3.2: Definition and diagnosis
- Page ID
- 42734
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Definition of heart failure
The term heart failure (HF) (congestive heart failure or cardiac decompensation or decompensatio cordis) describes an acute or chronic situation in which the amount of blood pumped through the circulation by the heart, is insufficient to meet the body’s demands at a normal cardiac filling pressure. According to the guidelines of the European Society of Cardiology, HF is defined as a syndrome in which the patient has the following triad of features: (1) symptoms typical of HF; (2) signs typical of HF; and most importantly (3) objective evidence of a structural or functional abnormality of the heart at rest (Table 3.2.1).
| Symptoms Typical of Heart Failure | Signs Typical of Heart Failure | Objective evidence of a structural or functional abnormality of the heart at rest |
|---|---|---|
|
|
|
Prevalence
The prevalence of HF in the Western world is estimated to be 1-2%, and the incidence is approximately 5-10 per 1000 persons per year (7,9). Coronary heart disease at a young age is more prevalent in men than women, and so the prevalence of HF is also higher in this group compared to age matched women. In older age groups, the prevalence of HF is equal between the sexes.
Acute and chronic heart failure
Heart failure may become a chronic condition, in which HF is persistent either with recurrences or with slow progression. A patient may be described as decompensated when chronic stable HF deteriorates. Acute HF has traditionally been used to describe the nature of the clinical presentation, as severe or of recent onset. Different clinical presentations fall under this definition.
Systolic versus diastolic heart failure
Heart failure patients may be broadly classified into one of two groups, or a combination of both, depending on the left ventricular ejection fraction (LVEF). The LVEF is most often assessed with echocardiography (see Table 3.3.2). When the LVEF is less than 45%, systolic pump function is abnormal and it is named systolic HF.[3] If LVEF is preserved (>50%), symptoms are attributed to impaired relaxation of the heart during diastole and therefore this condition is diagnosed as diastolic HF or HF with a preserved LVEF.[3][4] As a result of impaired relaxation, end diastolic pressure and, subsequently, left atrial- and pulmonary pressure will rise; alveolar pulmonary edema develops as a consequence of these changes. LF diastolic dysfunction may be present in asymptomatic patients, and it is considered an important precursor of heart failure.[5] Frequently, patients have both systolic and diastolic heart failure at the same time, but the term for this ailment is still systolic heart failure. The term heart failure is not limited to a failing left ventricle; the right ventricle may also be involved in the process and there may also be isolated right ventricular heart failure.
Pathophysiology of heart failure
HF is caused by a loss of cardiac pump function, which can be due to a structural abnormality of the heart muscle (e.g. myocardial infarction) or a change in the heart function (and often structure) in response to an abnormal load (e.g. aortic valve stenosis). The relationship between loading the ventricle (by filling it) and its output was described by Frank and Starling in 1918 and has become the cornerstone in understanding heart failure and how to treat it. The relationship states that as a result of loading the heart (increasing its filling or its pressure), the output increases (Figure 3.2.1).
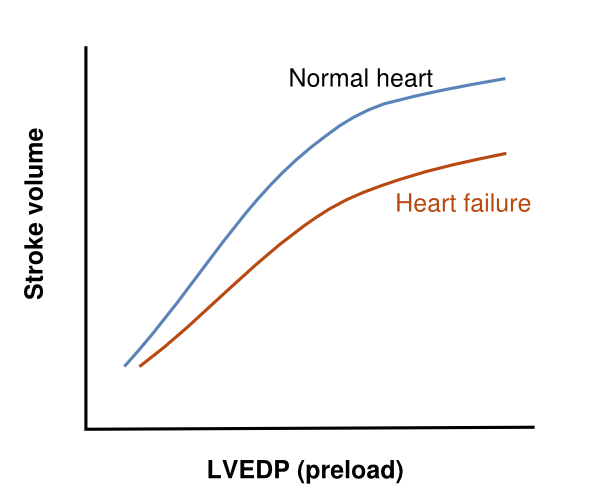
A heart that has a lower output can be improved by increasing its volume and its loading pressure. This is what naturally happens (LV dilatation and increased filling pressure) when the heart does not pump out enough volume, and, in the first phase of disease, compensates for the loss of contractility. It takes more energy from the heart to work at an increased loading, but the heart has a reasonable energy reserve. In a chronic situation, remodeling of the heart progresses (by hypertrophy of the myocytes and dilatation by increasing myocyte length and matrix changes), which, in the long term, leads to a further loss in function. The result of this dysfunction is further increased loading pressures in the heart and, by communicating the diastolic loading pressures to the left atrium and pulmonary veins, the pulmonary capillaries may become overloaded and leak water into the lungs. This is the practical restriction of further filling the heart as a tool to improve its function; even poor left ventricles may be filled more to increase their output [6] but the patients’ pulmonary capillaries cannot tolerate these hydrostatic pressures and start to leak water.
Hemodynamic explanations (the heart as a pump) use the concept of preload (filling) and afterload (workload of the heart, which is wall tension and arterial pressure or vascular resistance). In this way, the progression of left sided heart failure towards right sided heart failure is explained as follows: prolonged left ventricular failure increases pressures in the left atrium (preload), which in time leads to a subsequent increased resistance in the pulmonary vascular system (which is the afterload of the right ventricle) and eventually may also lead to right ventricular failure. Another relevant issue is afterload of the left ventricle influencing the output of the heart: as the afterload of the aortic pressure also influences the timing of closure of the aortic valve, a high aortic pressure will close the aortic valve early and will, therefore, diminish the output. Decreasing (theoretically diastolic, but more practically systolic) aortic pressure will increase the stroke volume by latter closure of the aortic valves. (Figure 3.2.2)

Hormonal/ sympathetic system mechanisms (RAAS/ Sympathetic overstimulation) of heart failure are as important as the hemodynamic mechanisms of heart failure.
A decreased cardiac output leads to diminished renal perfusion and release of hormones in the RAA-system: renin is released into the circulation by the renal juxtaglomerular apparatus, which stimulates the cleavage of angiotensinogen into angiotensin I and II during its passage through the lungs. Angiotensin II stimulates vasoconstriction in the kidneys, and in other vascular systems, increasing blood pressure; the second effect of angiotensin is to stimulate the release of aldosterone from the adrenals into the plasma, which retains sodium from the kidney tubules in the blood and thereby water. The RAA –system, which works as a compensatory mechanism for heart failure to increase blood pressure and blood volume, also stimulates hypertrophy of muscle cells and the formation of fibrosis, which in the long term are detrimental to heart failure.
The other compensatory mechanism for heart failure, stimulation of the sympathetic nervous system, increases heart rate to increase cardiac output, which is a powerful compensatory mechanism. However, chronic stimulation of the sympathetic nerves to the heart, leading to higher heart rates, is toxic to the heart, because of continuous release of norepinephrine to the myocyte. In addition, as a result of their continued stimulation, the betareceptors for norepinephrine are downregulated in heart failure, which further diminishes the function and functional reserve of the heart.
Management
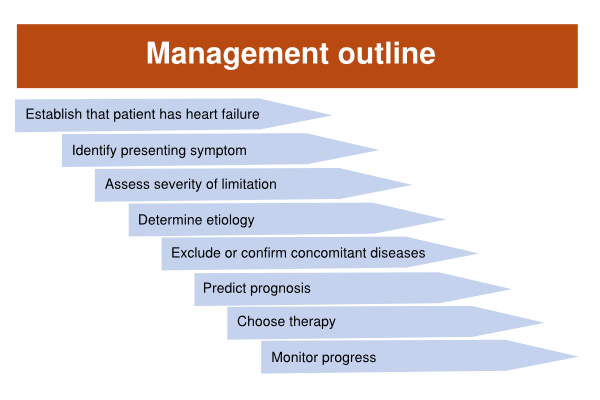
When a patient presents with symptoms of heart failure, it is worthwhile to have a dedicated diagnostic and therapeutic plan, in the order as indicated below (Figure 3.2.3). Clinical aspects are important for diagnosis, but the final diagnosis is only made after objective evidence of heart dysfunction.