1.25: Parathyroidectomy
- Page ID
- 17646
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
PARATHYROIDECTOMY
Eugenio Panieri & Johan Fagan
Parathyroidectomy is indicated for primary hyperparathyroidism and for secondary hyperparathyroidism refractory to medical treatment (Figures 1, 2).
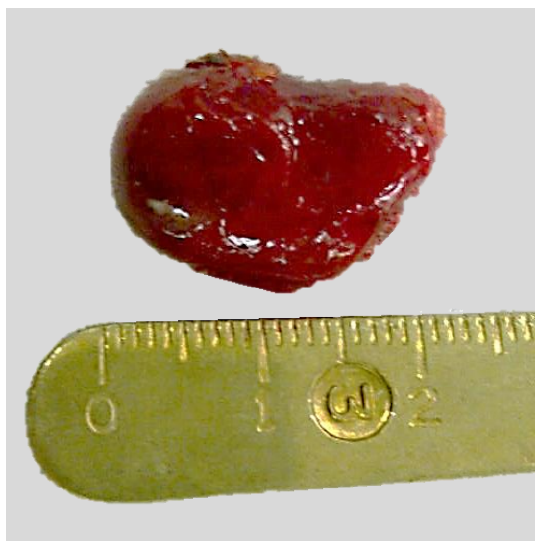
Figure 1: Typical parathyroid adenoma
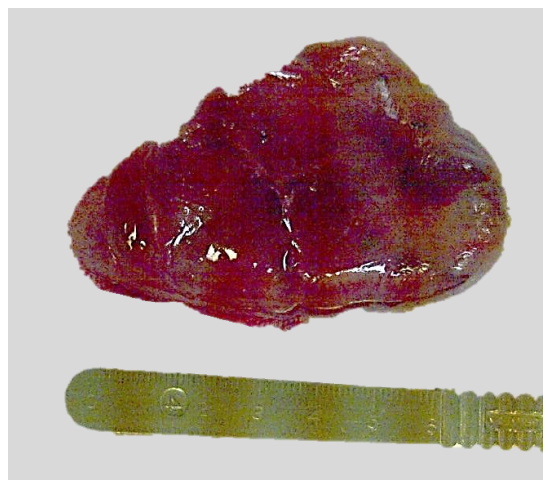
Figure 2: Giant sized adenoma
Surgical Anatomy
A detailed knowledge of parathyroid anatomy is essential to perform parathyroidectomy safely and effectively. Particular attention needs to be paid to identifying ectopic or unusually located glands and to avoid injury to important local structures, particularly the recurrent laryngeal nerve (RLN).
There are typically four parathyroid glands; supernumerary glands and <4 glands do occur. The parathyroids are generally located symmetrically in the neck in close proximity to the thyroid gland (Figure 3).
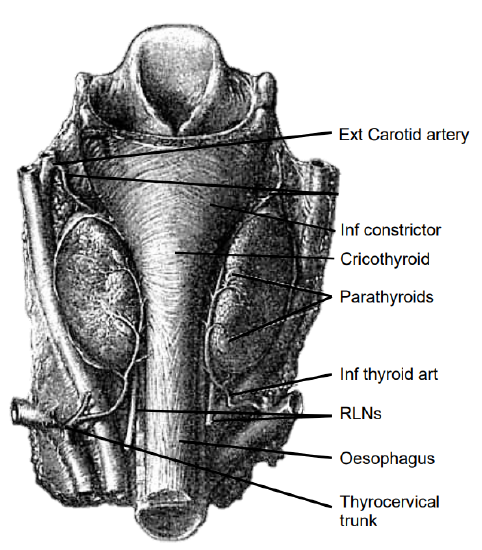
Figure 3: Posterior view of the thyroid gland demonstrating parathyroids, RLNs and superior and inferior thyroid arteries
Their characteristic golden-tan color varies from yellow to reddish brown. Their color permits for them to be distinguished from the pale-yellow lymph nodes, thymus, mediastinal fat, and the dark-red thyroid parenchyma. They have a diameter of about 3-8 mm and are usually oval-shaped, but may also be tear-shaped, drop-like, spherical, elongated, rod-like or flattened.
The superior parathyroid glands originate from the 4th pharyngeal pouch and adhere to the posterior surface of the caudally migrating thyroid. They have a much shorter distance to migrate than the inferior parathyroid glands; this would account for their more predictable location. They are embryologically and anatomically closely related to the Tubercle of Zuckerkandl and are usually found posteriorly at the level of the upper two-thirds of the thyroid about 1cm above the crossing point of the RLN and inferior thyroid artery (ITA) (Figure 4).
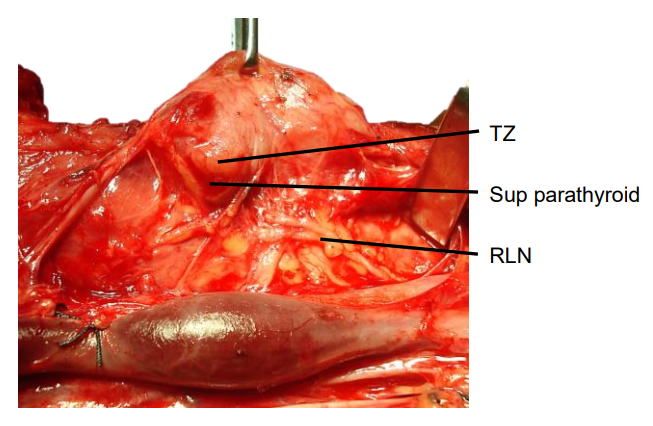
Figure 4: Tubercle of Zuckerkandl (TZ) and its relationship to the superior parathyroid gland and RLN
Ectopic superior parathyroids are uncommon (1%) and may be found in the posterior neck, retropharyngeal and retroesophageal spaces and intrathyroidally (Figure 5).
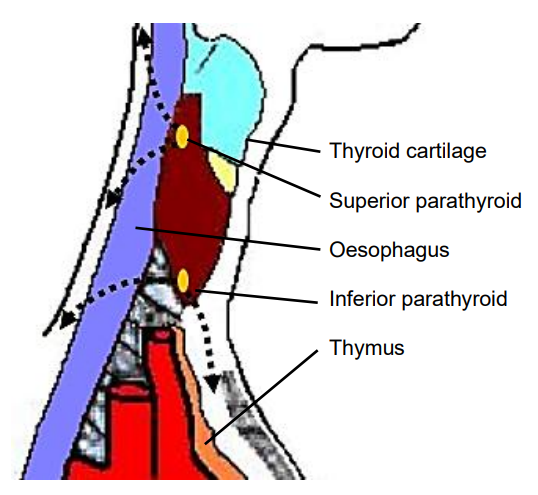
Figure 5: Ectopic parathyroids in retropharyngeal space and mediastinum
The inferior parathyroid glands arise from the dorsal wings of the 3rd pharyngeal pouches. They join the thymus as it migrates caudally and medially to its final position in the mediastinum. Ectopic inferior parathyroid glands can be found anywhere along this large area of descent from the proximal neck down to the superior border of the pericardium. Their commonest location is on the anterior or the posterolateral surfaces of the lower pole of the thyroid, between the lower pole of thyroid and thyroid isthmus (42%, Wang et al); or within the thyrothymic ligament in the lower neck in proximity to the thymus (39%). Other locations include lateral to the thyroid, within the carotid sheath (15%), or within mediastinal thymic tissue and pericardium (2%). (Figure 5).
The inferior parathyroids are usually found in a plane more ventral to that of the superior glands. If the RLN’s course is viewed in a coronal plane, then the superior parathyroid glands are located deep (dorsal) and the inferior parathyroid superficial (ventral) to the plane of the nerve (Figures 6, 7).
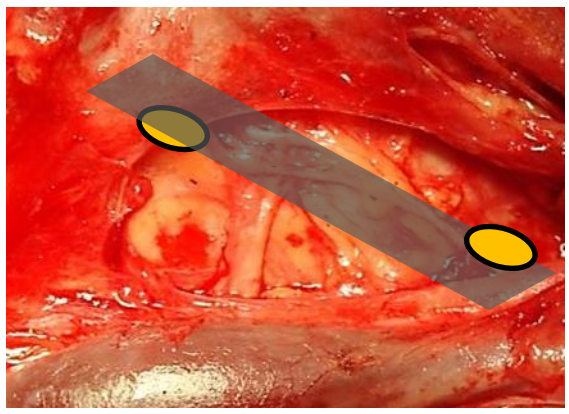
Figure 6: The superior parathyroid gland lies deep (dorsal) and the inferior parathyroid superficial (ventral) to a coronal plane along course of RLN
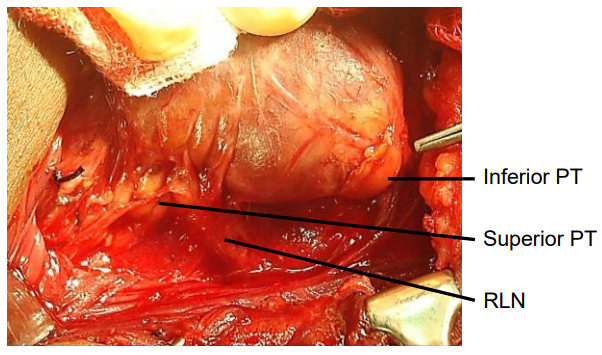
Figure 7: The superior and inferior parathyroids relative to a coronal plane along the course of the RLN
The inferior thyroid artery (ITA) is a branch of the thyrocervical trunk, which in turn arises from the subclavian artery (Figures 3, 5). It is the predominant vascular supply to both the upper and lower parathyroids (Figures 3, 8). Consequently, division of the main trunk of the ITA during thyroidectomy is discouraged as it places both parathyroids at risk of ischemic injury.
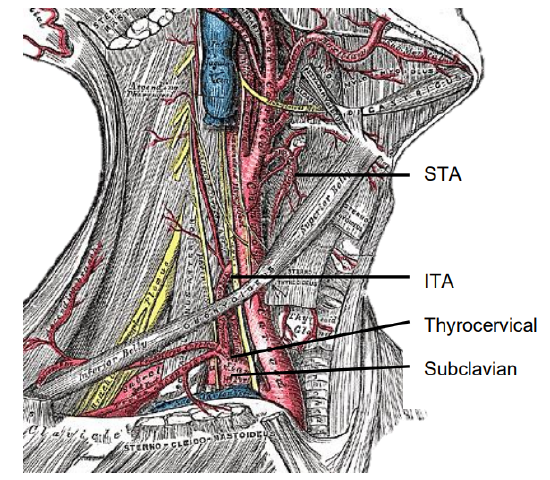
Figure 8: Superior thyroid artery (STA), subclavian artery, thyrocervical trunk and inferior thyroid artery (ITA)
The ITA courses superiorly along the surface of the anterior scalene muscle before turning medially behind the carotid sheath from where it reaches the inferior pole of the thyroid gland. It provides blood supply to the parathyroids, thyroid, upper esophagus and trachea. Its branches communicate with the superior thyroid artery (STA) and with the blood supply of the contralateral thyroid lobe via the thyroid isthmus.
The Recurrent Laryngeal Nerve (RLN) is a key structure in any exploration of the central neck. Identification and preservation of the RLN during thyroid and parathyroid surgery is essential to minimize morbidity. The RLN innervates all the intrinsic muscles of the larynx except the cricothyroid muscle (SLN) and provides sensory innervation to the larynx. Even minor neuropraxia may cause dysphonia; irreversible injury confers permanent hoarseness. The incidence of RLN injury during thyroidectomy is 0-28% and is the most common reason for medicolegal claims following thyroidectomy; the incidence of injury during parathyroidectomy is much lower.
The RLNs originate from the Xn. After circling around the subclavian artery (right) and aortic arch (left) the RLNs course superiorly and medially toward the tracheoesophageal groove (Figures 9, 10). The right RLN enters the root of the neck from a more lateral direction and its course is less predictable than that of the left. The RLNs enter the larynx deep to the inferior constrictor muscles and posterior to the cricothyroid joint.
The RLN may be non-recurrent in approximately 0.6% of patients i.e. it does not pass around the subclavian artery but branches from the Xn higher up in the neck, passing directly to the larynx close to the superior thyroid vessels (Figure 10). This aberration almost always occurs on the right side and is associated with a retroesophageal subclavian artery.
Knowledge of the anatomical relationships of the RLN to the tracheoesophageal groove, ligament of Berry, and ITA is essential. The course of the RLN with respect to the ITA is quite variable. Most commonly it crosses behind the branches of the artery, more predictably so on the left. However, the nerve may pass deep to, superficial to, or between the terminal branches of the ITA. Up to twenty anatomical variations have been described. In Figure 11 the RLN is seen to pass anterior to the artery.
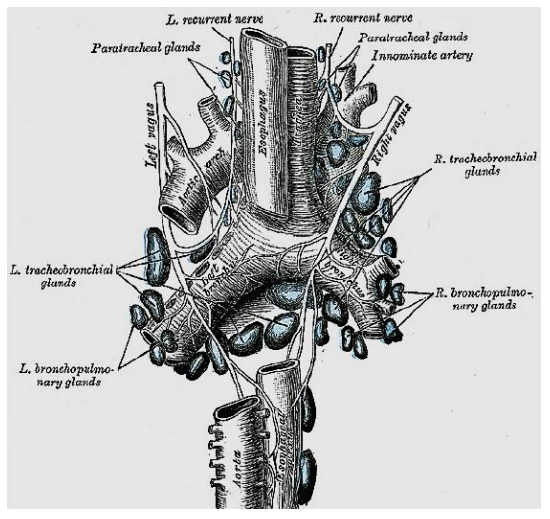
Figure 9: Posterior view of the course of the RLNs
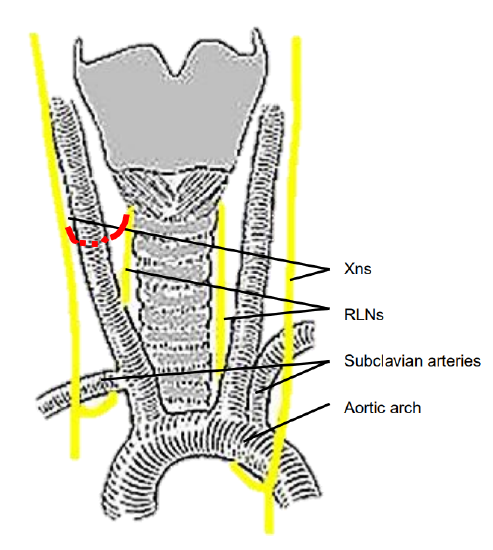
Figure 10: Typical anatomical course of RLNs (non-recurrent RLN in red)
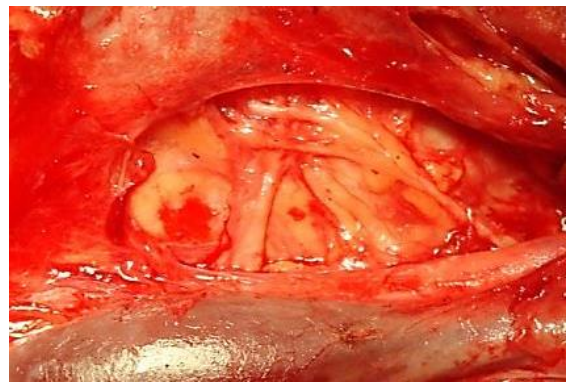
Figure 11: RLN passing over the inferior thyroid artery (right neck, thyroid reflected medially)
The majority of RLNs are located within 3 mm of Berry’s ligament; rarely the nerve is embedded in it, and more commonly lies lateral to it.
Classically, the RLN is identified intraoperatively in Simon’s triangle, which is formed by the common carotid artery laterally, the esophagus medially and the ITA superiorly (Figure 12).
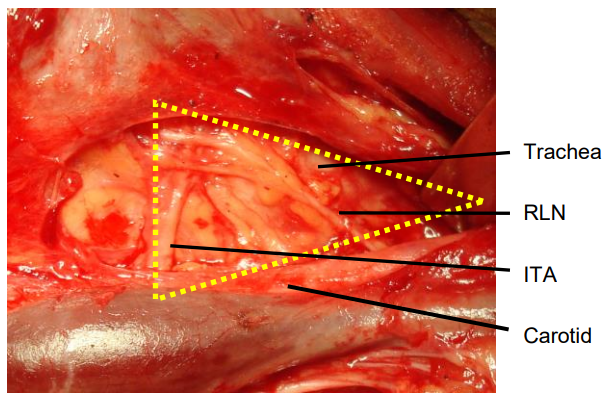
Figure 12: RLN crossing Simon’s triangle formed by trachea, ITA and common carotid artery
The Tubercle of Zukerkandl may also be used as an anatomical landmark to identify the nerve (Figure 4). The RLN generally courses between this structure and the trachea. However, this relationship can vary with enlargement of the tuberculum thereby placing the nerve at risk during surgical exploration.
Superior Laryngeal Nerve (SLN)
The SLN is a branch of the Xn and has both an external and internal branch (Figures 13, 14). The internal branch is situated above and outside the normal field of dissection; it is sensory and enters the larynx through the thyrohyoid membrane.
The external branch innervates the cricothyroid muscle, a tensor of the vocal cord. Injury to the SLN causes hoarseness, decreased pitch and/or volume, and voice fatigue. These voice changes are more subtle than those relating to RLN injury are frequently underestimated and not reported. The external branch is at risk because of its close proximity to the STA (Figures 13, 14). Understanding its relationship to the upper pole of the thyroid and the STA is crucial to preserving its integrity.
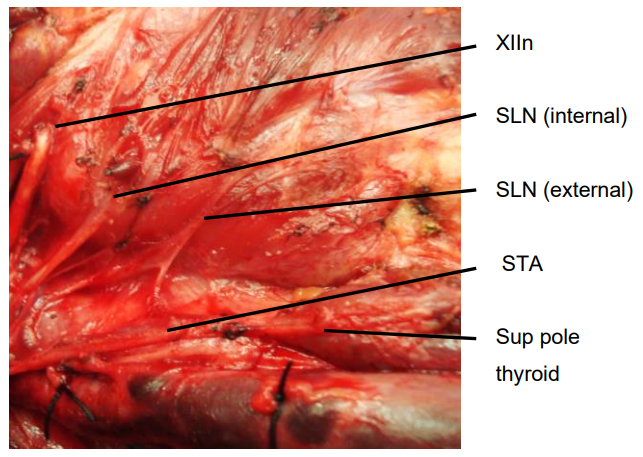
Figure 13: Anatomical relations of internal and external branches of right SLN to STA and to superior pole of thyroid
The usual configuration is that the nerve is located behind the STA, proximal to its entry into the superior pole of the thyroid. The relationship of the nerve to the superior pole and STA is however extremely variable. Variations include the nerve passing between the branches of the STA as it enters the superior pole of the thyroid gland; in such cases it is particularly vulnerable to injury.
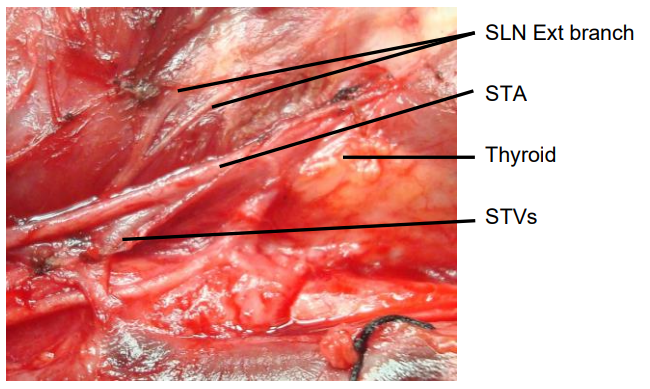
Figure 14: Note close proximity of external branch of SLN to STA and thyroid vein and to superior pole of thyroid gland
Types of parathyroidectomy
Focused parathyroidectomy: This is the usual procedure for a well-localised solitary adenoma. The offending gland is removed through a limited incision with direct exposure of the previously imaged parathyroid adenoma.
Bilateral neck exploration: In cases of unsuccessful preoperative localisation the surgeon explores the necks fully, identifies all four parathyroid glands and removes the adenoma.
Subtotal parathyroidectomy: This is indicated with parathyroid hyperplasia when all the glands have the capacity for increased parathyroid hormone (PTH) production. This occurs in secondary and tertiary hyperparathyroidism and in the unusual situation of primary hyperparathyroidism due to multiple gland hyperplasia. The three largest glands are removed and a small remnant of the most normal-looking gland is either left in situ or transplanted to an ectopic site, typically the forearm.
Total parathyroidectomy: All parathyroid tissue is removed. This may be done as a salvage procedure in cases of recurrent secondary hyperparathyroidism.
Preoperative evaluation: Primary hyperparathyroidism
Endocrine diagnosis: The diagnosis of primary hyperparathyroidism hinges on identifying an inappropriately raised PTH assay in the presence of elevated serum calcium. It is not unusual for hypercalcaemia symptoms of primary hyperparathyroidism to be non-specific and vague; hence it is often underestimated. Typical presentations include recurrent renal calculi, progressive bone density loss, pathological fractures, ill-defined musculoskeletal complaints, neurocognitive impairment, and unexplained abdominal pain; or it may present as a hypercalcemic crisis. While the diagnosis of primary hyperparathyroidism is not difficult to make for surgeons well versed in endocrine disorders, the occasional parathyroid surgeon is well advised to consult an endocrinologist prior to proceeding with surgery.
SestaMIBI scan: This is a nuclear medicine imaging technique with the highest sensitivity and specificity for identification of primary hyperparathyroid adenomas and is the authors’ investigation of choice. The use of Technetium99m (Tc99m) sestamibi for parathyroid imaging has led to a steady refinement of imaging. The accuracy is determined by the scanning technique employed; the dual-isotope (I123/ Tc99m sestamibi) scan provides better accuracy than the simpler sestamibi washout method. The pathological parathyroid can be localised preoperatively with great confidence allowing for a quicker and more focused neck exploration. Recent data would suggest that the combination CT99mTc-sestamibi-SPECT (reported sensitivity and specificity of up to 88% and 99% respectively) is the best approach for preoperative localisation with single gland disease. Unfortunately, these favorable results do not apply to all patients with parathyroid disease. It is important to note that failed localisation does not exclude primary hyperparathyroidism and is not a contraindication for surgical exploration.
Ultrasonography (US): The thyroid and surrounding structures can be evaluated with US. It has gained popularity due to the ease of the technique; many endocrine surgeons have the expertise to evaluate the neck in their own offices. Resolution has improved with newer generation equipment. The weaknesses of US are similar to 99mTc-sestamibi i.e. deep superior glands, ectopic glands and too-small glands are difficult to localise, and the mediastinum is inaccessible.
CT and MRI: CT and MRI are not indicated as first line investigations, but may be useful to evaluate parathyroid adenomas with non-localizing imaging studies or previously operated necks.
Preoperative evaluation: Secondary hyperparathyroidism
This diagnosis requires identification of an inappropriately raised PTH assay in the presence of an abnormally elevated serum phosphate-to-calcium ratio. The serum calcium typically falls within the normal range. Secondary hyperparathyroidism is almost always diagnosed in patients with chronic renal failure. Rarer causes include osteomalacia, rickets, and malabsorption. Secondary hyperparathyroidism contributes significantly to renal osteodystrophy and is associated with accelerated atherosclerosis, ectopic soft tissue calcification and skin ulcers in calciphylaxis. It contributes to a general feeling of malaise and musculoskeletal pain seen in chronic renal failure, and chronic pruritus. Close collaboration with a renal physician is essential to determine the best time for surgical intervention.
Preoperative consent
Scar: The incision is typically well-hidden within a natural skin crease of the neck but tends to descend with ageing.
Airway obstruction/wound haematoma: <1% of parathyroidectomy patients are stridulous postoperatively due to a haematoma, edema of the airway or injury to the RLNs.
Voice change: It is essential that the patient has a clear understanding of the risks relating to voice quality prior to surgery. While less common than with thyroidectomy, permanent RLN dysfunction does occur. The risk is highest with repeat surgery or with parathyroid carcinoma.
Hypocalcaemia: Transient hypocalcaemia occurs in approximately 20% of patients following successful removal of adenomas. Paradoxically the higher the levels of calcium and PTH preoperatively, the greater the postoperative drop in calcium. Most patients can be managed on oral calcium supplements until the remaining parathyroid glands re-equilibrate. Hypocalcaemia occurs in all cases of secondary hyperparathyroidism and requires proactive management with large doses of oral calcium supplements and Vitamin D1-α. Persistent symptoms require intravenous calcium supplementation.
Failed exploration: Some cases of hyperparathyroidism cannot be corrected surgically due to unusual pathology or failure to remove the pathological ectopic parathyroids; the risk of failed exploration is approximately 5%.
Anesthesia, positioning and draping
- General anesthesia with endotracheal intubation; local anesthesia is possible with confident preoperative localisation
- Prophylactic antibiotics are not required
- The neck slightly hyperextended by placing a bolster between the scapulae
- The head is stabilized on a head ring
- The table is tilted to 30º anti-Trendelenberg to reduce venous engorgement
- The head is free draped to allow turning of the head
Surgical technique
Because identification of parathyroid glands is reliant on subtle shades of colour and consistency, the recognition of parathyroid tissue can be impossible in a bloodied surgical field; meticulous haemostasis is therefore critical. Whilst parathyroidectomy is often simple and quick, it is not a procedure that can be rushed and should be booked early on an operating list to avoid undue pressure in terms of available operating time. The surgeon must be calm, unrushed and have a good assistant.
Skin incision: A curvilinear incision is placed in a skin crease approximately two finger breadths above the sternal notch between the medial borders of the sternocleidomastoid muscles (Figure 15). It is seldom necessary to make the incision longer than 4-5cm. Well-localized glands can be resected via a smaller incision. Placing the incision too low causes an unsightly low scar over the heads of the clavicles when the extended neck is returned to its normal position.
Subplatysmal flaps: Subcutaneous fat and platysma are divided, and a subplatysmal dissection plane is developed superiorly (platysma is often absent in the midline) remaining superficial to the anterior jugular veins, up to the level of the thyroid cartilage above, and the sternal notch below (Figure 16).
The skin flaps are secured with a fixed retractor (Figure 17).

Figure 15: Curvilinear skin incision two finger breadths above the sternal notch
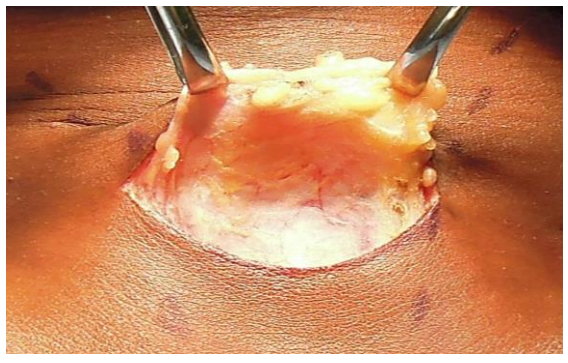
Figure 16: Subplatysmal flaps elevated
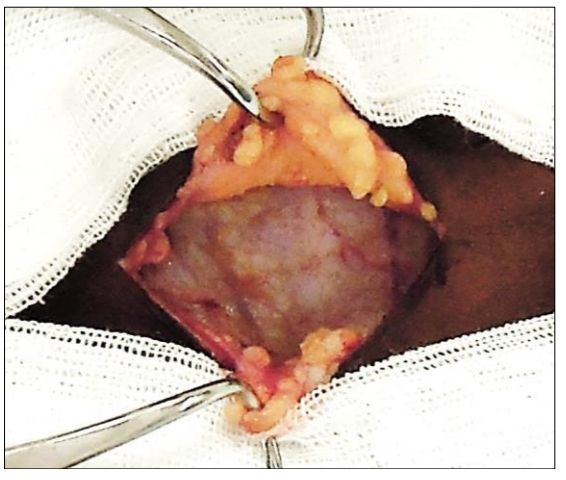
Figure 17: Subplatysmal skin flaps held with Jowell’s retractor. Note anterior jugular veins (AJVs)
Surgical Approaches
- Lateral approach involves dissecting along the medial border of the sternocleidomastoid muscle to the carotid sheath, and then medial to the sheath up to the thyroid region. This is employed in cases of confident preoperative localisation.
- Anterior approach involves medial mobilization of the thyroid gland. This is used in cases of possible bilateral neck exploration. It is favored by the author and is described in more detail below.
Separating strap muscles and exposing the anterior surface of thyroid: The fascia between the sternohyoid and sternothyroid muscles is divided in the midline with diathermy or scissors (Figure 18). This is an avascular plane, though care must be taken not to injure small veins occasionally crossing between the anterior jugular veins, particularly inferiorly. The infrahyoid (sternohyoid, sternothyroid and omohyoid) strap muscles are retracted laterally with a right-angled retractor. In difficult cases the strap muscles may be divided to improve access.
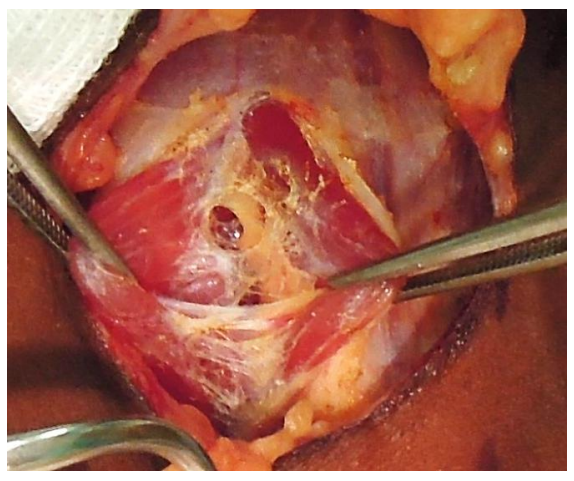
Figure 18: Fascia between sternohyoid and sternothyroid muscles divided to expose thyroid gland
It is usual at this stage for the surgeon to move to the side of the table opposite to the parathyroid to be resected.
Delivery of thyroid towards midline: The infrahyoid (sternohyoid, sternothyroid and omohyoid) strap muscles are retracted laterally with a right-angled retractor. The thyroid gland is delivered medially by applying gentle digital traction to the gland (Figure 19).

Figure 19: Medial rotation of (R) thyroid lobe exposes the middle thyroid vein
Division of middle thyroid vein(s): The vein is the first key vascular structure to be encountered and is tightly stretched by medial traction on the gland (Figure 19). Dividing the vein facilitates additional mobilization of the gland and permits delivery of the bulk of the thyroid lobe into the wound (Figure 20). Although dividing it is not always essential, it is better to do so than to risk tearing it.
If the surgeon is confident about preoperative localisation then dissection is next directed at the parathyroid adenoma.
Identifying superior parathyroid: Full mobilization and anterior delivery of the upper pole of the thyroid brings the region of the superior parathyroid gland into direct view.

Figure 20: Dividing the middle thyroid vein
The superior parathyroid gland is normally located in a posterior position at the level of the upper two-thirds of the thyroid and is closely related to the Tubercle of Zuckerkandl; it is about 1cm above the crossing point of the RLN and ITA. If the RLN’s course is viewed in a coronal plane, then the superior parathyroid gland lies deep (dorsal) to the plane of the nerve (Figures 4, 6, 7). It has a characteristic rich orange/ yellow color (Figures 21, 22). The (occasional) para-thyroid surgeon may find the parathyroids difficult to identify especially if there has been bleeding in the surgical field, so care must be taken to ensure meticulous haemostasis.
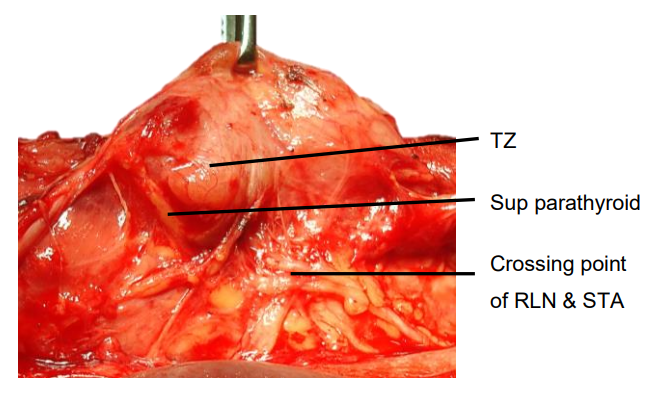
Figure 21: Position of superior parathyroid relative to Tubercle of Zuckerkandl (TZ), RLN and STA
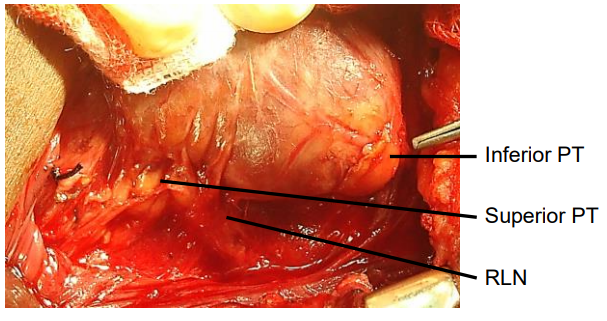
Figure 22: Superior and inferior parathyroids (PT)
The gland must remain in situ with blood supply intact. This is best achieved by carefully dissecting it off the posterior aspect of the thyroid gland and using short bursts of bipolar cautery to control bleeding. If the gland still cannot be identified, it is prudent to divide the STA and completely mobilize the upper pole of the thyroid. This will almost certainly bring the superior parathyroid into view.
Identification of inferior parathyroid: The inferior gland is initially looked for at the inferior aspect of the lower pole of the thyroid or within the thyrothymic ligament. If the RLN’s course is viewed in a coronal plane then the inferior parathyroid is superficial (ventral) to the plane of the nerve (Figures 6, 7, 21, 22). Its location is more varied than with the superior gland, but if it is at its expected location then it is generally simpler to identify. The inferior parathyroids are most commonly located between the lower pole of the thyroid and thyroid isthmus, most commonly on the anterior or posterolateral surfaces of the lower pole of the thyroid (42%, Wang et al), or may be located in the lower neck in proximity to the thymus (39%). Preserving it in situ avoids damaging the ITA blood supply.
Removal of adenoma: (Figures 23, 24) Once the abnormal parathyroid has been identified, it is removed. Parathyroid tissue can autotransplant if fragmented, so great care is taken to deliver an intact gland by delicately grasping its capsule until the vascular pedicle is identified. This is then be ligated with a 3/0 tie.
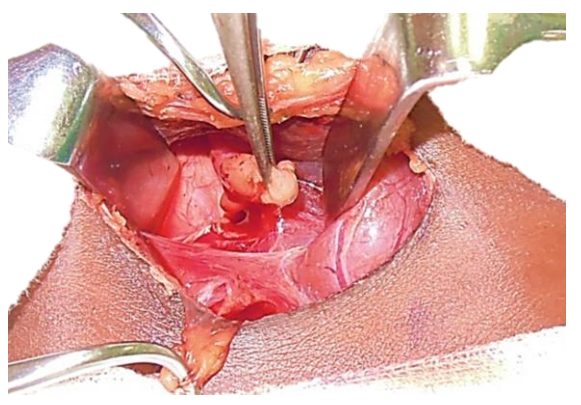
Figure 23: Right superior parathyroid adenoma being removed
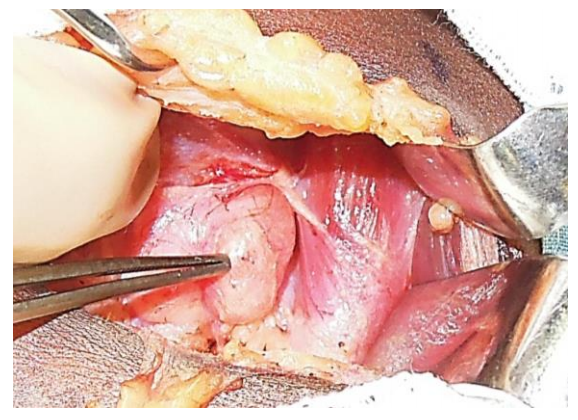
Figure 24: Right inferior parathyroid adenoma
Confirming successful removal: After identifying the parathyroid glands, it is essential to distinguish between normal and pathological glands. Simple rules of thumb are that increased size correlates with pathology, and that marked elevations of calcium and PTH levels are usually caused by larger adenomas. Adenomas are typically more rounded than normal parathyroid glands and have a darker, fleshy parenchymal appearance, sometimes described as similar to a “rat’s heart”. They are typically 1-2 cm in diameter and are significantly heavier than normal glands (Figure 25). Occasionally small adenomas (<1 cm) and very large ones (up to 8 cm) are found (Figure 1).

Figure 25: Typical parathyroid adenomas
The occasional parathyroid surgeon is well advised to confirm that abnormal parathyroid tissue has been removed as it is easy to mistake fat, lymph gland, thymus, a superficial thyroid nodule, or normal parathyroid for an adenoma, particularly if the dissection has been difficult. This can be done in two ways:
- Routine frozen section histology. Distinguishing between parathyroid and other tissue is quick and simple to do; but it is not good for differentiating between normal parathyroid, hyperplastic parathyroid or adenoma.
- Rapid intraoperative PTH assays (ioPTH) allow endocrine surgeons to record an immediate drop of PTH level as an accurate marker of surgical cure of hyperparathyroidism because of the short half-life of PTH. A large-bore peripheral IV line is used to draw blood for ioPTH levels both prior to (baseline) and following excision of the adenoma. From the time the blood is drawn, the assay takes approximately 15 minutes. It is essential to measure PTH levels as soon as possible to the time of resection of the adenoma as PTH measurements are labile and likely position dependent. A commonly used criterion for curative resection is a 50% drop in ioPTH levels (compared with baseline) at 5, 10, and 15 min following resection; a persistently elevated ioPTH indicates inadequate cure and necessitates further exploration. It requires access to a rapid ioPTH assay machine which should ideally be located in/ close to the operating room to avoid unnecessary delays.
The missing gland: Most parathyroid operations are simple, quick and rewarding for both surgeon and patient. However, on occasion parathyroid glands may be infuriatingly difficult to identify and tests the skill and patience of even the most experienced endocrine surgeon. Surgery is likely to be more complex in the following situations and the occasional parathyroid surgeon should consider referring such cases to an expert:
- Normocalcaemic hyperparathyroidism
- Failed/discordant preoperative localisation imaging
- Concomitant, large multinodular thyroid disease
- Failed previous exploration
- Family history suggestive of MEN syndrome
If exploration fails to reveal convincing evidence of a parathyroid adenoma, then two likely scenarios apply:
- All 4 parathyroids have been found, but none looks convincingly pathological: it is probable that the patient has four-gland hyperplasia, and a subtotal parathyroidectomy is indicated. Frozen section is invaluable to confirm that removed tissue is truly parathyroid tissue
- If 3 normal-looking glands have been identified it is probable that the missing gland is the adenoma and a more exhaustive search is required
A missing superior parathyroid gland is almost always located where it is meant to be i.e. in its normal position at the level of the upper two-thirds of the thyroid, in a posterior position, about 1 cm above the point where the RLN crosses the ITA. The surgeon needs to further mobilise the upper pole of the thyroid anteriorly. The parathyroid may be covered by a fine layer of thyroid capsule; dissecting onto the thyroid parenchyma itself may release it and bring it into view. Should it still not be visible one then needs to transect the STA to fully mobilize the upper pole. If it still cannot be located, then one may be dealing with the rare situation of ectopic retro-esophageal and retropharyngeal locations and these regions need to be explored.
A missing inferior parathyroid gland poses more of a challenge as the anatomical variations are greatest. The following areas need to be systematically explored:
- Lower pole of thyroid.
- Thyrothymic ligament
- Simon’s triangle, just below the ITA
- Thymectomy by applying traction to the thyrothymic ligament
- Lateral cervical space, behind the carotid sheath towards the posterior mediastinum
- Carotid sheath
- Retro-esophageal space
If this still fails to identify pathological glands it is then reasonable to abandon the procedure and to consider secondary exploration after more exhaustive imaging 6-12 months later.
Wound closure
- Irrigate the wound
- Do a Valsalva manoeuvre and check for bleeding
- Wound drainage is not routinely required
- Approximate the strap muscles in the midline along 70% of their lengths
- Close the platysma layer with interrupted absorbable 3/0 sutures
- Skin closure is achieved with a subcuticular absorbable monofilament suture
- A light dressing is applied
Postoperative care
- Keeping thorough records is invaluable in cases of recurrent hyperparathyroidism. Therefore, keep meticulous and detailed notes about the extent of the exploration noting which normal parathyroid glands were seen, precisely where they were located and what tissue was removed
- The intravenous line is removed, and a normal diet is taken as tolerated
- Following successful focussed parathyroidectomy the patient may be discharged the same day
- More complex cases are monitored overnight for bleeding or airway obstruction
- Serum PTH levels are routinely measured 24 hours postoperatively. A return to normal PTH levels confirms a successful operation. A hypocalcemic trough occurs 2-5 days postoperatively. Calcium and Vitamin D1α are commenced pre-emptively if the PTH reading is low
Specific Scenarios
Secondary hyperparathyroidism: Up to 90% of patients meeting criteria for haemodialysis have secondary hyperparathyroidism. Surgery is indicated for:
- Calciphylaxis
- Patient preference
- Medical observation not possible
- Failure of maximum medical therapy with persistent hypercalcaemia, hypercalcuria, PTH >800pg/mL and hyperphosphataemia
- Osteoporosis
- Progressive symptoms e.g. pruritus, pathologic bone fractures, ectopic soft tissue calcification, severe vascular calcification, and bone pain
Three different surgical procedures involving bilateral neck exploration are employed for patients with secondary hyperparathyroidism who fulfill criteria for surgery. Each operation has its proponents and an institutional history. There is no convincing evidence of superiority of any one approach:
- Subtotal parathyroidectomy i.e. removing 3½ glands and leaving a ½-gland remnant in situ (author’s preference)
- Total parathyroidectomy (four-gland resection) with autotransplantation
- Total parathyroidectomy (four-gland resection) without autotransplantation
Repeat surgery for failed exploration: Such cases should be managed by surgeons well-versed in the subtleties of parathyroid surgery. The following issues need to be carefully considered before embarking on expensive investigations and repeat surgery:
- Is the diagnosis of primary hyperparathyroidism correct, or is there an alternative explanation for the endocrine abnormalities?
- Differentiate recurrent parathyroid disease from persistent hyperparathyroidism: did PTH levels drop following the 1st operation, or did they remain elevated?
- Obtain surgical notes of the primary procedure, histology reports, and postoperative endocrinology records
If a convincing case can be made for reexploration, then the most helpful imaging remains Tc 99m-sestamibi and cervical US. If both are negative, then a CT-scan may add useful information. Whilst potential ectopic locations of parathyroids should be considered, most missed parathyroid glands are located within the cervical region. Repeat neck exploration for persistent or recurrent disease can be very difficult as the normal tissue planes are scarred and it is associated with higher rates of injury to the RLN and permanent hypoparathyroidism. The lateral or ‘‘backdoor’’ approach (dissection between the anterior border of the sternocleidomastoid muscle and posterior border of the strap muscles) may be useful as it provides direct access to the posterior surface of the thyroid gland without encountering scar tissue from previous surgery done through the conventional anterior approach.
Radioguided parathyroidectomy: This technique may be helpful with complex repeat surgery, but the author does not use it for routine parathyroidectomy due to cost and logistic constraints. It is similar to other radioguided techniques such as sentinel lymph node biopsy. A parathyroid-specific radiotracer such as Tc99msestamibi is administered intravenously approximately 2 hours prior to surgery; this time delay allows for a high concentration of isotope to be retained within the parathyroid adenoma whilst it has started to wash out from other sites of uptake such the salivary glands and thyroid. A gamma camera is used intra-operatively to identify the adenoma.
Minimally invasive parathyroid surgery: Several techniques have been devised to reduce the length of the skin incision and to bring the putative benefits of minimally invasive techniques to thyroid and parathyroid surgery. Minimally invasive parathyroidectomy can be performed via a limited 2-3cm cervical incision with visual assistance of an endoscope, but since it can be performed with a similarly sized incision with direct visualization, this technique is not widely used.
Useful References
- Mohebati A, Shaha AR. Anatomy of Thyroid and Parathyroid Glands and Neurovascular Relations. Clin Anat. 2012;25(1):19-31
- Wang C. The anatomic basis of parathyroid surgery. Ann Surg. 1976; 183: 271–5
- Fraser WD. Hyperparathyroidism. The Lancet. 2009;374:145–58
- Adler JT, Sippel RS, Chen H. New Trends in Parathyroid Surgery. Curr Probl Surg. 2010;47(12):958-1017
- Lew JI, Solorzano CC. Surgical Management of Primary Hyperparathyroidism: State of the Art. Surg Clin N Am. 2009;89:1205–25
- Pitt SC, Sippel RS, Chen H. Secondary and Tertiary Hyperparathyroidism: State of the Art Surgical Management. Surg Clin N Am. 2009;89:1227–39
Thyroidectomy under local and regional (cervical plexus block) anesthesia
https://vula.uct.ac.za/access/conten...naesthesia.pdf
Author
Eugenio Panieri MBChB, FCS
Associate Professor
Division of General Surgery
University of Cape Town
Cape Town, South Africa
eugenio.panieri@uct.ac.za
2nd Author and Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


