1.30: Medial Maxillectomy
- Page ID
- 17655
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
MEDIAL MAXILLECTOMY
Johan Fagan
Medial maxillectomy refers to surgical resection of the medial and superomedial walls of the maxillary antrum. It is increasingly being done by transnasal endoscopic technique for suitable cases and when the required expertise and technology are available. This chapter will only deal with the open surgical medial maxillectomy technique.
Maxillectomy is potentially complicated by injuries to the orbital contents, lacrimal apparatus, optic nerve, ethmoidal arteries, intracranial contents, and may be accompanied by brisk bleeding. A sound understanding of the 3-dimensional anatomy of the maxilla and the surrounding structures is therefore essential. Hence the detailed description of the surgical anatomy that follows.
Surgical Anatomy
Bony anatomy
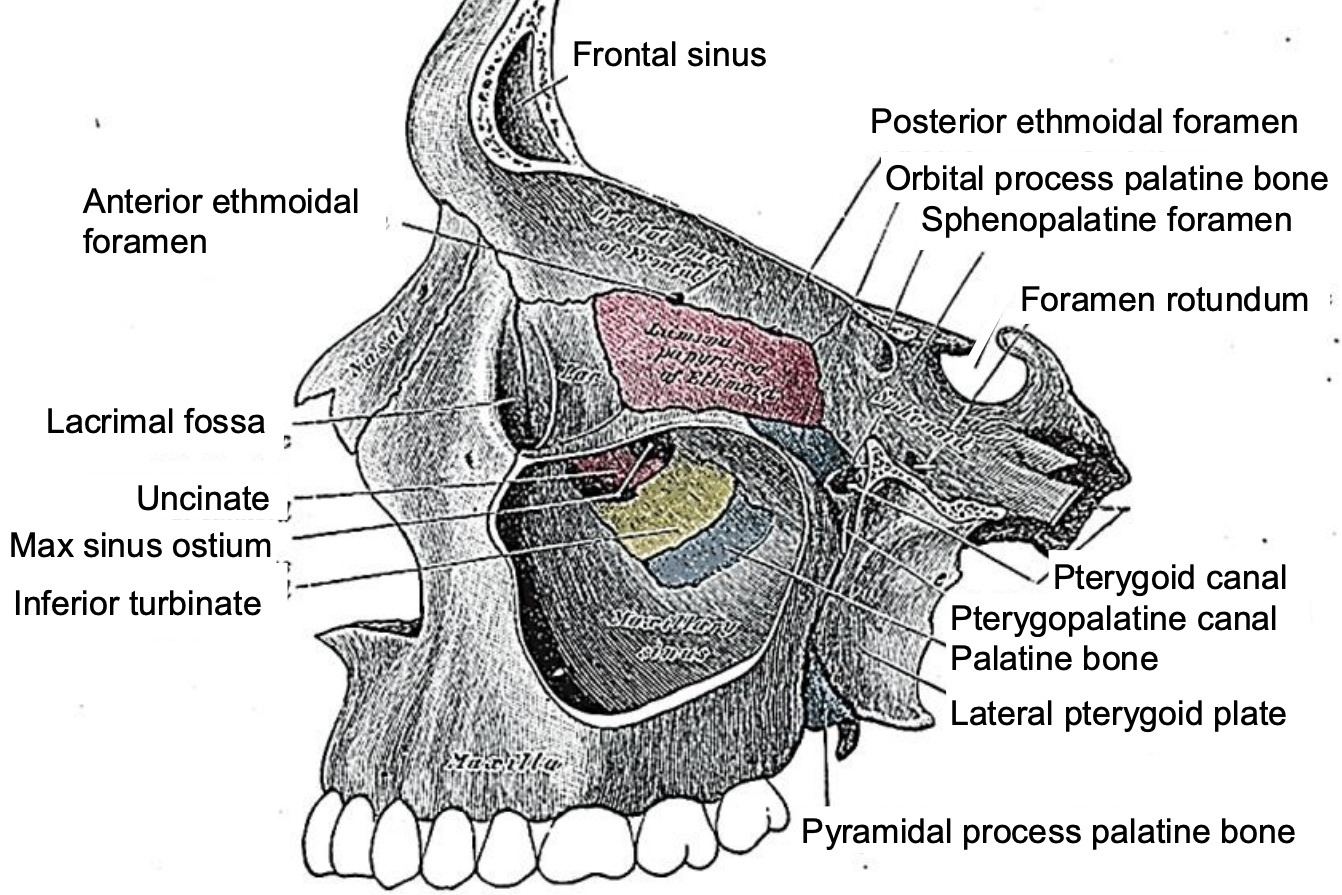
Figure 1: Lateral view of maxilla with windows cut in lateral and medial walls of maxillary sinus
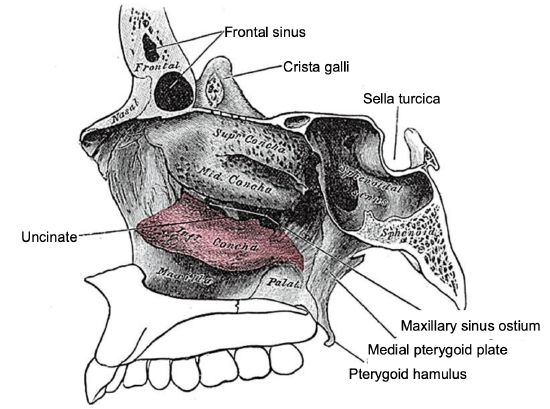
Figure 2: Bony anatomy of the lateral wall of the nose
Figures 1 & 2 illustrate the detailed bony anatomy relevant to medial maxillectomy. Critical surgical landmarks to note include:
- The level of the floor of the anterior cranial fossa (fovea ethmoidalis and cribriform plate) corresponds with anterior and posterior ethmoidal foramina located along the frontoethmoidal suture line.
- The proximity (5-11 mm) of posterior ethmoidal foramen and artery to the optic nerve within the optic foramen.
Figure 2 illustrates the bony anatomy of the lateral wall of the nose. The inferior turbinate (concha) is resected with a medial maxillectomy, but the middle turbinate is generally preserved, unless involved by pathology.
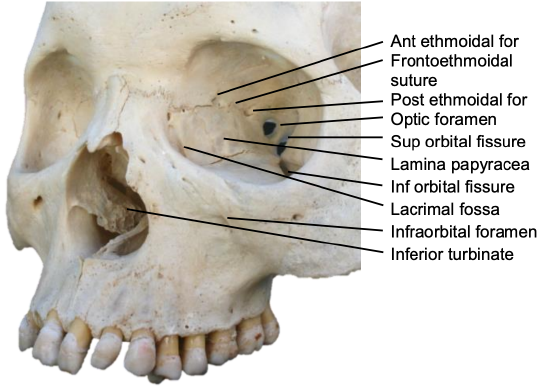
Figure 3: Bony anatomy in cadaver
Figure 3 demonstrates the anatomy of the medial wall of the nose in a cadaveric skull. Note in particular the thin lamina papyracea, the lacrimal fossa, the frontoethmoidal suture line and the anterior and posterior ethmoidal foramina and the infraorbital foramen.
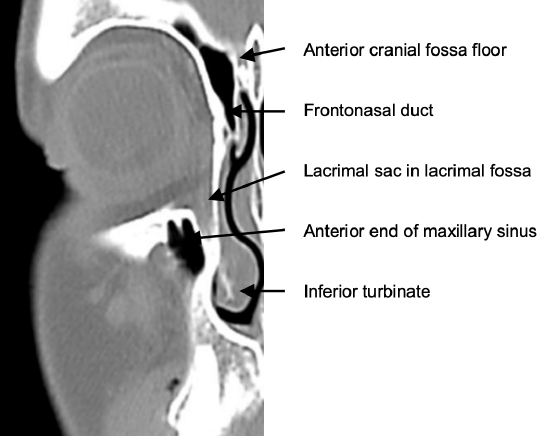
Figure 4: Coronal CT slice through lacrimal fossa
Figure 4 demonstrates the coronal anatomy at the level of the anterior extent of a medial maxillectomy. Specifically note the lacrimal sac, which is normally transected at surgery in the lacrimal fossa, and the relative heights of the floors of the antrum and the nasal cavity.
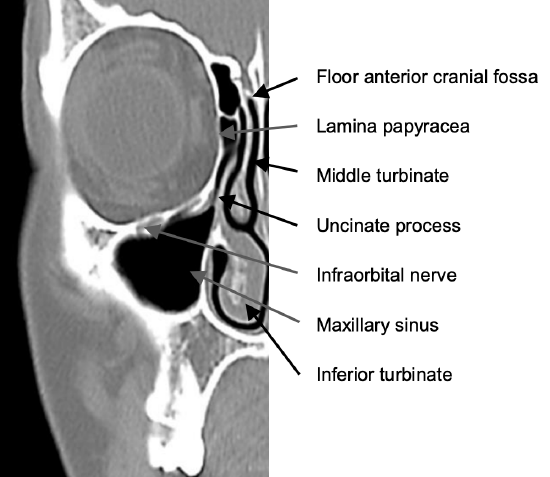
Figure 5: Anatomy in the coronal plane through the anterior ethmoids midway along a medial maxillectomy
Figure 5 demonstrates the coronal anatomy midway back along a medial maxillectomy. Specifically note the infraorbital nerve in the orbital floor, the thin lamina papyracea and the relative heights of the floors of the antrum and the nasal cavity.
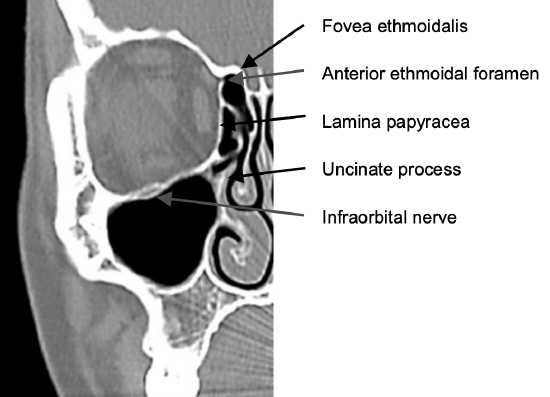
Figure 6: Note the position of the anterior ethmoidal artery where it passes through its foramen which is located in the frontoethmoidal suture line
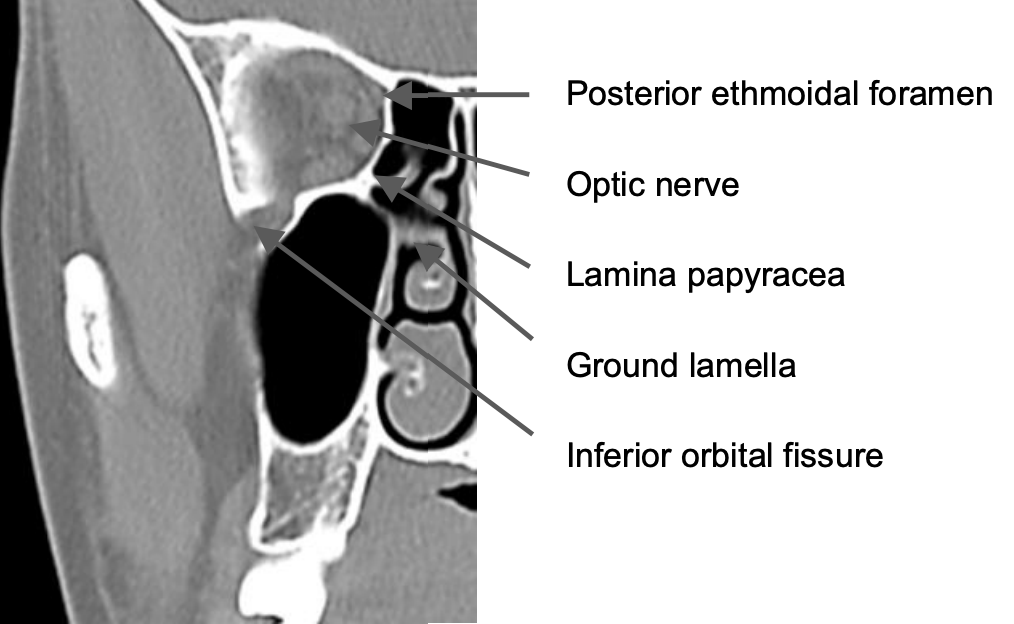
Figure 7: Coronal slice through posterior ethmoids demonstrating posterior ethmoidal foramen and optic nerve
Figures 6 & 7 demonstrate the value of using the anterior and posterior ethmoidal arteries and frontoethmoidal suture line to determine the level of the floor of the anterior cranial fossa when opening the lamina papyracea from the orbital side during medial maxillectomy.
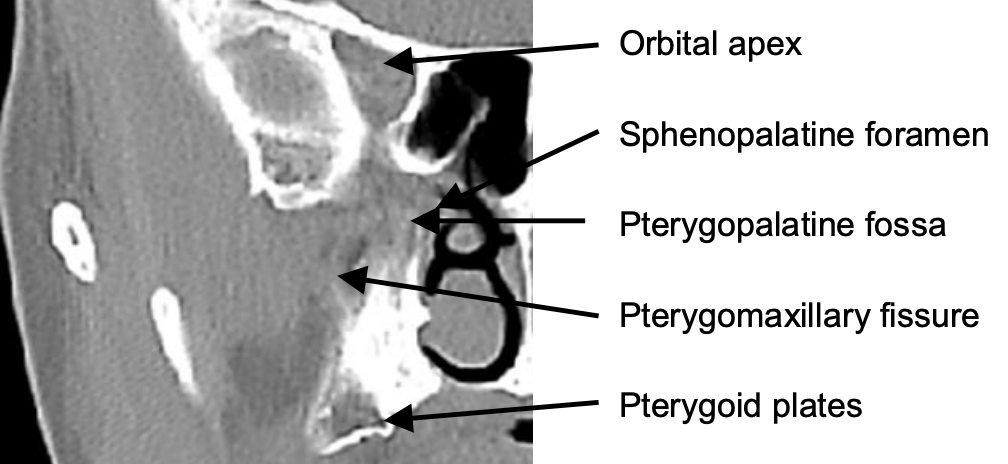
Figure 8: Coronal cut immediately behind the maxillary sinus through the orbital apex, pterygoid plates and pterygopalatine fossa.
Figure 8 demonstrates the coronal anatomy immediately posterior to the maxillary sinus, which is in the plane through which a total maxillectomy is done, and in which the internal maxillary artery and its branches as well as the sphenopalatine ganglion and its branches are encountered within the pterygopalatine fossa. The pterygopalatine fossa communicates laterally with the infratemporal fossa via the pterygomaxillary fissure, and medially with the nasal cavity via the sphenopalatine foramen.
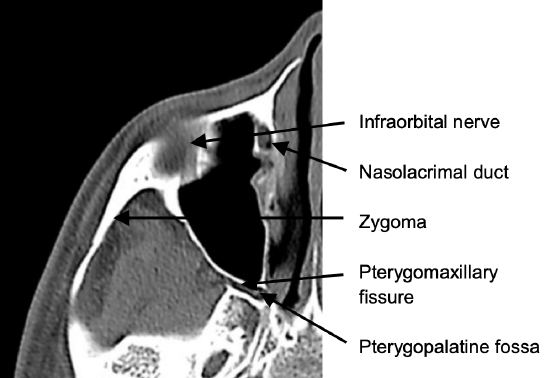
Figure 9: Axial cut at level of infraorbital nerve and orbital floor
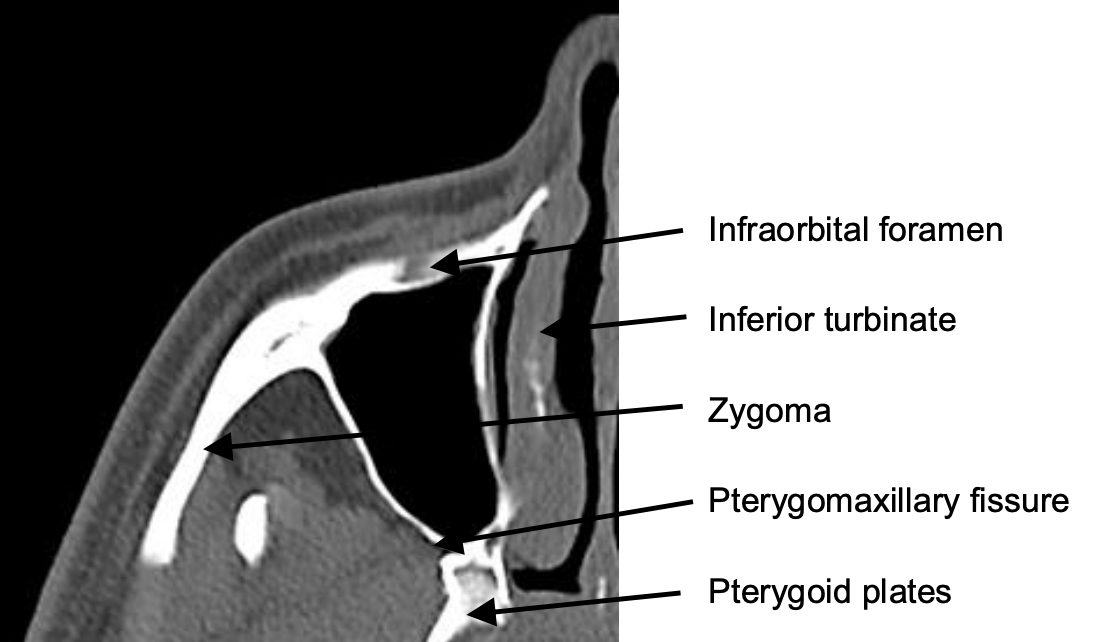
Figure 10: Axial cut at level of infraorbital foramen and pterygoid plates
Figures 9 & 10 show axial views of the anatomy of the maxillary sinus. The posterior resection lines of total and inferior maxillectomies pass through the pterygopalatine fossa and pterygomaxillary fissure and the anterior aspect of the pterygoid plates. Medial maxillectomy is done medial to the infraorbital nerve.
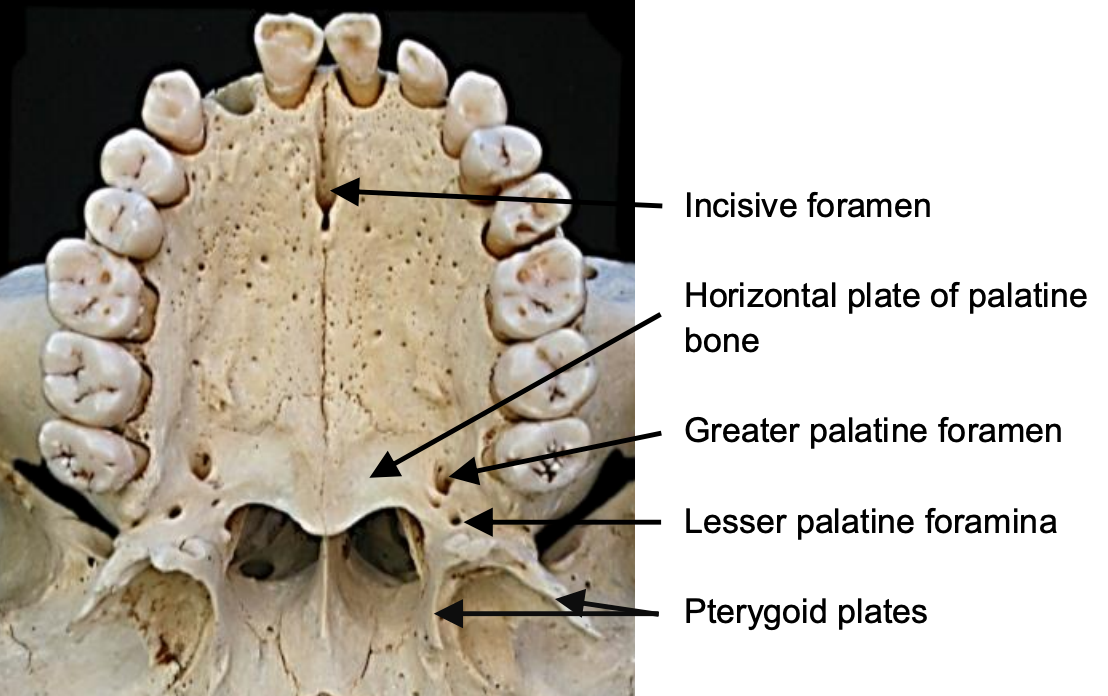
Figure 11: Anatomy of hard palate
The bony anatomy of the hard palate is illustrated in Figure 11.
Vasculature
An understanding of the blood supply of the maxilla permits the surgeon to anticipate when and where to encounter bleeding, and to plan the sequence of the surgery to reserve the bloodier parts of the surgery until last so as to minimize blood loss and to avoid blood obscuring the surgical field.
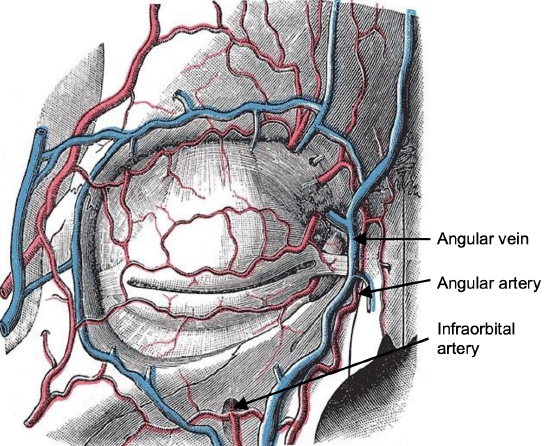
Figure 12: Vasculature around the orbit
The only significant vein encountered during maxillectomy is the angular vein (Figure 12) at the medial canthus.
The blood supply to the maxilla and paranasal sinuses originates both from the external and internal carotid artery systems. The arterial supply relevant to maxillectomy is as follows:
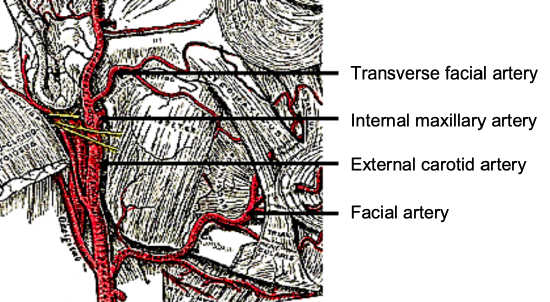
Figure 13: Facial artery and origin of internal maxillary artery, both branches of the external carotid artery
- Facial/external maxillary artery, a branch of the external carotid artery courses in the soft tissues of the face and past the medial canthus as the angular artery (Figures 12, 13).
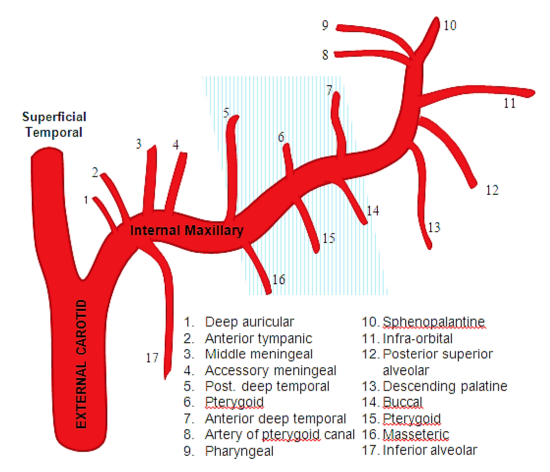
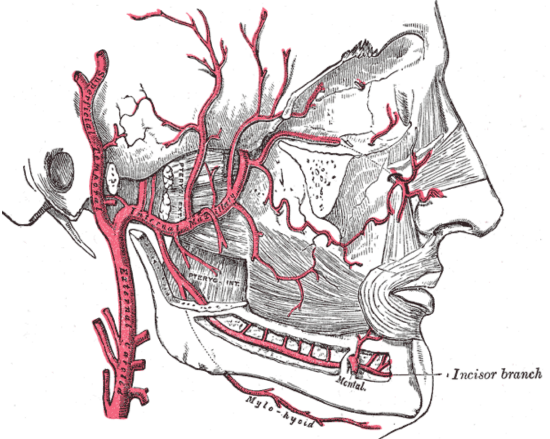
Figure 14a, b: Branches of internal maxillary artery; blue shaded area is the 2nd part of artery before it enters the pterygopalatine fossa
- Internal maxillary artery, a branch of the external carotid artery (Figures 13, 14a, b), passes through the pterygomaxillary fissure to enter the pterygopalatine fossa.
Branches of the internal maxillary artery of surgical significance include:
- Greater palatine artery (descending palatine) (Figure 14): It passes inferiorly from the pterygopalatine fossa through the pterygopalatine canal (Figure 1) and emerges from the greater palatine foramen of the hard palate (Figure 11). It then runs anteriorly medial to the superior alveolus and enters the incisive foramen (Figure 11).
- Infraorbital artery: It courses in the infraorbital groove and canal with the infraorbital nerve in the floor of the orbit/roof of antrum and exits anteriorly via the infraorbital foramen to supply the overlying soft tissues of the face (Figures 12, 14).
- Sphenopalatine artery (Figure 14): It enters the nasal cavity through sphenopalatine foramen at the back of the superior meatus where it gives origin to posterior lateral nasal branches.
- Posterior septal artery: This is a branch of the sphenopalatine artery and crosses the posterior nasal cavity just above the posterior choana to end on the nasal septum; one branch descends in a groove in the vomer to enter the incisive canal and anastomose with the greater palatine artery.
Branches of the internal carotid artery of surgical significance include:
- Anterior ethmoidal artery: It originates from the ophthalmic artery and enters the orbit through the anterior ethmoidal foramen (Figure 3) which is located 25 mm from the anterior lacrimal crest.
- Posterior ethmoidal artery: It originates from the ophthalmic artery and enters the orbit through the posterior ethmoidal foramen (Figures 3, 7). It is located approximately 36 mm from the anterior lacrimal crest, and 12 mm (8-19 mm) from the anterior ethmoidal foramen.
- Ophthalmic artery: It emerges with the optic nerve from the optic canal, 44 mm from the anterior lacrimal crest and approximately 6 mm (5-11 mm) from the posterior ethmoidal foramen.
Nerves
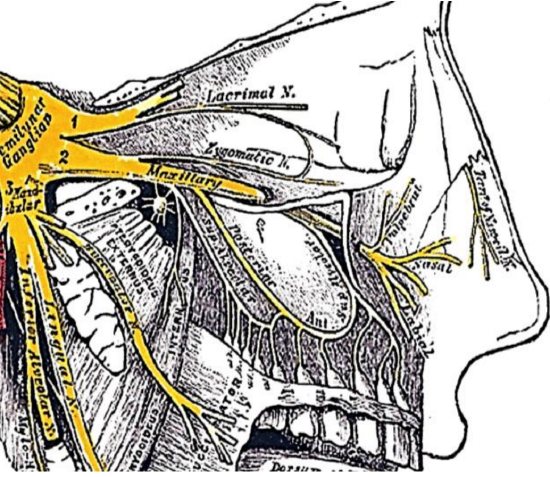
Figure 15: V2, pterygopalatine ganglion and infraorbital nerve
The maxillary division of V (V2) enters the pterygopalatine fossa via foramen rotundum. The only branch of surgical significance is the infraorbital nerve. It runs in the floor of the orbit/roof of the antrum to exit from the infraorbital foramen (Figure 15). The only other major nerve that must be considered at maxillectomy is the optic nerve.
Orbital structures
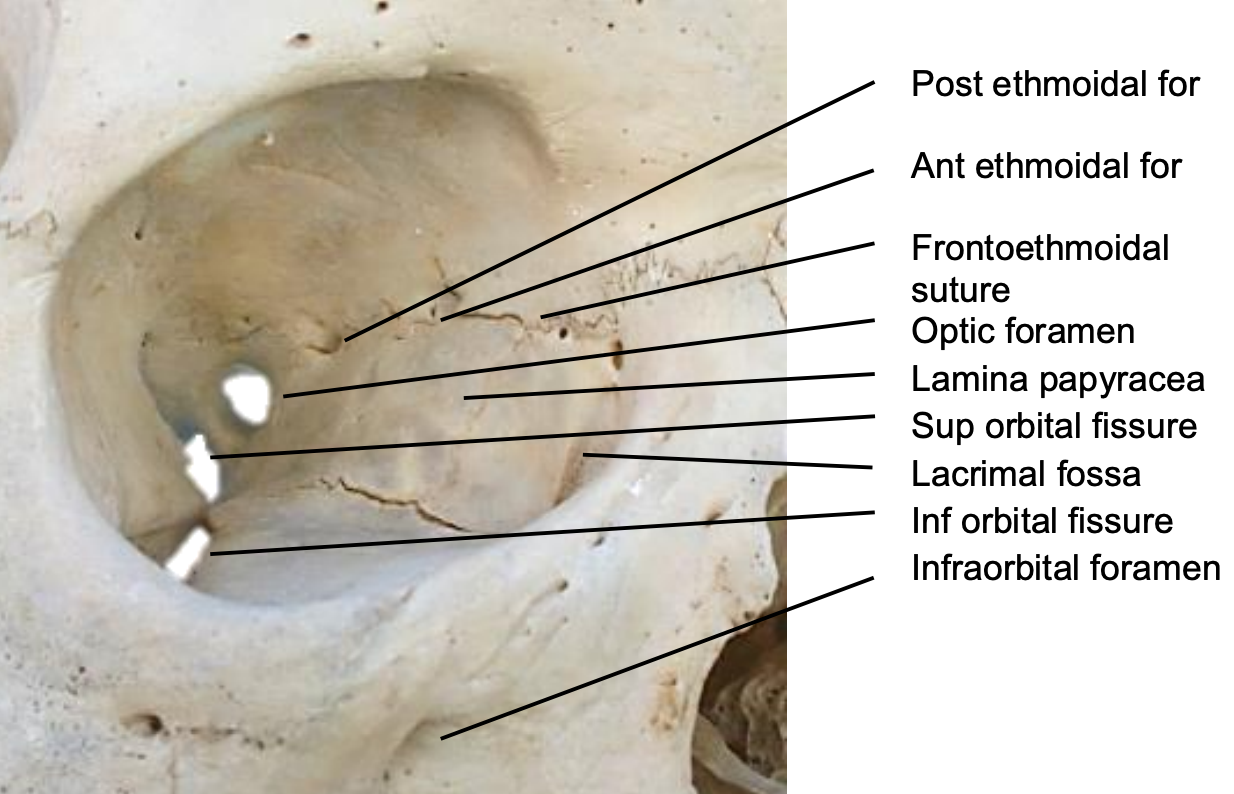
Figure 16: Right medial orbital wall
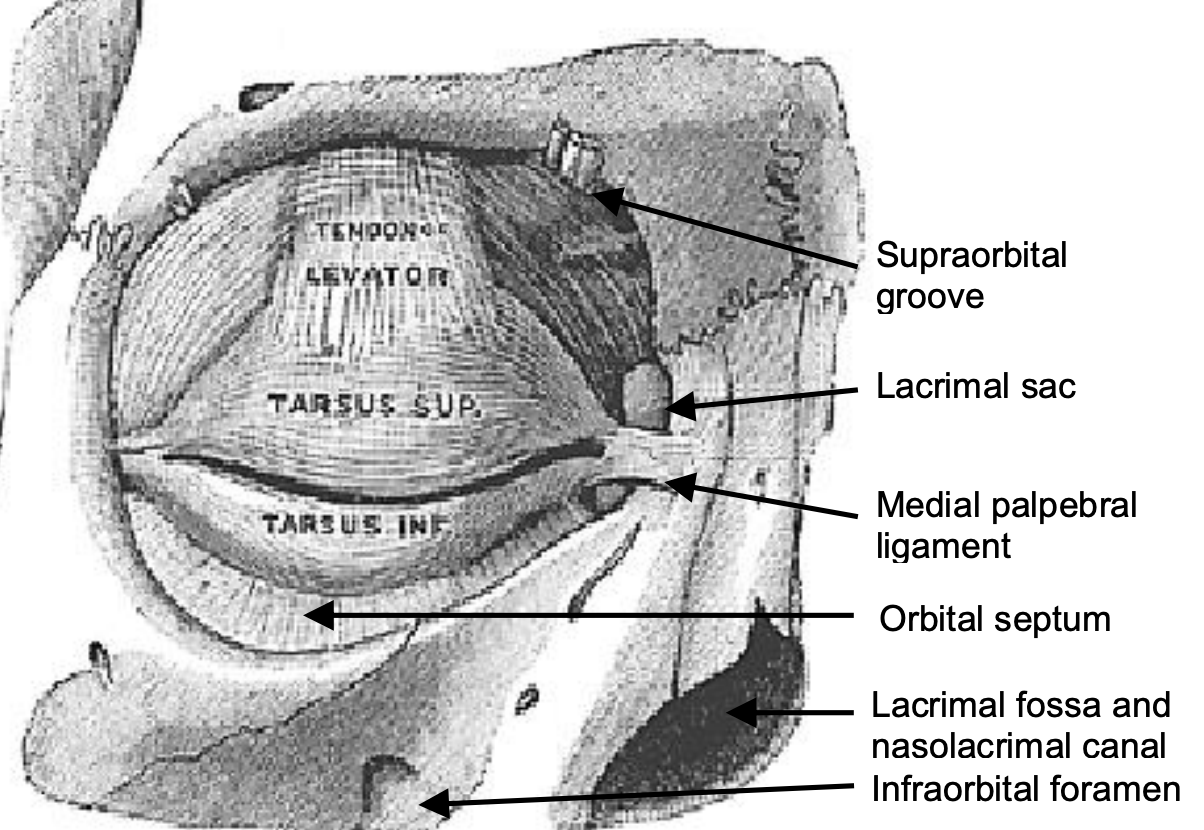
Figure 17: Right orbit showing medial palpebral ligament, orbital septum, lacrimal sac and lacrimal fossa
Figure 16 shows the detailed bony anatomy of the orbit. During dissection of the orbit, the following structures are encountered: medial palpebral ligament, orbital septum, lacrimal sac, periosteum, anterior and posterior ethmoidal arteries and inferior orbital fissure (Figure 16, 17). Only when doing orbital exenteration is the superior orbital fissure encountered.
- Orbital septum (Figure 17): This connective tissue structure attaches peripherally to the periosteum of the orbital margin and acts as a diaphragm that retains the orbital contents. Laterally, it is attached to the orbital margin 1.5 mm anterior to the attachment of the lateral palpebral ligament to the lateral orbital tubercle. The septum continues along the superior orbital rim. Superomedially it crosses the supraorbital groove, passes inferomedially anterior to the trochlea, and follows the posterior lacrimal crest behind the lacrimal sac. It then crosses the lacrimal sac to reach the anterior lacrimal crest, passes inferiorly along the anterior lacrimal crest and then laterally along the inferior orbital rim.
- Medial palpebral ligament (medial canthal tendon) (Figure 17): This is a fibrous band that fixes the tarsi to the medial orbital wall. It is intimately related to the lacrimal drainage system. It lies anterior to the canaliculi, but a deep head inserts into the posterior lacrimal crest and onto the fascia of the lacrimal sac.
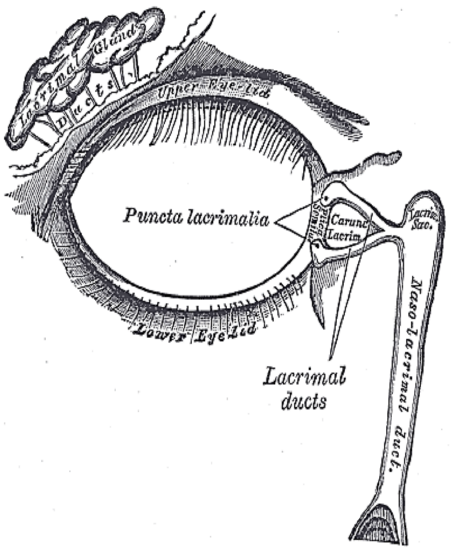
Figure 18: Right lacrimal system
- Lacrimal sac (Figures 1, 3, 4, 16, 17, 18): It is located in the lacrimal fossa, which is bound medially by the lacrimal bone and the frontal process of the maxilla (Figure 1, 16). It is related anteriorly, laterally, and posteriorly to the medial palpebral ligament.
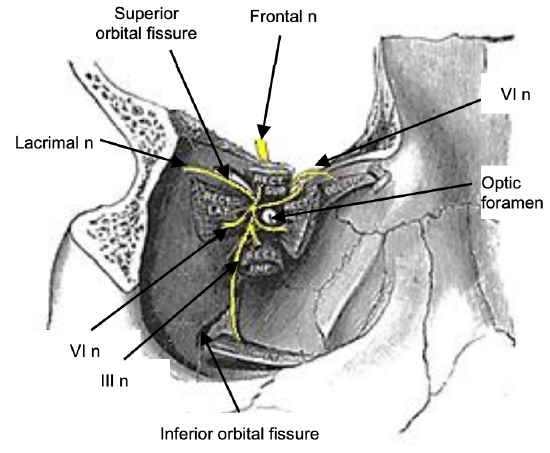
Figure 19: Inferior and superior orbital fissures of (R) orbit
- Inferior orbital fissure (Figure 16, 19): This fissure is situated in the floor of the orbit and separates the sphenoid bone from the maxilla. It transmits the maxillary nerve and a few minor nerves, but no vessels of surgical significance.
- Superior orbital fissure (Figure 16, 19): This fissure lies between the lesser and greater wings of the sphenoid bone. Important anatomical structures that pass through the fissure are cranial nerves III, IV, VI; and the superior and inferior divisions of ophthalmic vein.
Medial Maxillectomy
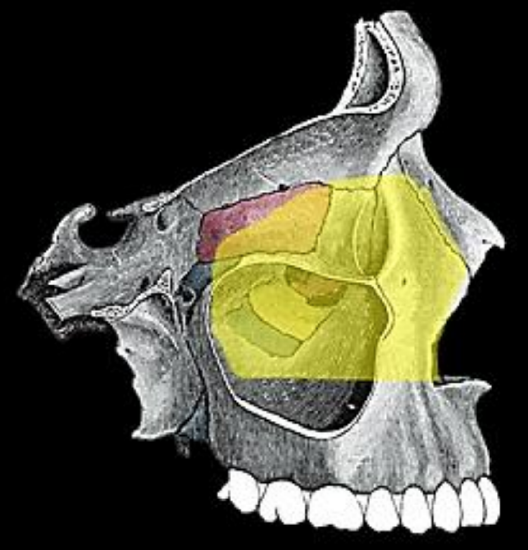
Figure 20: Yellow area indicates extent of bony resection of medial maxillectomy
Medial maxillectomy entails resection of the lateral wall of the nasal cavity (medial wall of antrum and orbit), the ethmoid sinuses and the medial part of the orbital floor (Figure 20).
It is employed with tumors (including inverting papilloma) involving the lateral wall of the nose, the lacrimal sac, and ethmoids. CT scan is an important means of anticipating the extent of maxillectomy that is required and to assess the anatomy of the skull base and paranasal sinuses. Once a tumor involves orbital fat, extends inferiorly to invade the palate or nasal floor, extends laterally beyond the infraorbital foramen, or involves the posterior antral wall and beyond, then more extensive resection is required.
Surgical steps
Preoperative consent includes discussing the facial incisions, injury to the optic and infraorbital nerves, diplopia, epiphora, enophthalmos, telecanthus, and CSF leak. The operation is done under general anesthesia, with orotracheal intubation. Perioperative broad-spectrum antibiotics are administered for 24 hours. Local anesthetic with vasoconstrictor is injected along the planned skin incisions. The nasal cavity is decongested with a topical vasoconstrictor. The eyelids are sutured together with 6/0 silk taking care not to invert the eyelashes to avoid corneal abrasions.
The operation may be considered in 3 stages: soft tissue dissection/bone exposure; bone resection; and closure/reconstruction.
It is important to complete the soft tissue dissection and bone exposure before doing any bone work to avoid excessive blood loss.
Soft tissue dissection/bone exposure
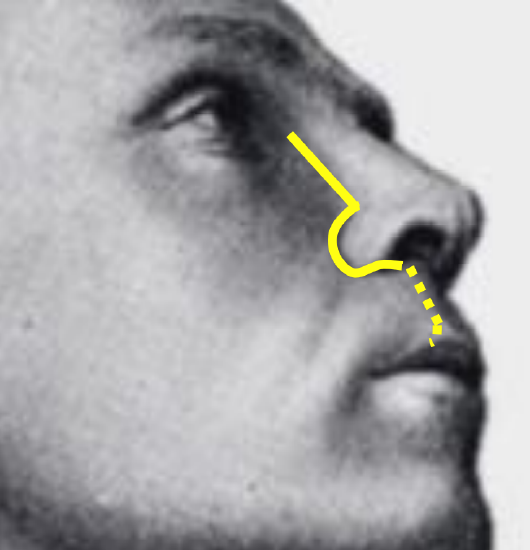
Figure 21: Lateral rhinotomy incision. Very rarely is the lip split extension required for access
- Medial maxillectomy may be done via midfacial degloving or lateral rhinotomy approach (Figure 21). The midfacial degloving approach avoids facial scars and is suited to resections that do not extend above the orbital floor i.e. do not include resection of the lamina papyracea and ethmoids. Once the resection requires removal of the medial wall of the orbit and the ethmoids, lateral rhinotomy provides better access. The skin is incised with a scalpel. The remainder of the soft tissue dissection may be done with electrocautery. The incision is extended onto the nasal bone and the maxilla. The angular vessels are cauterized or ligated adjacent to the medial canthus of the eye (Figure 12).
- The soft tissues of the face are elevated off the face of the maxilla using cautery or an elevator, remaining hard on bone while doing this dissection. Expose the entire face of the maxilla. Stop the dissection laterally at the infraorbital foramen taking care to preserve the infraorbital nerve and to avoid bleeding from the infraorbital artery.
- Sequentially identify the medial palpebral ligament, anterior lacrimal crest, the lacrimal sac in the lacrimal fossa, and the posterior lacrimal crest. Elevate the lacrimal sac from its fossa and transect it as distally as possible with a scalpel, to facilitate a dacryocystorhinostomy. Expect some bleeding from the transected sac.
- Next, the medial and inferior orbit is exposed. The periosteum is stripped from the nasal bone and frontal process of the maxilla, taking care to remain in a subperiosteal plane. Strip the orbital contents in an extraperiosteal plane from the lamina papyracea and frontal bone taking care not to fracture or penetrate the thin bone of the lamina papyracea.
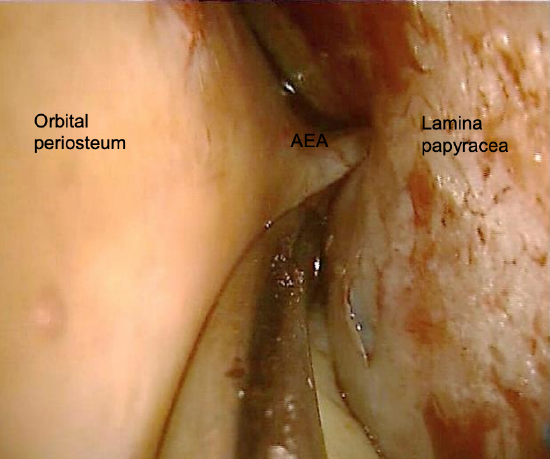
Figure 22: Anterior ethmoidal artery (AEA) exiting foramen at level of frontoethmoidal suture line (right eye)
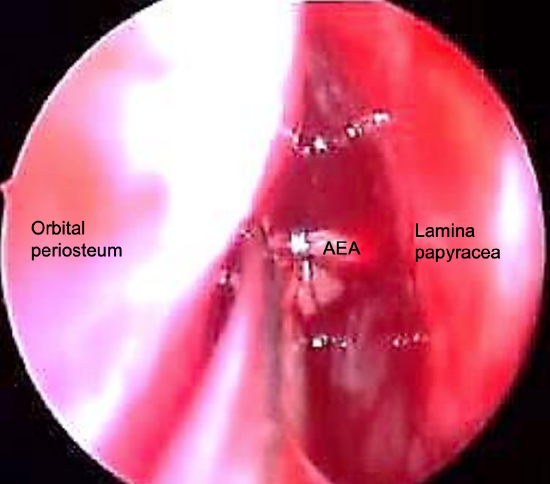
Figure 23: Liga clips being applied to anterior ethmoidal artery (AEA)
- Identify the frontoethmoidal suture line. This is a crucial surgical landmark as it corresponds with the level of the cribriform plate and the anterior and posterior ethmoidal foramina. Retract the orbital contents laterally and identify the anterior ethmoidal artery as it bridges the divide between the anterior ethmoidal foramen and the periorbita (Figure 22, 23). The anterior ethmoidal artery is ligated, clipped or bipolared and divided, thereby providing access to the posterior ethmoidal artery. It is generally not necessary to divide this vessel.
- Now strip along the floor of the orbit in an extraperiosteal plane. Take special care not to tear the periosteum at the inferior orbital margin at the attachment of the orbital septum to avoid entering the orbital fat and causing extrusion of the fat.
- Next free the soft tissues from the bone up to the anterior free margin of the nasal aperture with diathermy. Retract the nasal ala and incise the lateral wall of the nasal vestibule to expose the ipsilateral nasal cavity and inferior turbinate, taking care not to injure the inferior turbinate of septum to avoid troublesome bleeding.
At this point the soft tissue dissection is complete.
Bony resection

Figure 24: Anterior antrostomy, taking care not to injure infraorbital nerve
- An antrostomy is made in the anterior face of the maxilla with a hammer and gouge or a burr, entering the antrum through the thin bone in the canine fossa. A punch or bone nibbler is used to remove the majority of the bone of the anterior wall of the maxillary sinus up to the orbital rim superiorly, but taking care to leave a margin of bone around the infraorbital foramen so as to protect the nerve and to avoid bleeding from the infraorbital vessels (Figure 24). Inspect the antrum to determine the extent of the tumor and to plan the subsequent bony cuts.
- The medial maxillectomy can now been done. The extent of the bony resection is tailored to the primary tumor.

Figure 25: Coronal CT anteriorly demonstrating resected lateral nasal wall, orbital walls and transected lacrimal sac

Figure 26: Coronal CT demonstrating resected lateral nasal wall including inferior turbinate and uncinate process, orbital floor up to infraorbital nerve, lamina papyracea and anterior ethmoidectomy, with preservation of the middle turbinate

Figure 27: Coronal CT more posteriorly demonstrating resected lateral nasal wall, inferior turbinate and inferomedial orbital wall, and ethmoidectomy with resection remaining below the level of the posterior ethmoidal foramen, and with preservation of middle turbinate
- Figures 25 – 27 illustrate the extent of the bone resection with a classic medial maxillectomy.
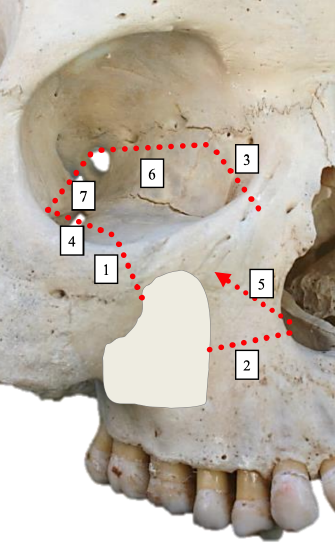
Figure 28: A sequence for osteotomies
- The sequence of the osteotomies is planned to reserve troublesome bleeding to the end (Figure 28). This may have to be adjusted depending on the location and extent of the tumor.
- Osteotomy through inferior orbital rim: A sharp osteotome/power saw/ bone nibbler is used to cut through the thick inferior orbital rim just medial to the infraorbital nerve
- Osteotomy connecting antrostomy with nasal vestibule: A sharp osteotome is used to connect the anterior antrostomy with the floor of the nasal vestibule.
- Osteotomy across frontal process of maxilla: This part of the dissection is often best done with a Kerrison’s rongeur or oscillating saw. There is often persistent minor bleeding from the bone that may be controlled with bone wax or cautery. The osteotomy is stopped short of the level of the frontoethmoidal suture.
- Osteotomy along orbital floor: While retracting and protecting the orbital contents with a narrow copper retractor an osteotomy is continued posteriorly through the thin bone of the orbital floor/antral roof using either a sharp osteotome or heavy scissors, aiming for the posteromedial corner of the roof of the maxillary sinus.
- Osteotomy along floor of nose: A sharp osteotome or heavy scissors is used to divide the lateral wall of the nose/medial wall of the antrum along the floor of the nasal cavity up to the posterior wall of the antrum. When doing this dissection with an osteotome, the dissection is halted when the osteotome hits up against the solid pterygoid bone (signaled by a change in the sound).
- Osteotomy through lacrimal bone, lamina papyracea and anterior ethmoids: It is critical that this osteotomy be placed below the level of the frontoethmoidal suture line and the ethmoidal foramina so as to avoid fracturing or penetrating through the cribriform plate. The osteotomy is done be gently tapping on an osteotome to enter the ethmoid air cell systems while carefully retracting the orbital contents laterally. The osteotomy stops short of the posterior ethmoidal artery to safeguard the optic nerve.
- Vertical posterior osteotomy through posterior ethmoids and along posterior wall of antrum and pterygopalatine fossa: The final posterior vertical cut is made with a heavy curved (Mayo) scissors as a downward continuation of the osteotomy in (6). It runs though the medial wall of the maxillary sinus, starting superiorly at the posterior end of the previous osteotomy, and ending at the level of the nasal floor.
- The medial maxillectomy specimen is then removed by gently levering it inferiorly and laterally with the Mayo scissors while completing the posterior osteotomy, in the process fracturing through the apex of the orbital floor and the posterior ethmoids cells and remaining lateral to and preserving the middle turbinate.
- The specimen is inspected to determine the adequacy of the tumor resection.
- An external ethmoidectomy may safely be completed up to the cribriform plate.
- The ethmoids are carefully inspected to determine whether an external frontoethmoidectomy +/- sphenoidectomy is required, and for evidence of a CSF leak.
Clinical example

Figure 29: Malignancy of the lacrimal sac resected with a medial maxillectomy
Closure/Reconstruction
Hemostasis is achieved with cautery, bone wax and or topical hemostatics. It is only rarely necessary to pack the nose.
The objectives of closure are to minimize enophthalmos, diplopia, epiphora and an unsightly scar. It is not unusual for patients to complain of some diplopia, but this usually resolves with the passage of time. Suture any tears in the periorbita to avoid herniation of orbital fat. The lacrimal sac is slit open along its longitudinal axis and the edges are sutured to the surrounding tissues to avoid epiphora. If an extensive resection of the orbital floor has been done, then consideration should be given to reconstructing the floor with fascia / bone / titanium mesh. The skin is carefully repaired to optimize the cosmetic results. Patients are instructed about nasal douching and are recalled for nasal toilette.
Author & Editor
Johan Fagan
MBChB, FCS (ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


