5.6: Exercise, Nutrition, Hormones, and Bone Tissue Health
- Page ID
- 63393
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
- Describe the effect exercise has on bone tissue
- Discuss the role nutrients play in bone health
- Describe the effects of hormones on bone tissue
- Explain how the structure of bone is affected by insufficiencies in exercise, nutrients, and hormones.
All of the organ systems of your body are interdependent, and the skeletal system is no exception. The food you take in via your digestive system and the hormones secreted by your endocrine system affect your bones. Even using your muscles to engage in exercise has an impact on your bones.
Exercise and Bone Tissue
Functions of bone are to provide support for the body by providing a framework that resists outside forces such as gravity and provides solid anchoring points for muscles to pull against to cause movement. Applying these stressors on the bone tissue cause our osteoblasts to build matrix in order to provide sufficient resistance. The two mays in which bone structure adapts to such forces are to alter the thickness of the cortical (surface) compact bone and to align the trabeculae in the cancellous bone. The trabecular pattern of growth follows the course of stress lines along the bone and the thickest trabeculae develop along the lines of maximum stress.
If the stressors on a particular bone increase, then the bone will remodel itself to become stronger and resist the new load. Increased stressors could be carrying more weight (either by increasing body mass or carrying external weight, such as a backpack), increases the amount of weight-bearing activities, and strengthening muscles. The opposite will also happen if such stressors decrease: the bone will remodel itself to removed un-needed matrix. The proximal femur in Figure \(\PageIndex{1}\) below shows these lines of tension and compression.

Skeletal System
|
During long space missions, astronauts can lose approximately 1 to 2 percent of their bone mass per month. This loss of bone mass is thought to be caused by the lack of mechanical stress on astronauts’ bones due to the low gravitational forces in space. Lack of mechanical stress causes bones to lose mineral salts and collagen fibers, and thus strength. Similarly, mechanical stress stimulates the deposition of mineral salts and collagen fibers. The internal and external structure of a bone will change as stress increases or decreases so that the bone is an ideal size and weight for the amount of activity it endures. That is why people who exercise regularly have thicker bones than people who are more sedentary. It is also why a broken bone in a cast atrophies while its contralateral mate maintains its concentration of mineral salts and collagen fibers. Bones undergo remodeling as a result of forces (or lack of forces) placed on them. Numerous, controlled studies have demonstrated that people who exercise regularly have greater bone density than those who are more sedentary. Any type of exercise will stimulate the deposition of more bone tissue, but resistance training has a greater effect than cardiovascular activities. Resistance training is especially important to slow down the eventual bone loss due to aging and for preventing osteoporosis. |
NASA astronaut Steve Swanson, Expedition 40 commander, equipped with a bungee harness, exercises on the Combined Operational Load Bearing External Resistance Treadmill (COLBERT) in the International Space Station. (Image credit: "iss040e086619" by NASA Johnson is licensed under CC BY-NC 2.0) |
Nutrition and Bone Tissue: Calcium and Vitamin D
Calcium is a critical component of the bone extracellular matrix, especially in the form of calcium phosphate and calcium carbonate. Calcium must be obtained from the diet, but it cannot be absorbed by the small intestine without vitamin D. Therefore, intake of vitamin D is also critical to bone health. Milk and other dairy foods are key sources of dietary calcium as are green leafy vegetables, broccoli, and intact salmon and canned sardines with their soft bones. Nuts, beans, seeds, and shellfish provide calcium in smaller quantities.
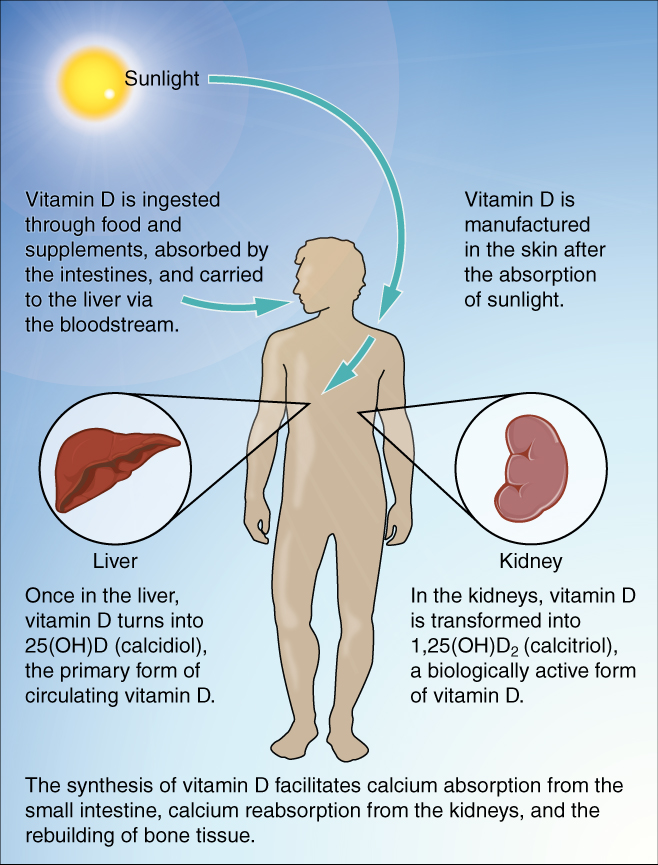
Vitamin D is not found naturally in many foods, except for fatty fish like salmon and tuna or fortified milk or cereal, so the body must produce it from a cholesterol precursor. Sunlight on the skin triggers the body to produce vitamin D (Figure \(\PageIndex{3}\)), but many people, especially those of darker complexion and those living in northern latitudes where the sun’s rays are not as strong, are deficient in vitamin D. In cases of deficiency, a doctor can prescribe a vitamin D supplement.
Figure \(\PageIndex{3}\) shows a simplified version of vitamin D synthesis. Vitamin D manufactured in response to UV-B radiation absorption by the keratinocytes of the stratum spinosum will enter the bloodstream. From the bloodstream vitamin D is delivered to either the liver or the kidneys. When vitamin D reaches the liver, it is converted into the primary form of circulating vitamin D (calcidiol). In the kidneys, vitamin D is transformed into calcitriol, a more potent but short-lived form of vitamin D. Both forms of vitamin D then facilitate calcium absorption from the small intestine, calcium reabsorption from the kidneys, and the rebuilding of bone tissue.
Hormones and Bone Tissue
The endocrine system produces and secretes hormones, many of which interact with the skeletal system. These hormones are involved in controlling bone growth, maintaining bone once it is formed, and remodeling it.
Hormones That Influence Osteoblasts
Several hormones are necessary for controlling bone growth and maintaining the bone matrix. The pituitary gland secretes growth hormone (GH), which, as its name implies, controls bone growth in several ways: it triggers chondrocyte proliferation in epiphyseal plates, resulting in the increasing length of long bones, and it increases calcium retention and stimulates osteoblastic activity, which improves bone density.
GH is not alone in stimulating bone growth and maintaining osseous tissue. During puberty, the sex hormones (estrogen from the ovaries, testosterone from the testes) also promote osteoblastic activity and production of bone matrix, and they are responsible for the growth spurt that often occurs during adolescence. They also promote the conversion of the epiphyseal plate to the epiphyseal line (i.e., cartilage to its bony remnant), thus bringing an end to the longitudinal growth of bones.
Skeletal System:
Osteoporosis is a disease characterized by a decrease in bone mass that occurs when the rate of bone resorption exceeds the rate of bone formation, a common occurrence as the body ages. Histologically, osteoporosis is characterized by a reduction in the thickness of compact bone (cortical thinning) and in the number and size of trabeculae in cancellous bone (trabecular thinning) (Figure \(\PageIndex{4}\)). As a result of having fewer, thinner trabeculae the spaces within the cancellous bone become larger, which is where the "porous" appearance comes from.
While osteoporosis can involve any bone, it most commonly affects the proximal end of the femur and the vertebrae. As a result of the loss of bone density, the osseous tissue may not provide adequate support for everyday functions and something as simple as a sneeze can cause a vertebral fracture. When an elderly person falls and breaks a hip (really, the femur), it is very likely the femur that broke first, which resulted in the fall.
For many elderly individuals, a hip fracture can be life threatening. The fracture itself may not be serious, but the immobility that comes during the healing process can lead to the formation of blood clots that can lodge in the capillaries of the lungs resulting in respiratory failure, pneumonia due to the lack of poor air exchange that accompanies immobility, pressure sores (bed sores) that allow pathogens to enter the body and cause infections, and urinary tract infections from catheterization.
Current treatments for managing osteoporosis include bisphosphonates (the same medications often used in Paget’s disease), calcitonin, and estrogen (for women only). Bisphophonates is a class of medications that inhibit osteoclast activity, acting in synergy with calcitonin. Estrogen promote osteoblast activity. Another important step in managing the potential outcomes from osteoporosis is minimizing the risk of falls, for example, by removing tripping hazards.
 A.
A. B.
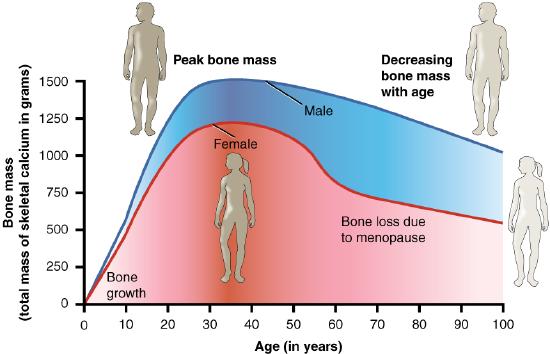
B.Bone mass (total mass of skeletal calcium in grams) peaks around 30 years of age for both males and females (Figure \(\PageIndex{4}\)). Females lose bone mass more quickly than males starting at about 50 years of age. This occurs because 50 is the approximate age at which females go through menopause and the ovaries cease the production of estrogen, a hormone that promotes osteoblastic activity and production of bone matrix. Thus, osteoporosis is more common in females than in males, but males can develop it too. Anyone with a family history of osteoporosis has a greater risk of developing the disease, so the best treatment is prevention, which should start with a childhood diet that includes adequate intake of calcium and vitamin D and a lifestyle that includes weight-bearing exercise. Promoting proper nutrition and weight-bearing exercise early in life can maximize bone mass before the age of 30, thus reducing the risk of osteoporosis.
Hormones That Influence Osteoclasts
Bone modeling and remodeling require osteoclasts to resorb unneeded, damaged, or old bone, and osteoblasts to lay down new bone. Two hormones that affect the osteoclasts are parathyroid hormone (PTH) and calcitonin. These two hormones are released in response to blood calcium levels that are too low or too high and their effects are targeted at maintaining homeostatic blood calcium. PTH stimulates osteoclast proliferation and activity. As a result, calcium is released from the bones into the circulation, thus increasing the calcium ion concentration in the blood. Calcitonin, a hormone secreted by the thyroid gland, has some effects that counteract those of PTH. Calcitonin inhibits osteoclast activity and stimulates calcium uptake by the bones, thus reducing the concentration of calcium ions in the blood. As evidenced by their opposing functions in maintaining calcium homeostasis, PTH and calcitonin are generally not secreted at the same time.
Concept Review
Mechanical stress stimulates the deposition of mineral salts and collagen fibers within bones. Calcium, the predominant mineral in bone, cannot be absorbed from the small intestine if vitamin D is lacking. Vitamin K supports bone mineralization and may have a synergistic role with vitamin D. Magnesium and fluoride, as structural elements, play a supporting role in bone health. Omega-3 fatty acids reduce inflammation and may promote production of new osseous tissue. Growth hormone increases the length of long bones, enhances mineralization, and improves bone density. Thyroxine stimulates bone growth and promotes the synthesis of bone matrix. The sex hormones (estrogen from the ovaries, testosterone from the testes) promote osteoblastic activity and the production of bone matrix, are responsible for the adolescent growth spurt, and promote closure of the epiphyseal plates. Osteoporosis is a disease characterized by decreased bone mass that is common in aging adults. Calcitriol stimulates the digestive tract to absorb calcium and phosphate. Parathyroid hormone (PTH) stimulates osteoclast proliferation and resorption of bone by osteoclasts. Vitamin D plays a synergistic role with PTH in stimulating the osteoclasts. Additional functions of PTH include promoting reabsorption of calcium by kidney tubules and indirectly increasing calcium absorption from the small intestine. Calcitonin inhibits osteoclast activity and stimulates calcium uptake by bones.
Review Questions
Q. Calcium cannot be absorbed from the small intestine if ________ is lacking.
A. vitamin D
B. vitamin K
C. calcitonin
D. fluoride
- Answer
-
Answer: A
Q. Which one of the following foods is best for bone health?
A. carrots
B. liver
C. leafy green vegetables
D. oranges
- Answer
-
Answer: C
Q. Which of the following hormones are responsible for the adolescent growth spurt?
A. estrogen and testosterone
B. calcitonin and calcitriol
C. growth hormone and parathyroid hormone
D. thyroxine and progesterone
- Answer
-
Answer: A
Q. With respect to their direct effects on osseous tissue, which pair of hormones has actions that oppose each other?
A. estrogen and testosterone
B. calcitonin and calcitriol
C. estrogen and progesterone
D. calcitonin and parathyroid hormone
- Answer
-
Answer: D
Critical Thinking Questions
Q. If you were a dietitian who had a young female patient with a family history of osteoporosis, what foods would you suggest she include in her diet? Why?
- Answer
-
A. Since maximum bone mass is achieved by age 30, I would want this patient to have adequate calcium and vitamin D in her diet. To do this, I would recommend ingesting milk and other dairy foods, green leafy vegetables, and intact canned sardines so she receives sufficient calcium. Intact salmon would be a good source for calcium and vitamin D. Other fatty fish would also be a good vitamin D source.
Q. During the early years of space exploration our astronauts, who had been floating in space, would return to earth showing significant bone loss dependent on how long they were in space. Discuss how this might happen and what could be done to alleviate this condition.
- Answer
-
A. Astronauts floating in space were not exerting significant pressure on their bones; they were “weightless.” Without the force of gravity exerting pressure on the bones, bone mass was lost. To alleviate this condition, astronauts now do resistive exercise designed to apply forces to the bones and thus help keep them healthy.
Glossary
- osteoporosis
- disease characterized by a decrease in bone mass; occurs when the rate of bone resorption exceeds the rate of bone formation, a common occurrence as the body ages
Contributors and Attributions
OpenStax Anatomy & Physiology (CC BY 4.0). Access for free at https://openstax.org/books/anatomy-and-physiology


