractor. It is important to identify the entire SAN between the SCM muscle and the internal jugular vein (IJV). Usually the IJV lies immediately behind the proximal portion of the nerve. Occasionally the nerve may go behind the vein or even cross it (Figures 11a-c).
Once the SAN has been exposed, the tissue lying superior and posterior to the nerve is dissected free from the splenius capitis and levator scapulae muscles. When the dissected tissue (Level IIb) reaches the level of the SAN it is passed beneath the nerve to be removed in continuity with the main part of the specimen (Figure 11b).
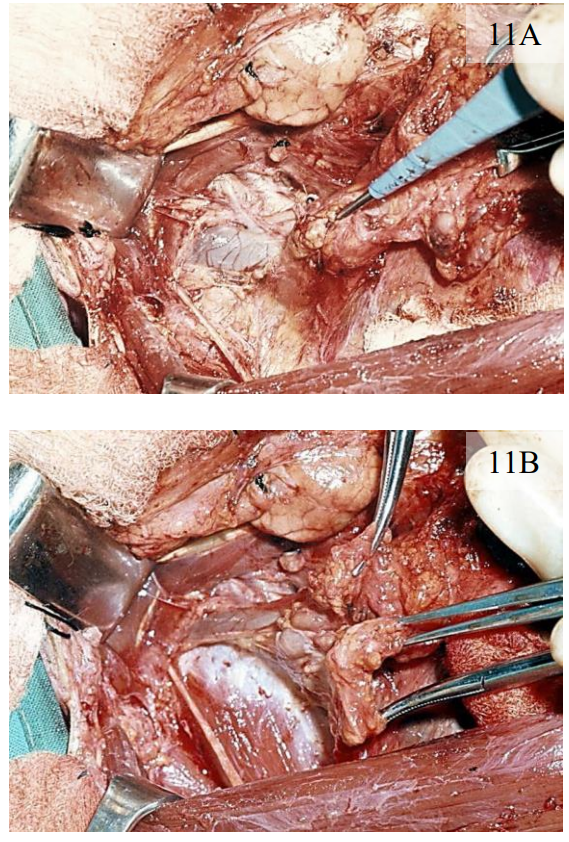
Then the specimen is further freed by making an incision into the tissues located below the entrance of the SAN into the SCM muscle, down as far as the level of Erb’s point.
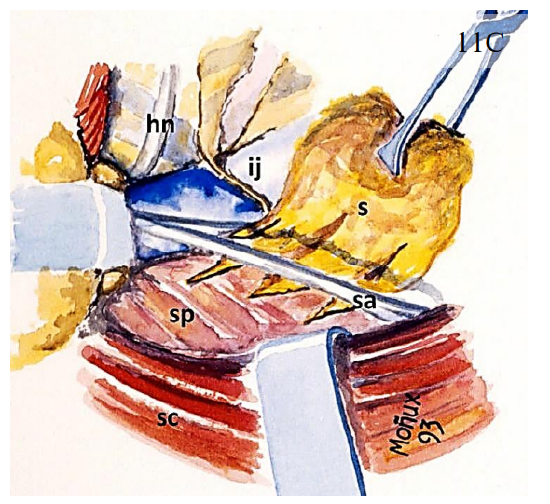
Figures 11 A-C: The “spinal accessory manoeuvre” allows removal of the tissue lying posterior and superior to the nerve in continuity with the rest of the specimen. (A) The nerve is exposed between the SCM muscle and the internal jugular vein. (B) The fibrofatty tissue lying posterior and superior to the nerve is passed beneath the nerve. (C) Artist’s view of the “spinal accessory manoeuvre” on the right side of the neck. (sa: Spinal accessory nerve; ij: Internal jugular vein; s: Specimen; sc: SCM muscle; sp: Splenius capitis muscle)
Dissecting posterior triangle of neck
To facilitate exposure of supraclavicular area (Level Vb), this region is approached from posterior to the SCM muscle (Figure 12). The loose fibrofatty tissue of the supraclavicular fossa and absence of well-defined dissection planes within this area make knife dissection ineffective, and it is best performed with scissors and blunt dissection.
The SCM muscle is retracted anteriorly and the external jugular vein is divided and ligated inferiorly in the neck if this had not be done previously. The dissection proceeds from the anterior border of the trapezius muscle in a medial direction including the lymphatic contents of the supraclavicular fossa. At the upper margin of this area is where damage to the SAN is most likely to occur.
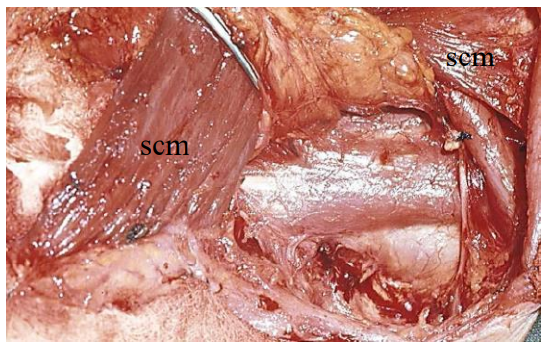
Figure 12: Dissection of the supraclavicular fossa. The SCM muscle (scm) is retracted anteriorly and the dissection proceeds posterior to the muscle until the scalene muscles are identified
The omohyoid muscle is next identified; its fascia is dissected off the muscle so that is may be removed with the contents of the posterior triangle. The muscle may be transected if necessary but may be retracted inferiorly to identify the transverse cervical vessels deep to the omohyoid muscle.
The deep layer of the cervical fascia overlying the levator scapulae and scalene muscles now comes into view. The brachial plexus is easily identified because it appears between the anterior and middle scalene muscles (Figure 13).
Remaining superficial to the scalene fascia (deep layer of the cervical fascia) prevents injuring the brachial plexus and the phrenic nerve. Dissection proceeds medially until the anterior border of the SCM muscle is reached. The muscle is retracted posteriorly and the dissection is continued anterior to the muscle towards the carotid sheath.
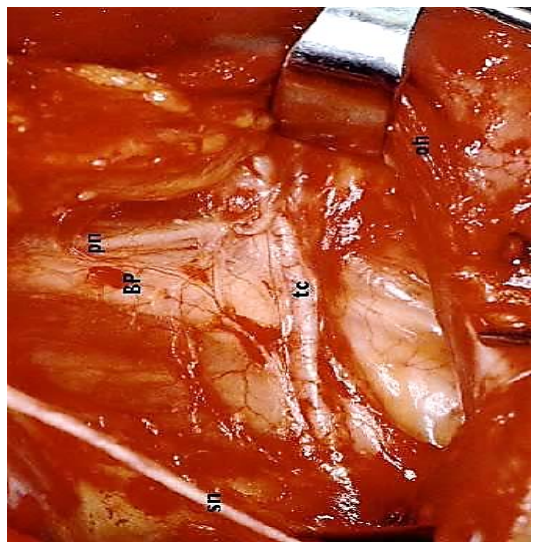
Figure 13: Anterior view of the anatomic landmarks of the right supraclavicular fossa. (BP: Brachial plexus; pn: Phrenic nerve; tc: Transverse cervical artery; sn: Supraclavicular branch of cervical plexus; oh: Omohyoid muscle retracted inferomedially)
Dissecting the deep cervical muscles
As the dissection proceeds medially towards the carotid sheath, several branches of the cervical plexus are found over the deep muscles of the neck (Figures 14 and 15A).
Optimal shoulder function may be preserved if the deep branches of the 2nd, 3rd, and 4th cervical nerves are preserved, as they may communicate with the SAN. There are also similar anastomoses from the 3rd, 4th and 5th cervical nerves to the phrenic nerve – these should also be preserved. Preservation of these nerves is best achieved by keeping the dissection superficial to the scalene fascia.
Continuing the dissection posterior to the carotid sheath carries a high risk of damage to the sympathetic chain.
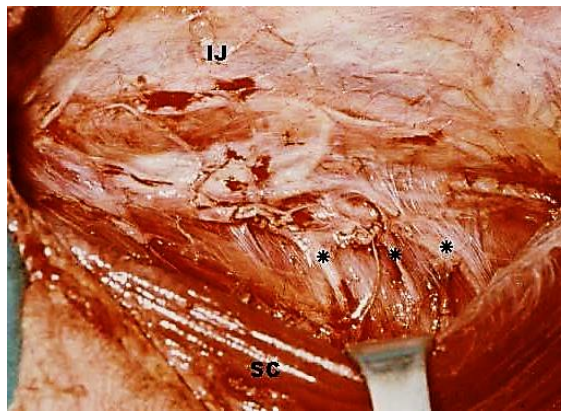
Figure 14: Lateral view of the deep branches of the cervical plexus that have been preserved on the right side (SC: SCM muscle; IJ: Internal jugular vein; *: Deep branches of cervical plexus)
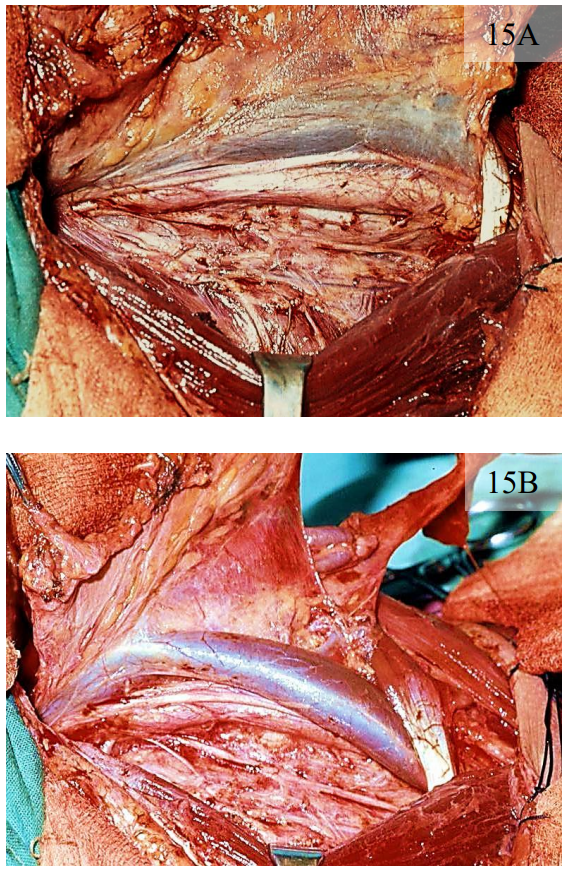
Figures 15A, B: Dissecting carotid sheath
Dissecting the carotid sheath
This part of the dissection is best executed with a knife while applying adequate countertension to the tissues. The surgical specimen is grasped with hemostats and retracted medially, while the surgeon uses a gauze pad in the non-dominant hand to pull laterally over the deep cervical muscles.
An incision is made with the scalpel along the entire length of the carotid sheath over the vagus nerve. The fascia is then dissected from the internal jugular vein. This is achieved by continuously passing the knife blade up and down along the wall of the internal jugular vein along its entire length. The fascia can be seen parting from the vein after each pass of the blade, until the internal jugular vein is completely released from its fascial covering (Figure 15B).
The facial, lingual, and thyroid veins are next clearly identified, ligated, and divided to complete the isolation of the internal jugular vein.
Dissection of the carotid sheath has two danger points for surgeons – at the top and the bottom of the dissection. The surgeon must be extremely cautious to avoid injuring the vein at these two points as traction exerted at these two points to facilitate dissection of the fascial envelope produces a folding of the wall of the internal jugular vein that is easily cut at the touch of the scalpel blade.
Low in the neck, the terminal portion of the thoracic duct on the left, and the right lymphatic duct – when present – also are within the boundaries of the dissection and must be preserved.
Following release of the internal jugular vein from its fascia, the dissection proceeds medially over the carotid artery. The specimen is now completely separated from the great vessels, remaining attached only to the strap muscles.
Dissecting the strap muscles
This may be the last step or may already have been performed at an earlier stage of the operation, depending on the preference surgeon or the location of the primary tumor. The midline of the neck constitutes the medial margin of the neck dissection.
This the superficial layer of the deep cervical fascia is incised in the midline from the upper border of the surgical field to the sternal notch. The anterior jugular vein is identified, ligated, and divided at both ends of the surgical field. The fascia is now dissected from the underlying strap muscles. The dissection starts at the upper part of the surgical field and continues in a lateral and inferior direction. The sternohyoid and omohyoid muscles are completely freed from their fascial coverings (Figures 16 A, B).
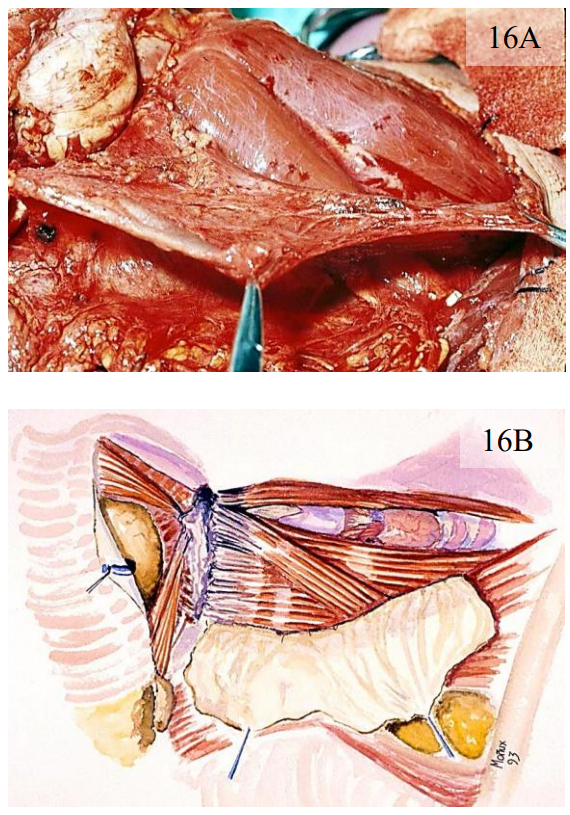
Figure 16: (A) Dissection of strap muscles. (B) Artist’s view of dissection of the fascia covering the strap muscles
At this point the specimen is almost free and any remaining vessels - arteries or veins - should be ligated and divided unless required for some other procedure such as anastomosis of a free flap!
Dissecting the central compartment
During dissection of the central compartment (Level VI), the recurrent laryngeal nerves must be identified and followed upwards to the larynx and downwards to the upper mediastinum. The lobe of the thyroid, if being preserved, makes such surgery difficult, as preservation of the parathyroid glands is extremely important with its functioning blood supply.
Closure of wound
The neck is carefully inspected for bleeding points and retention of sponges etc. The entire wound is irrigated with saline (Figure 17).
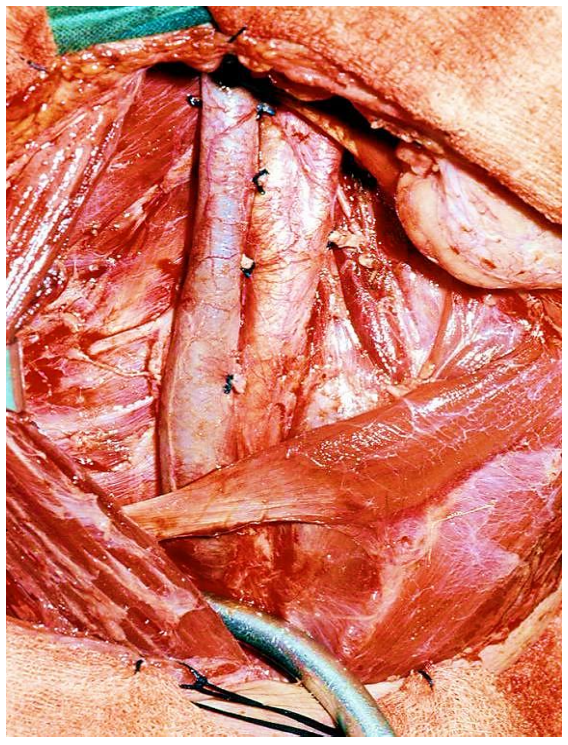
Figure 17: Image of the right neck after a neck dissection. Note the preserved submandibular gland
The skin is closed in two layers over a large suction drain. The platysma is sutured with absorbable buried sutures, and the skin closure with skin clips.
Comment
While the term functional neck dissection has not been included in more recent classifications of neck dissection, the procedure as described is eminently suited to elective selective neck dissections (Level I, II, III and IV) and for therapeutic selective neck dissections for N1 necks.
Video
- Download: Functional neck dissection technique
- YouTube: https://www.youtube.com/watch?v=sdq QxbZMLlA
Other Open Access Atlas neck dissection chapters:
- Modified and radical neck dissection technique
- Selective neck dissection operative technique
References
- De Bree R, Takes RP, Castelijns JA, Medina, JE, Stoeckli SJ, Mancuso AA, Ferlito A. (2015). Advances in diagnostic modalities to detect occult lymph node metastases in head and neck squamous cell carcinoma. Head Neck, 37(12), 1829-39
- Gavilán J, Herranz J, Martin L, Functional neck dissection: the Latin approach. Operative Techniques in Otolaryngology 2004;15: 168 -75
- Ferlito A, Gavilán J, Buckley J, et al. Functional neck dissection: fact and fiction. Head Neck 2001; 23; 804-8
- Gavilán J, Heranz J, De Santo LW, Gavilán C: Functional and selective neck dissection. New York Thieme, 20025. Bocca E, Pignataro O, Sasaki CT, Functional neck dissection. A description of operative technique. Arch Otolaryngol 1980; 106: 524-7 6. Dhiwakar M, Ronen O, Malone J, et al. Feasibility of submandibular gland preservation in neck dissection: a prospective anatomic-pathologic study. Head Neck 2011;33-(5): 603-9
Copyright
Figures reproduced with permission of THIEME
Authors
Patrick J Bradley, MBA
FRCS Emeritus
Honorary Professor of Head and Neck Oncologic Surgery
Nottingham University Hospitals
Queens Medical Centre Campus
Nottingham, England
pjbradley@zoo.co.uk
Javier Gavilán, MD
Professor and Chairman
Department of
Otolaryngology La Paz University Hospital
Autonomous University of Madrid
Madrid, Spain
javier.gavilan@salud.madrid.org
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


