4.10: Rhinoplasty Basic Approaches and Techniques in Nasal Tip Surgery
- Page ID
- 49378
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
RHINOPLASTY: BASIC APPROACHES AND TECHNIQUES IN NASAL TIP SURGERY
GJ Nolst Trenité
The variety of procedures for nasal tip surgery and the individual differences in tip anatomy are complicated by the confusing terminology in the international literature. It was Tardy who advocated a systematic rational approach to the nasal tip. With this framework in mind, the inexperienced nasal surgeon can use the appropriate incisions, approaches and techniques more easily. The basic philosophy is to operate as atraumatically as possible and to preserve tip support, which is very important in getting good long term postoperative results.
There are three basic surgical approaches to the tip of the nose:
1. Non-delivery approach
- Cartilage-splitting
- Retrograde eversion
2. Delivery approach
3. External approach
Indications for each of these approaches depend on the specific anatomy of the nose and the proposed changes:
- Volume reduction
- Reconstruction
- Rotation
- Change of projection
Surgical Procedures
1. Non-delivery approach The non-delivery approach is very appropriate for:
- Small volume reduction of the lateral crus
- Slight cephalic rotation of the tip
Volume reduction can easily be done using a transcartilaginous incision, in which only slight surgical trauma occurs.

Figure 1: Drawing of the skeletal landmarks and the planned resection on the skin
The operative procedure for the cartilage splitting non-delivery approach is as follows: after drawing the skeletal landmarks and boundaries on the skin of the nose, the most cephalic part of the lateral crus to be resected is outlined with a marking pen on the external skin (Figure 1).
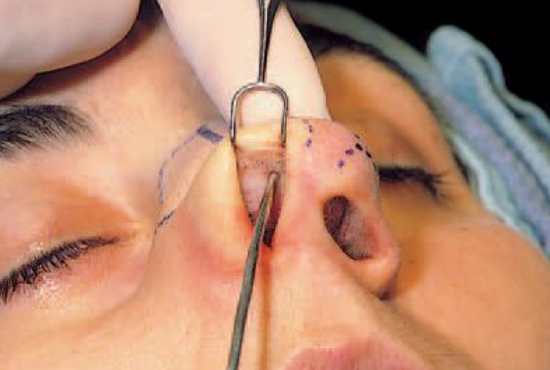
Figure 2a: Imprint of the vestibular skin with a suction tube to mark the planned site of the transcartilaginous incision

Figure 2b: Suction tube imprint of the vestibular skin (arrow)
It is helpful to indicate on the vestibular skin where the transcartilaginous incision should be made. This can be done either by a through-and-through needle from the outside or, more elegantly, by using the imprint of a surgical instrument on the vestibular skin (Figures 2a,b).
Care should be taken to preserve at least 5 mm of uninterrupted cartilage (in a vertical dimension) of the lateral crus.

Figure 3: Vestibular skin incision
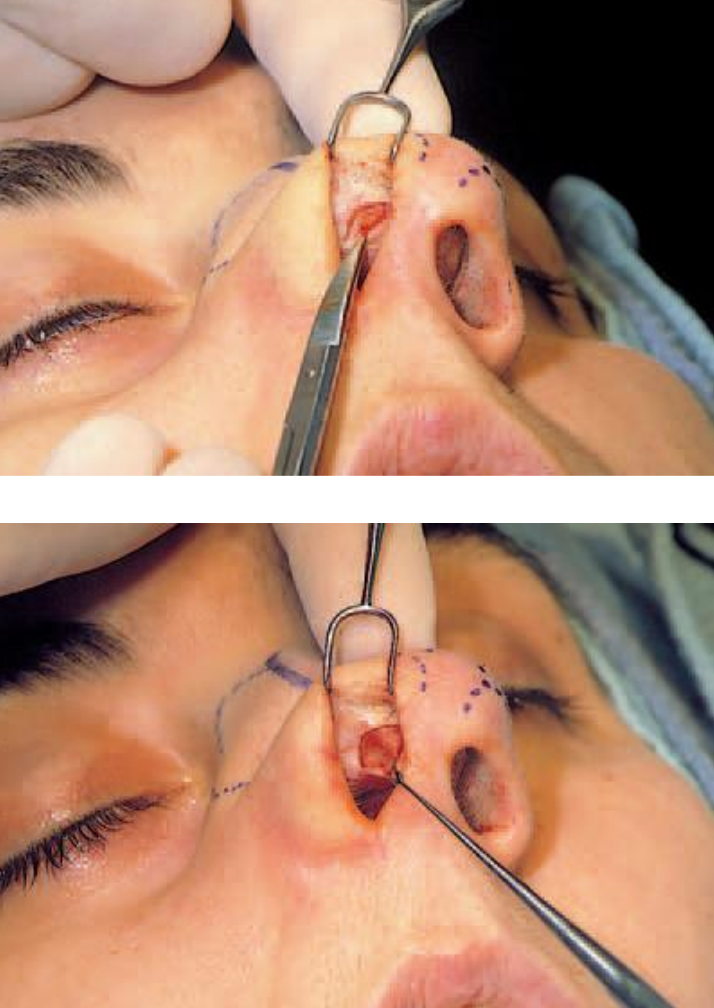
Figures 4a,b: The vestibular skin is dissected free from the cephalic part of the lateral crus to be resected
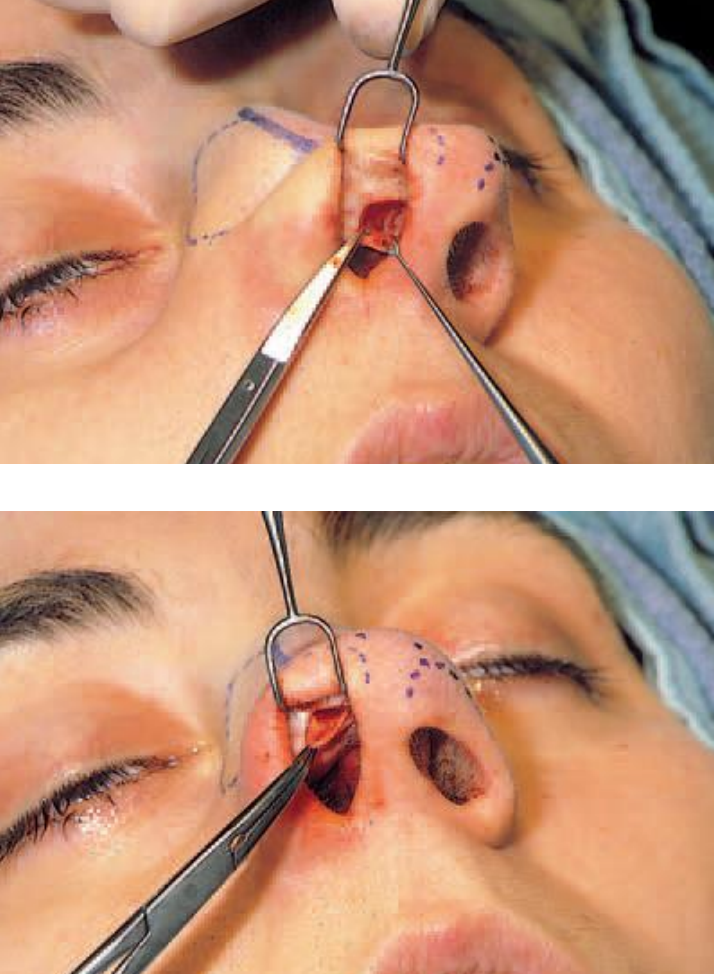
Figure 5a,b: Dissection at the nonvestibular site after splitting the cartilage

Figures 5c,d: Resection of cephalic parts of the lateral crura
Although many surgeons make their incisions through the vestibular skin and cartilage at once, it facilitates the dissection of the vestibular skin to do this in two stages. A vestibular skin incision with a No. 15 blade (Figure 3) is followed by dissecting the vestibular skin free from the proposed resection of the cephalic part of the lower lateral cartilage with a pair of sharp pointed curved scissors (Figures 4a,b). After splitting the cartilage (No. 15 blade), the nonvestibular side of the cephalic part to be resected is dissected free from the overlying soft tissue and removed (Figures 5a-d). Pressure of the middle finger of the operator’s hand (holding the double-hooked ala retractor) on the lateral crus will give excellent exposure and control during surgery.
After sufficient and symmetric volume reduction, the vestibular skin should be sutured carefully with 5/0 atraumatic absorbable suture material. This simple tip refinement procedure gives minimal surgical trauma, leaving the integrity of the lower lateral intact ensuring the best chances for uncomplicated healing process.
Nowadays, the retrogade-eversion approach is performed less often. Instead of a transcartilaginous incision, an intercartilaginous incision is made followed by retrograde dissection over the lateral crus at the non-vestibular side, eversion of the lateral crus and resection of the planned cephalic portion of the cartilage.
2. Delivery approach
The delivery approach, although more traumatic, is indicated when the planned changes to the nasal tip are more than just a small volume reduction.
The indications for this approach are:
- Asymmetry
- Bifidity
- Extra cephalic tip rotation
- Diminishing of the tip projection
With this approach, it is possible to modify the alar cartilages under direct vision up to the dome and interdomal area. Different operative techniques can be applied:
- Precise excision of cartilage to achieve good symmetry
- Remodeling the alar cartilages by scoring and morcellation
- Interdomal suturing to correct bifidity
- Interruption of the continuity of the alar cartilage to reduce an extremely overprojected tip (‘pinocchio’ nose) or to enhance cephalic tip rotation.

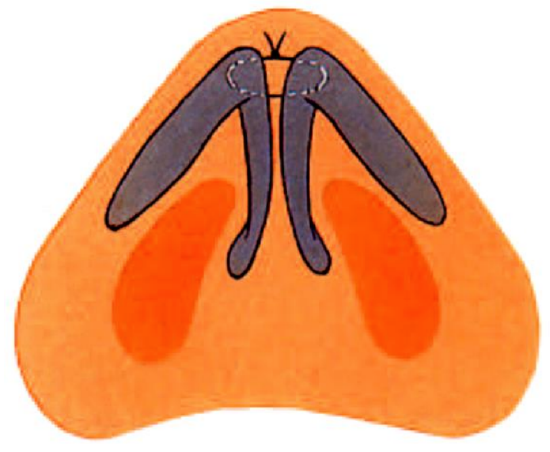
Figure 6: Intercartilaginous incision caudal to the valve area and around the anterior septal angle
The surgical procedure to deliver the alar cartilages starts with an intercartilaginous incision with a No. 15 blade. It is important to make this incision caudally to the valve area to prevent unnecessary scarring in the valve area. This intercartilaginous incision should be carried well around the anterior septal angle (Figure 6). If not, delivery could be stagnated.

Figure 7: Marginal incision
The next step is to make a marginal incision (No. 15 blade), hugging the caudal edge of the lower lateral to prevent surgical damage to ‘the soft triangle’. The incision starts at the upper part of the caudal edge of the medial crus, then goes around the dome and follows the caudal edge of the lateral crus as far as necessary (Figure 7).
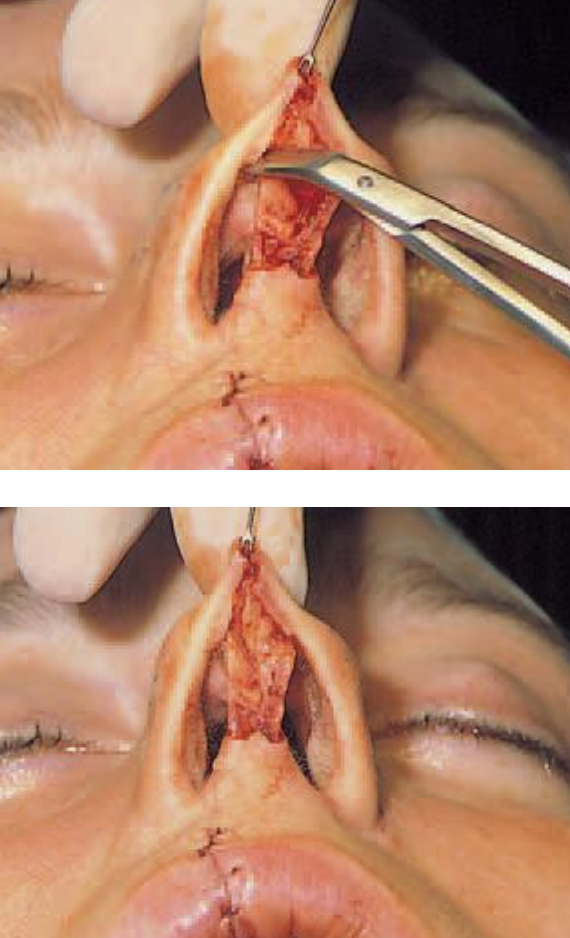
Figures 8a,b: Precise dissection and excision of a cephalic portion of the lateral crus
After these two incisions, the non-vestibular side of the lateral crus is freed from the soft tissue by dissection with a pair of sharp pointed curved scissors. To deliver the bipedicled chondrocutaneous flaps, small hemostats are very handy. Precise excision of cartilage is now possible under direct vision (Figures 8a,b).
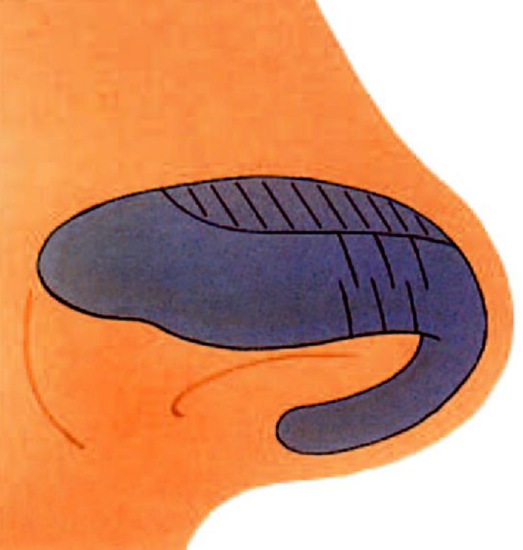
Figure 9a: Weakening procedure of the lateral crus by scoring the cartilage
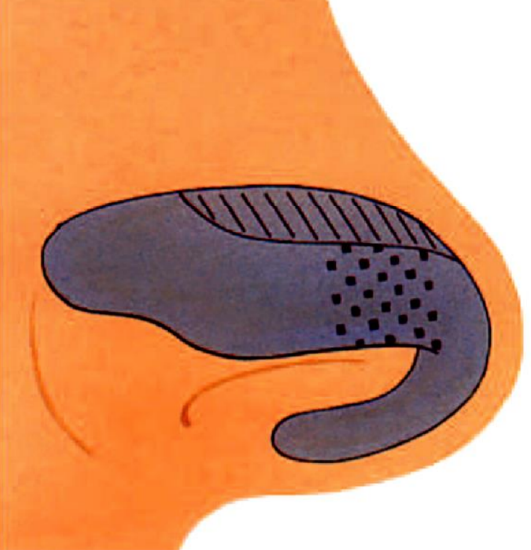
Figure 9b: Weakening procedure of the lateral crus by morcellation
In the case of bulging of the lateral crus, the weakening procedure (scoring or morcellation) is performed, if indicated in combination with resection of a cephalic portion of the lateral crus (Figures 9a,b).

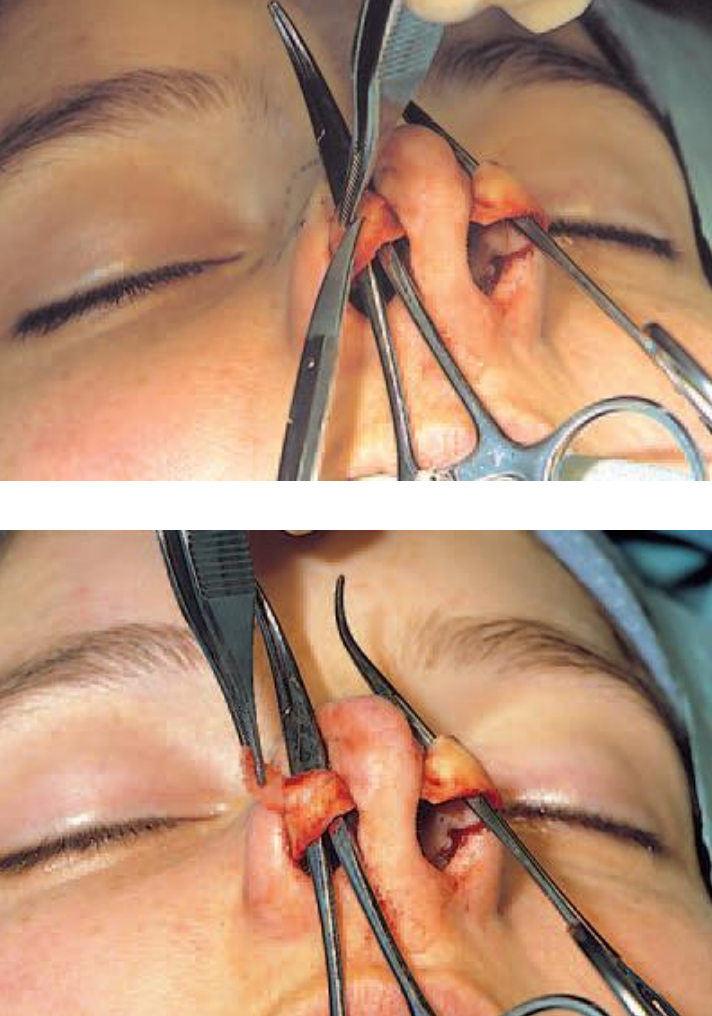
Figures 10a, b: Horizontal mattress suture technique to correct bifidity of the tip
Figures 10 c,d: Mattress suture with 6/0 Goretex of left lower lateral followed by transportation of the needle with a mosquito clamp to the right side for the same procedure

Figure 10e: Direct postoperative result after advancing the domes with horizontal mattress suture technique
The delivery approach is also appropriate in the case of bifidity of the nasal tip, in which the horizontal mattress suture technique can be performed to advance the domes with a non-absorbable (Goretex) or a slow absorbable (PDS) atraumatic suture (Figures 10a-e).
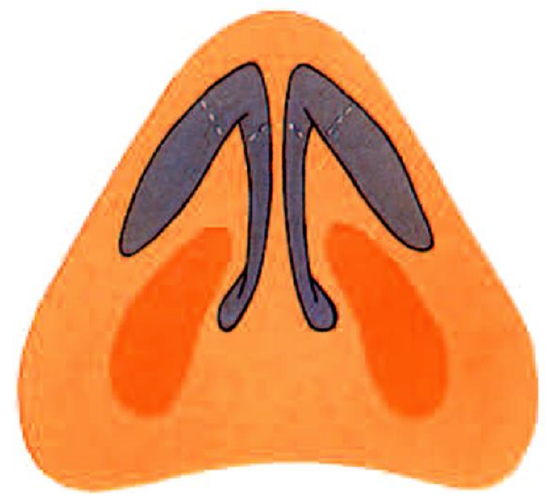
Figure 11a: Dome amputation

Figure 11b: Sutured lower laterals with an onlay tip graft to hide possible postoperative irregularities
Interrupting the continuity of the alar cartilage can give some unpredictable scarring, especially visible in thin-skinned noses. In the case of dome amputation to reduce a ‘pinocchio’ nose, an onlay tip graft will hide possible irregularities in the healing process (Figures 11a,b).

Figures 12a,b: Interrupted strip technique to obtain adequate cephalic tip rotation in case of a tension nose
To reduce tip projection and to obtain sufficient cephalic tip rotation, as is indicated in correcting a tension nose, the continuity of the alar cartilage is interrupted by transection of the lateral crus at the junction of its middle and lateral third, followed by resection of the cartilage segment of the lateral third and cephalic part (Figures 12a,b).
A supplementary procedure to enhance tip rotation is resection of a caudal strip of cartilage in the septum. The surgeon should be aware that the healing process is less predictable, with more chance of postoperative asymmetries, with the delivery approach than with the non-delivery approach.
3. External approach
The external approach, although even more traumatic and time consuming, gives the best exposure of the three approaches. This approach enables the surgeon to perform bimanual surgery, and it makes judgement of the specific deformities much easier. Therefore, it is especially indicated in the case of:
- Congenital deformities such as cleft, lip nose
- Extensive revision surgery
- Severe nasal trauma
- Elaborate reduction and augmentation procedures
Nevertheless, there is a tendency to use the external approach routinely, especially by less experienced nasal surgeons. This is justified as long as the surgeon weighs the surgical trauma of the chosen approach against the possibilities of a satisfying postoperative result in each individual case.
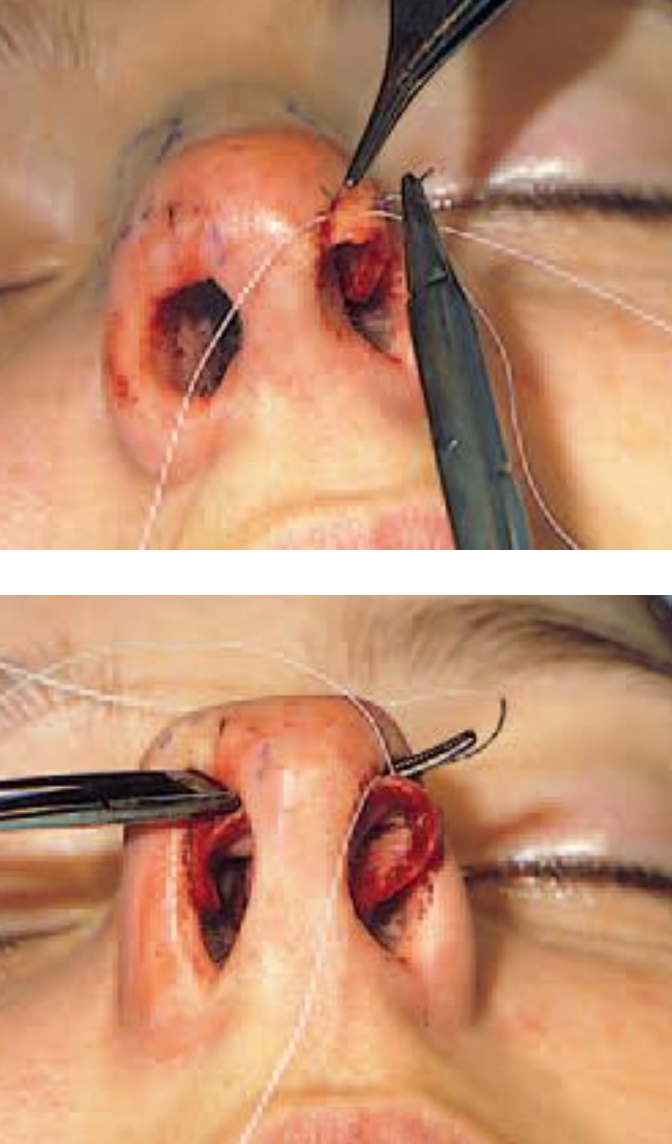
Figures 13a,b: External approach after careful preparation of the columella skin flap avoiding injury to the underlying cartilage of the medial crura

Figure 14: Meticulous suturing of the midcolumellar incision with 6/0 nylon
Careful preparation of the columella skin flap (Figures 13a,b), without disturbing the underlying cartilage of the medial crura, and meticulous suturing of the midcolumellar skin incision (Figure 14), to prevent skin necrosis and visible scarring, are prerequisites.
Clinical examples
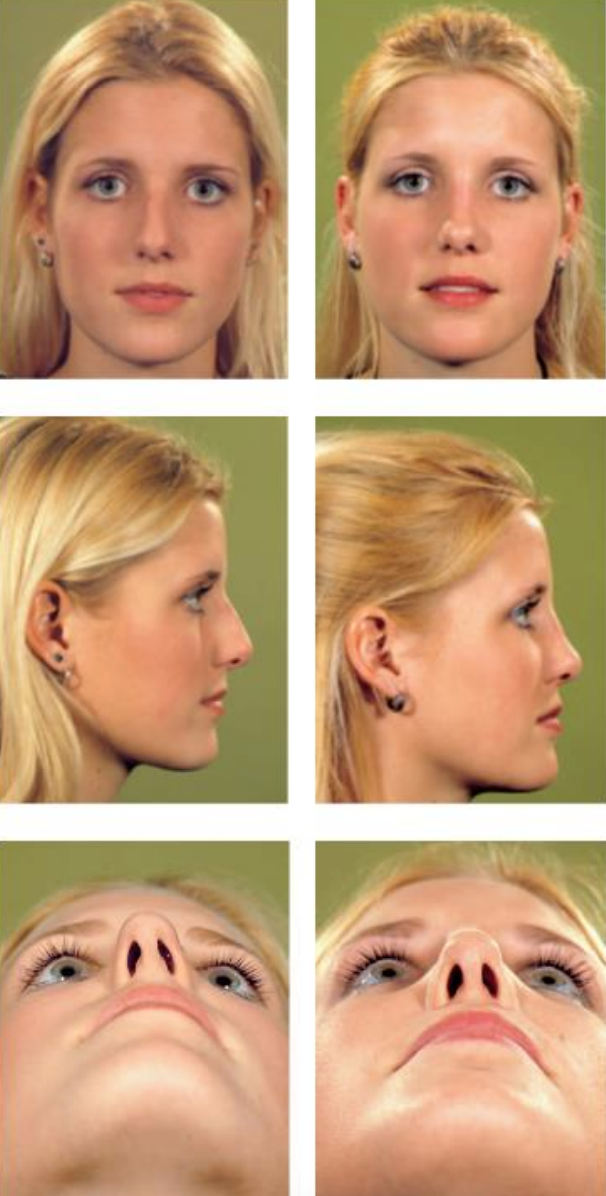
Figure 15: Pre- (left) and postoperative (right) views of a patient who underwent a rhinoplasty by the non-delivery approach. First a septoplasty was performed to correct a caudal septal deviation to the left followed by a cephalic resection of the lower laterals. Then a cartilaginous bony hump was removed followed by medial oblique, lateral micro-osteotomies and infracture of the nasal bones
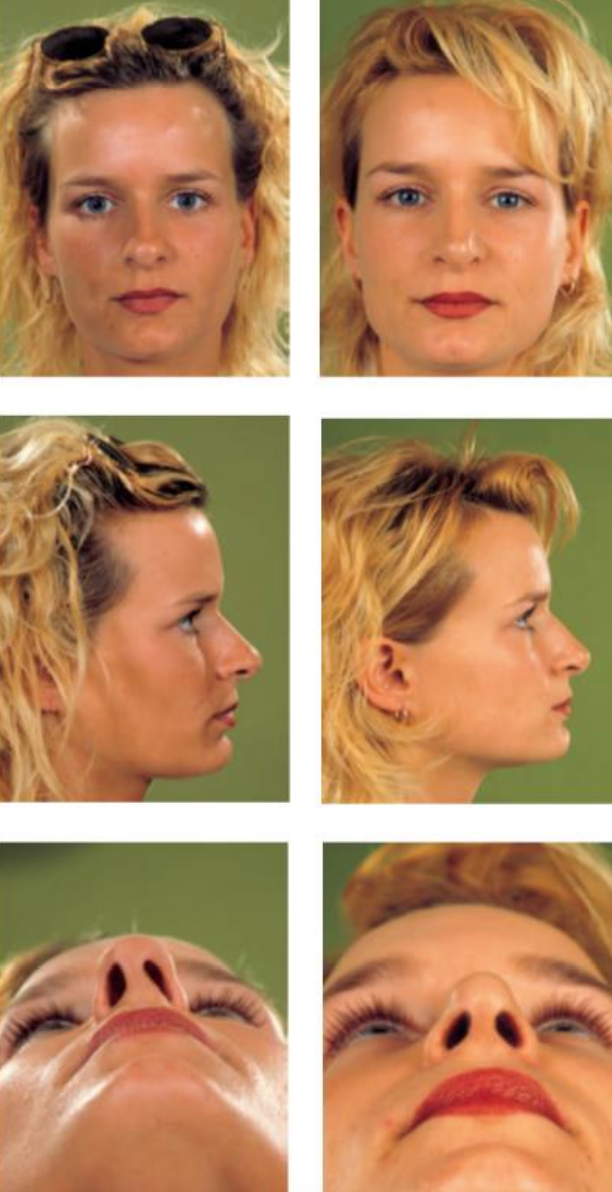
Figure 16: Pre- (left) and postoperative (right) views of rhinoplasty by the delivery approach, to narrow the broad trapezoid tip with transdomal and interdomal suturing followed by a bilateral cephalic resection of the lower laterals and a small resection of the cartilaginous dorsum. The asymmetry of the nostrils due to a caudal septal deviation to the left was corrected by a septoplasty through a hemitransfixion incision
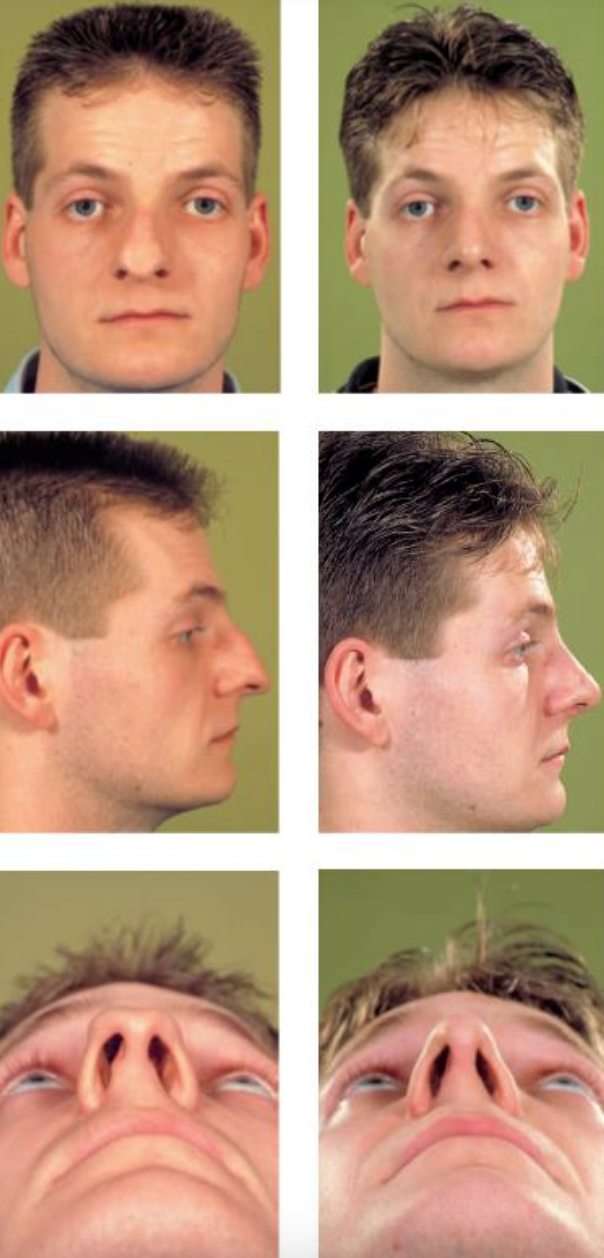
Figure 17: Pre- (left) and postoperative (right) views of a patient with a congenital deformity of the nose with agenesis of the nasal bones, overdevelopment of the cartilaginous vault and an extreme trapezoid deformity of the nasal tip. Narrowing of the tip with inter- and transdomal suturing and adequate cephalic tip rotation was performed with an interrupted strip technique through an external approach. Finally alar base wedge resections were performed to correct alar flaring
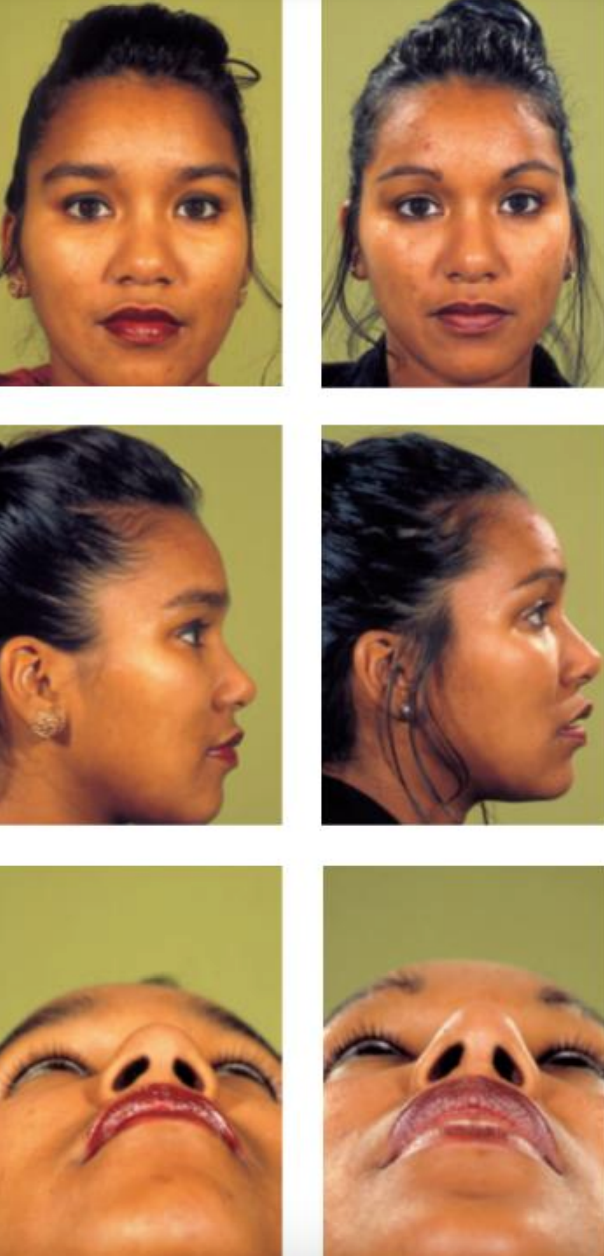
Figure 18: Pre- (left) and postoperative (right) views of a patient with a bulbous tip with lack of projection. An external rhinoplasty was performed for more tip projection and refinement with the use of autogenous grafts (columella strut and shield graft) from septal cartilage
In Figures 15-18 clinical cases of nondelivery, delivery and external approaches are shown.
The material in this chapter originates from the textbook “Rhinoplasty: A practical guide to functional and aesthetic surgery of the nose” G.J. Nolst Trenité (ed) ISBN 978-90-6299-206-5 https://www.rhinoplasty.nl/store/
Author
Gilbert Nolst Trenité MD, PhD
Professor of Otorhinolaryngology
Former President of European Academy of Plastic Surgery
Amsterdam, Netherlands
nolsttrenite@gmail.com
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


