1.4: Histology of the Teeth and Periodontal Tissue
- Page ID
- 41540
- Overview
- Bone tissue review
- Histology of teeth
- Enamel
- Dentin
- Pulp
- Cementum
- Histology of the periodontium
- Periodontal Ligament
- Alveolar bone
- Summary of hard tissues
Overview
This chapter briefly covers the histology of the hard tissues enamel, dentin, cementum and bone, as well as the soft tissues of pulp and the periodontal ligament. The definitions and clinical considerations of these tissues are addressed in the chapters on the development of these tissues (Chapters 8-11)
For more practice using histology images, we share these useful links
- The Oral histology Lab
- by Brian R. MacPherson, Ph.D. and James G. Tieman, Ed.D., at the University of Kentucky (we linked to this in the previous chapter as well)
- The Microanatomy Web Atlas
- by Gwen V. Childs, Ph.D., FAAA at the University of Arkansas for medical sciences. Jump to the digestive system/tooth unit.
Histology of bone tissue (brief review)
Bone tissue is deposited in layers by osteoblasts. These cells become trapped within lacunae between layers of bone tissue, and differentiate into osteocytes. Bone tissue can either be compact and made of osteons, or spongy bone made of trabeculae. Bone tissue is almost entirely ECM, summarized in Table 4.1. Bone tissue is highly vascular—compact bone contains central canals and perforating canals, whereas in spongy bone the space between bony trabeculae is filled with red bone marrow or highly vascular adipose connective tissue.
| Components of bone tissue | |
|---|---|
| <1% | Osteocytes |
| 66% | Mineral ECM: Calcium Hydroxyapatite |
| 33% | Protein ECM: Collagen |
Table 4.1: Components of bone tissue
Histology of teeth
Histology of enamel
Enamel shares some mineral characteristics with bone tissue, but it is acellular and avascular. Enamel matrix is deposited in columns called enamel rods by cells called ameloblasts. Enamel is the strongest substance in the human body, on account of its high mineral content, listed in Table 4.2.
| Components of enamel | |
|---|---|
| 0.0% | Cells (there are no cells) |
| 96% | Mineral ECM: Calcium Hydroxyapatite |
| 4% | Protein ECM: Amelogenins and Enamelin (not collagen) |
Table 4.2: Components of enamel

During embryonic development, ameloblasts work on a circadian rhythm, depositing ECM at a regular pace for 4 days, then changing speed. The changes in speed leads to changes in enamel density, which can be seen as horizontal Striae of Retzius. Another pattern is visible because ameloblasts do not create an enamel rod in a perfectly straight line, but changes directions slightly over days. This leads to the pattern known as Hunter-Schreger bands. The border between enamel and underlying dentin is a distinct line named the Dentino-enamel Junction (DEJ).
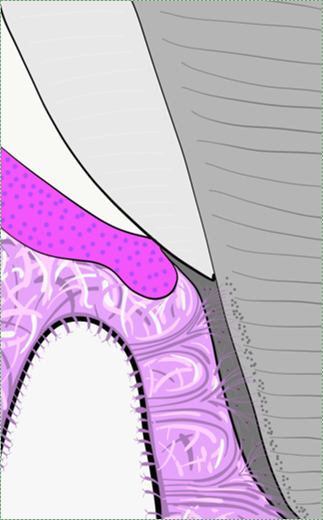
Histology of dentin
Dentin, like enamel, is avascular, but it should not be called acellular. Dentin matrix is deposited by cells called odontoblasts. These cells—or more accurately, their cell bodies– are found within the pulp cavity, immediately adjacent to the dentin. Each odontoblast has an arm-like protrusion called an odontoblastic process that extends nearly the entire thickness of the dentin ECM that cell secreted. The odontoblastic process secretes more dentin (in a soft form that hardens later), as well as a fluid called dentinal fluid into the space known as a dentinal tubule. Dentin is not as strong as enamel, because of its lower mineral content, listed in Table 4.3.
| Components of dentin | |
|---|---|
| – | Cells (odontoblasts cell bodies in pulp, odontoblastic processes in dentin) |
| 70% | Mineral ECM: Calcium Hydroxyapatite |
| 30% | Protein ECM: Collagen, mostly |
Table 4.3: Components of dentin.

Similar to the lines of Retzius, dentin is deposited at different rates over days, which creates bands called the Imbrication lines of von Ebner. These lines run perpendicular to the dentinal tubules. Exceptionally-pronounced imbrication lines are named Contour lines of Owen, and occur with exceptional changes in nutrition (such as childbirth).

Root dentin has a layer of speckles near the border with the cementum named Tome’s granular layer. It has no known function. It is a good landmark when looking at dentin under the microscope, its presence indicates you are viewing root dentin, not mantle dentin, and a thin layer of cementum should be close by.
Histology of pulp
The pulp chamber is composed of an indeterminate type of connective tissue, although it most resembles areolar connective tissue. The most common cell types found within the pulp core are fibroblasts and mesenchymal stem cells. The pulp houses the blood, nerve and lymphatic supplies for each tooth. The pulp has 4 layers that appear distinct under the microscope listed in Table 4.4.
| Layer | Predominant feature |
|---|---|
| Odontoblast layer | Odontoblast cell bodies |
| Cell-free zone | Not actually free of cells, cells aren’t visible |
| Cell-rich zone | Cells are visible and densely packed |
| Pulp core | Location of capillaries, nerve endings and lymphatic vessels |
Table 4.4: The four layers of the pulp chamber and their predominant features.
Histology of cementum
Cementum forms a thin layer (roughly 60 µM, but see below) over the surface of root dentin, which is roughly the width of a hair. The ECM of cementum differs significantly enough from enamel that the two can be differentiated by their color (cementum is yellowish in hue), whereas no significant color difference exists between cementum and dentin. The ECM of cementum is deposited by cementoblasts, which can be found on the surface of cementum throughout life. As a result, the thickness of cementum can triple in thickness between the ages of 10 and 70 years of age. Cementum incorporates more fluoride than the other hard tissues.
Cementum, like dentin and enamel, is an avascular tissue, but it can contain cells. There are two types of cementum based on histological (visual) studies dating back to the 1830s. These two types are cellular and acellular cementum. More recent advances in molecular biology and genetics are yielding newer concepts, but the old classification system still rules.
In cellular cementum, cementoblasts are trapped within the ECM and differentiate into cementocytes. In the mature tissue, Cementocytes are found within lacunae, similar to bone tissue. However, canaliculi only extend in the direction of the periodontal ligament. In the opposite direction is avascular dentin, which cannot provide cementocytes with nutrients. Cellular cementum is found in the apical half of the root.
Acellular cementum does not contain cementocytes, and can be found in the coronal half of the root. The border between cementum and dentin– the Dentino-cemental junction— is less distinct than the DEJ. Cementum is slightly less strong than dentin, and is composed of the materials listed in Table 4.5.
The lower mineral content of cementum compared to bone tissue suggests it is also less strong than bone, but as we see in subsequent chapters, the loss of bone, dentin and cementum in response to periodontitis or orthodontia is complex and requires discussion of morphogens and the differentiation of resorptive cells.
| Components of cementum | |
|---|---|
| – | Cellular cementum (apical portion)
Acellular cementum (coronal portion) |
| 50% | Mineral: Calcium Hydroxyapatite |
| 50% | Protein: Collagen and proteoglycan mixture |
Table 4.5: Components of cementum
Fibers in cementum
Acellular cementum contains extrinsic collagen fibers which travel perpendicular to the surface of the root, and are likely secreted by both fibroblasts and cementoblasts. These fibers attach to alveolar bone, and represent the ends of the principal fibers of the periodontal ligament embedded within cementum (also called Sharpey’s fibers, just as in bone tissue).
Cellular cementum contains intrinsic fibers and possibly extrinsic fibers. Intrinsic collagen fibers are secreted by cementoblasts, and do not extend beyond cementum. They are oriented parallel to the root surface and are mainly involved in the repair of cementum (a scaffold). More recent publications subdivide cellular cementum into Cellular Intrinsic Fiber Cementum and Cellular Mixed Stratified Cementum, based on the amount of extrinsic collagen fibers present. Cementum that does not contain extrinsic collagen fibers (closer to the crown, the cervical region) does not contribute to the attachment to bone tissue.
Histology of periodontal tissues
Histology of the Periodontal Ligament
The Periodontal Ligament (PDL) is a region of dense regular CT that connects the cementum to alveolar bone. Sharpey’s fibers extend from the PDL into cellular cementum. Like the dentin-cemental junction, the border between cementum and PDL is blurred due to their shared lineage. Clusters of rogue epithelial cells can be found within the PDL which are named the epithelial rests of Malassez.
Histology of alveolar bone
Alveolar bone is compact bone tissue, with a semi-unique feature of containing dozens of tiny holes through which Sharpey’s fibers from the PDL insert, as well as larger holes for the nerves, blood and lymphatic vessels than exit bone tissue and into the apical foramen of the tooth. This makes the surface of the alveolar sockets appear porous, which is almost unique for the surface of bone tissue. The porous surface is called the cribriform plate, which is not to be confused with the other region of compact bone riddled with tiny holes, the cribriform plate of the ethmoid bone (whose holes are for smell nerve endings, connecting the nasal cavity to the brain).
Resorptive cells in hard tissues
The periosteum is a layer of dense connective tissue that surrounds bone tissue. In addition to collagen fibers, it contains osteoblasts and osteoclasts involved in bone remodeling. Similar cells exist for cementum and dentin, but not enamel. Cementoclasts and Odontoclasts are capable of demineralizing cementum and dentin, respectively. Like osteoclasts, these cells express genes involved in acid secretion as well as digestive enzymes, including members of the matrix metalloproteinase family. Unlike osteoclasts, they are not active continuously in a remodeling unit, they have no baseline activity and are typically only activated during tooth exfoliation.
Odontoclasts and cementoclasts likely differentiate from the same bone marrow stem cell that can also become an osteoclast. The exact signals involved in determining whether the multi-potent stem cell differentiates into an osteoclast, odontoclast or cementoclast is not well understood. The body may regulate this process by long or medium-range hormone and growth factor signals. The trigger may also be very short-range: binding of the stem cell to proteins or glycoproteins within the ECM of target tissues, providing the stem cell with positional information. While roughly identical to osteoclasts under the microscope, odontoclasts and cementoclasts have important physiological differences. For instance, the hormone calcitonin inhibits osteoclasts but triggers odontoclast activity during root resorption. The significance of this detail is that root loss does not always match bone loss. For instance, in osteoporosis, bone loss leads to the loss of teeth, not root loss. During tooth exfoliation, however, root dentin is resorbed but alveolar bone undergoes both resorption and deposition, to form a pathway through bone above the permanent tooth and fill in alveolar socket space below.
Some publications suggest cementoclasts are distinct cells found in the periodontal ligament and that they play a role in the maintenance of cementum throughout life. Other publications suggest cementoclasts are the same cell type as odontoclasts and osteoclasts. Without further study, it is hard to tell whether a cementoclast is a distinct cell type, or an osteoclast found near cementum. The mechanism of resorption is likely the same (acids and proteinases), but whether these cell are regulated the same is an important question during root exfoliation or orthodontic movement.
Summary of hard tissues
Table 4.6 compares the components of the ECM of hard tissues.
| Hard tissue | Components | |
|---|---|---|
| Enamel | 96% | Mineral: Calcium Hydroxyapatite |
| 4% | Protein: Amelogenins and Enamelins (not collagen) | |
| Dentin | 70% | Mineral: Calcium Hydroxyapatite |
| 30% | Protein: Collagen, mostly | |
| Cementum | 50% | Mineral: Calcium Hydroxyapatite |
| 50% | Protein: Collagen and proteoglycan mixture | |
| Bone | 66% | Mineral: Calcium Hydroxyapatite |
| 33% | Protein: Collagen | |
Chapter 3 * Table of Contents * Chapter 5


