1.17: Chemotherapy
- Page ID
- 10639
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Principles of Clinical Cancer Chemotherapy and Drug Resistance
Cancer Mortality: 2000 = 553,091; Est.2003 = 556,500
Cancer Chemotherapy -- Effectiveness by Disease
Curative
- Acute Lymphocytic Leukemia, Hodgkin’s Disease, Diffuse Histiocytic Lymphoma, Burkitt’s Lymphoma
- Testicular Cancer, Choriocarcinoma
- Wilms’ Tumor,* Ewing’s Sarcoma,* Embryonal Rhabdomyosarcoma*
Probably Curative
- Acute Myelogenous Leukemia
- Small Cell Lung Cancer, Breast Cancer,* Osteogenic Sarcoma*
Major Therapeutic Benefit (Short of Cure)
- Head and Neck Cancer, Cervical Cancer, Metastatic Breast Cancer, Ovarian Cancer
- Soft Tissue Sarcoma
- Nodular Lymphomas, Chronic Leukemias
- Insulinomas
Limited Effectiveness
- Lung Cancer
- GI Cancer
- Prostate Cancer
- Melanoma
* Adjuvant chemotherapy: Drugs administered after removal of all detectable disease.
First Order Kinetics
A given dose/unit time of chemotherapy will kill a constant percentage of cells, not a constant number. This means that the same dose which decreases the tumor burden from 106 to 103 cells will be needed to decrease the burden from 103 to 100 cells.
Assuming an initial tumor burden of 106 cells, a treatment which is 99.9% effective will still leave 103 cells untouched. Thus, treatment may eliminate clinical symptoms, but the tumor can recur. Treatment should aim for 10-1 cells or less remaining to ensure a high percentage of cures.
“Log-kill hypothesis”
- Dashed line = no treatment.
- Top solid line = moderate, infrequent dosing of chemotherapy which prolongs survival but results in recurrent symptoms and eventual death.
- Middle line = aggressive treatment. Cell kill exceeds regrowth and treatment is sufficiently long to sterilize tumor (patient is cured).
- Bottom line = primary tumor is surgically removed or debulked, and adjuvant chemotherapy is used to kill remaining occult tumor.
Host Toxicity
Therapeutic effects on tumor (solid line) and toxicity (broken line) are related to drug dose. Both curves are steep, and displacem ent of the toxicity curve to the right reflects the therapeutic index (median toxic dose/median effective dose) which is usually low for antitumor agents.

Selectivity
Normal bone marrow cell kill and recovery (solid line) are compared to tumor cell kill and recovery (broken line). Each chemotherapy course causes a similar destruction of normal bone marrow and tumor cells, Rate of recovery of normal bone marrow, however, is greater than that of tumor cells. Number of normal bone marrow progenitors does eventually decrease with continued therapy.

Combination Chemotherapy
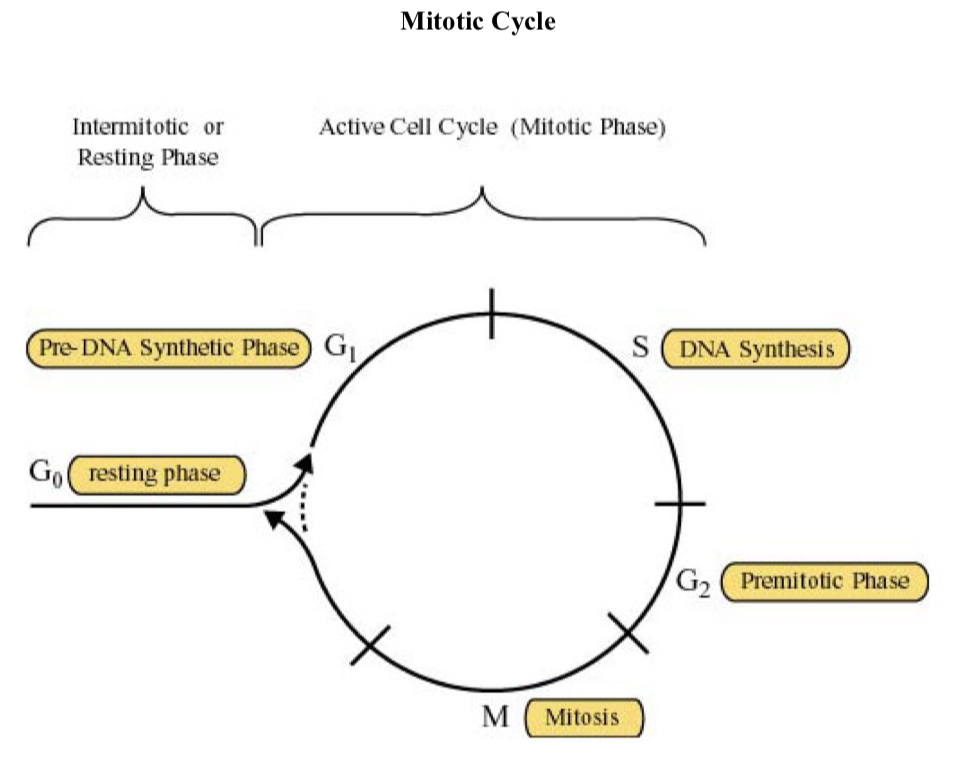
Combining drugs with different mechanisms of action and different dose-limiting toxicities can produce a bigger therapeutic effect at maximally tolerated doses of all drugs. Antitumor drugs may be placed into one of three classes based on the relationship of the effect to the mitotic cycle of the cell:
- Cell cycle active, phase specific
- Cell cycle active, phase non-specific
- Non-cell cycle active
Cell Cycle Active, S Phase Specific
ANTIMETABOLITES
Mechanisms
- incorporation of nucleotide analog in DNA or RNA, resulting in abnormal nucleic acids
- inhibition of certain enzymes involved in nucleotide biosynthesis
Examples:
- Pyrimidines
Uracil: 5-fluorouracil (5-fluoro-2’-deoxyuridine)
Thymine: 3’-azido-3’-deoxythymidine
Cytosine: Cytosine arabinoside; 5-azacytidine
- Purines
Adenine: 6-mercaptopurine
Guanine: 6-thioguanine
ANTIFOLS (METHOTREXATE)
Mechanism: competitive inhibition of dihydrofolate reductase, necessary for generation of methyl donors required for thymidine synthesis.

Toxicity (general)
- interfere with replication of all rapidly proliferating cells
- bone marrow --- myelosuppression
- GI mucosa ---- diarrhea, stomatitis
Toxicity (specific)
- 6-mercaptopurine --- cholestatic jaundice
- Methotrexate
renal – high doses may block tubules and cause acute renal failure
hepatic – usually seen with chronic daily administration of low doses (i.e., psoriasis treatment)
CNS – encephalopathy in patients given prior irradiation
Cell Cycle Active, G2/M Phase Specific
BLEOMYCIN
Mechanisms
- induces single-strand and double-strand DNA breaks
- selectivity for G2 phase, but cells in G1 can also be killed
Toxicity
- subacute or chronic pneumonitis
- little myelosuppression
PLANT ALKALOIDS: VINCRISTINE (VCR), VINBLASTINE (VBL), TAXOL, EPIDOPHYLLOTOXINS (VP-16, VM-26), CAMPTOTHECINS
Mechanisms
- Tubulin Binders
VCR, VBL inhibit polymerization of tubulin
Taxol blocks depolymerization; stabilizes microtubule - VP-16, VM-26 target topoisomerase II; non-intercalating
- Camptothecins (topotecan, irinotecan) inhibit topoisomerase I
Toxicity
- neurotoxicity
- paresthesias
- constipation
- decreased deep tendon reflexes
- myelosuppression
- SIADH (VCR, VBL)
Cell Cycle Active, Phase Non-Specific
ALKYLATING AGENTS
Mechanisms
- base alkylation resulting in DNA cross-linking
- single strand breaks
- double strand breaks and strand misreading
Examples:
- Nitrogen Mustard
- Cyclophosphamide
- Nitrosoureas
- Cis-platinum
- Busulfan
Toxicities (general)
- myelosuppression
- stomatitis
- nausea/vomiting
- alopecia
- impaired ovulation and spermatogenesis
- mutagenesis and carcinogenesis
Toxicities (specific)
- Cyclosphosphamide: hemorrhagic cystitis, bladder fibrosis, cardiotoxicity (reversible), SIADH
- Busulfan: interstitial pulmonary fibrosis
- Nitrosoureas: cumulative myelosuppression
- Platinum: acute tubular necrosis, ototoxicity
ANTHRACYCLINES
Mechanisms
- intercalate between strands of DNA double helix
- formation of drug free radicals
- inhibition of topoisomerase II
Examples:
- daunorubicin
- doxorubicin (Adriamycin)
Toxicities
- myelosuppression
- stomatitis
- cardiotoxicity (irreversible, dose-related)
Non Cell Cycle Active
CORTICOSTEROIDS
Mechanisms
- unclear –induce apoptosis of lymphoblasts and effective in lymphoid malignancies
- work via nuclear receptors
Examples
- prednisone
- dexamethasone
Toxicity
- typical steroid toxicity –relatively modest in this context
L-ASPARAGINASE (E. COLI, ERWINIA)
Mechanisms
- l-asparaginase converts asparagine to aspartate and NH3. Normal cells can reverse this process to form asparagine.
- Drug has activity in acute lymphocytic leukemia. Lymphoblasts lack asparagine synthetase and die without preformed asparagine in plasma.
Toxicity
- Hypersensitivity (urticaria, anaphylaxis)
- Pancreatitis
- Hepatotoxicity
Classification by Important Toxicity
- Renal - Acute Tubular Necrosis
- Platinum
- Streptozotocin
- Methotrexate
- Hepatic
- 6-Mercaptopurine (cholestatic jaundice)
- L-asparaginase (abnormal liver function tests)
- Anthracyclines (dependence on biliary excretion)
- Bladder (hemorrhagic cystitis)
- Cyclophosphamide
- Neurotoxicity (paresthesias)
- Plant alkaloids
- Pulmonary (interstitial fibrosis)
- Bleomycin
- Busulfan
- Nitrosoureas (high doses)
- Cardiac
- Anthracyclines (chronic cardiomyopathy)
- Cyclophosphamide (acute arrhythmias)
- Carcinogenesis
- Alkylating agents
- Procarbazine
- SIADH
- Vincristine
- Cyclophosphamide
Requirements for Combination Chemotherapy
- Several different drugs, each independently active against a given disease
- Each drug should have
- A different mechanism of action
- A different dose-limiting toxicity
- As a result:
- Each drug is given at full dose
- The rate of cell kill increases
- The chance of emergence of a drug-resistant clone decreases
Examples:
Combination Chemotherapy – ALL

Combination Chemotherapy: Other Curative Regimens
MOPP – Hodgkin’s Disease

M-BACOP – Diffuse Lymphoma

VBP – Testis

Adriamycin®= doxorubicin Oncovin®= vincristine
Tumor Host Resistance
- Changes in the tumor
- Location of tumor cells
- Pharmacologic sanctuary
- Blood supply to the anatomical region
- Extravascular distance for drug diffusion
- Drug metabolism by extracellular enzymes and normal cells that surround the tumor
- Effect of tumor size
- First order kinetics
- Penetration of drug
- Gradients of oxygen, nutrients
- Growth Characteristics
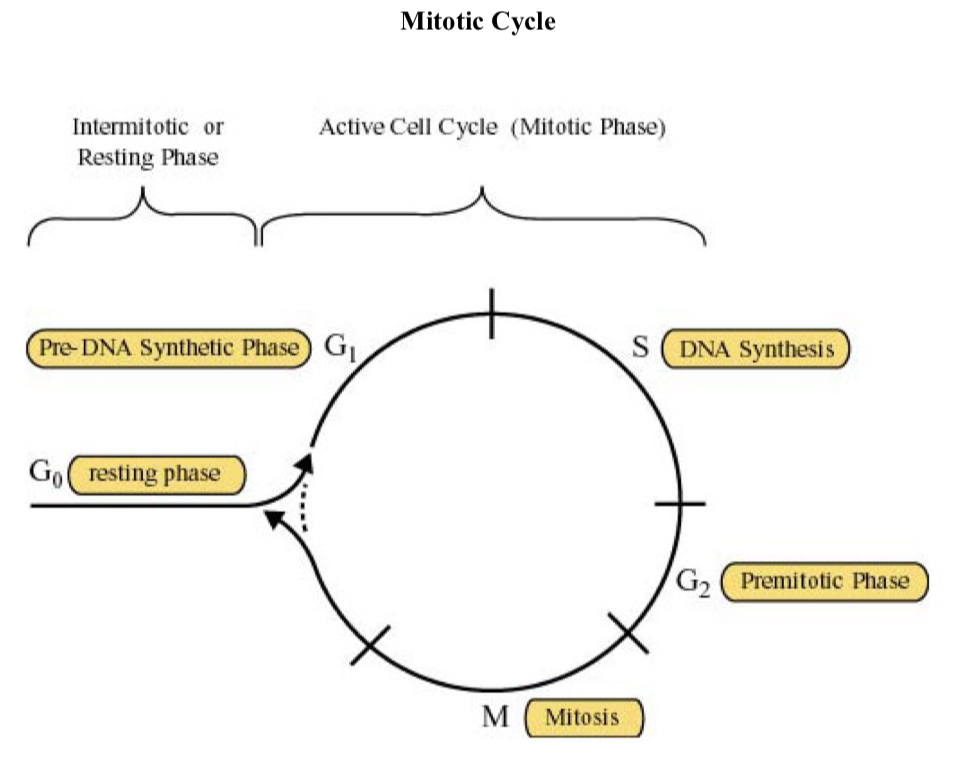
Mean volume doubling times for certain human tumors
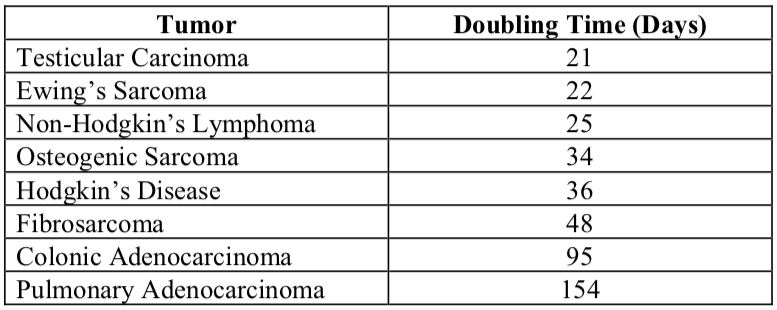
There is an inverse correlation between volume doubling time and response to chemotherapy (slower growth = worse response). Each bar in the graph below represents the average doubling time of a different human metastatic tumor:
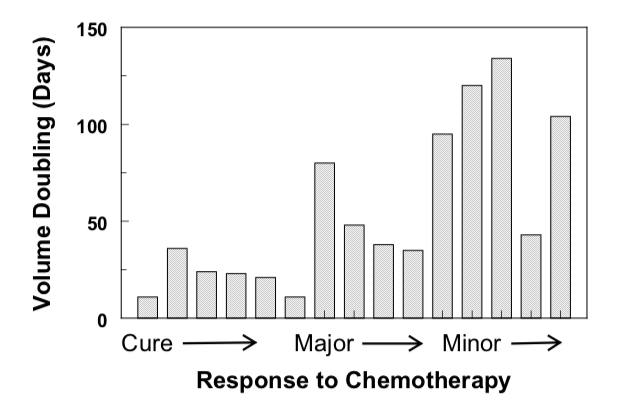
Gompertzian growth
Relationship between tumor size (A), growth fraction (B), and growth rate (C)
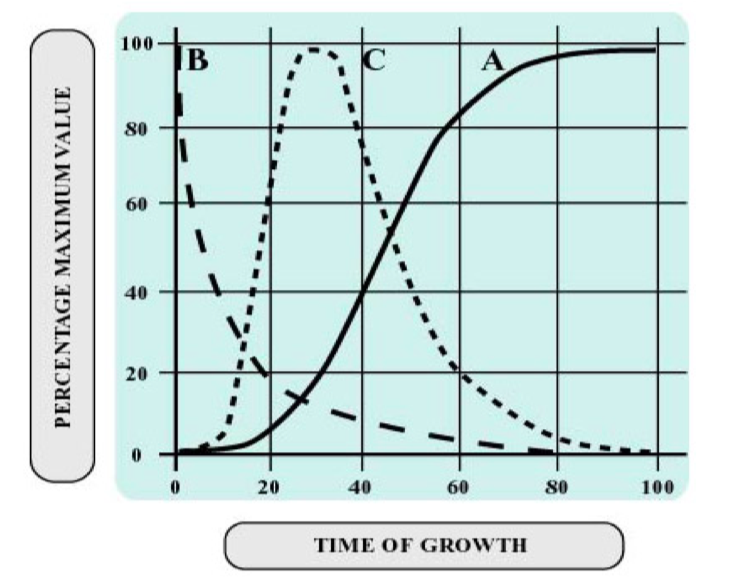
Although growth fraction is maximal at time of initiation of growth, the growth rate is maximal when the tumor is about 37% of its limiting size.
- Location of tumor cells
- Changes in the Host
- Altered absorption, distribution or excretion of a drug so that less reaches the tumor.
- Increased synthesis of enzymes from non-malignant cells which inactivate the drug.
- Increased sensitivity of normal tissues to the effect of a drug.
Cellular Resistance
- Natural Drug Resistance – lack of sensitivity of a tumor cell to drugs prior to therapy.
- Acquired Drug Resistance – genotypic and phenotypic changes during therapy that render a tumor cell insensitive to the lethal effects of a drug.
- Goldie-Coldman Hypothesis: the probability of selecting a single cell with resistance to a specific drug is related to both population size and mutation frequency. Drug exposure provides the pressure for selection of a resistant cell population.
- The frequency of drug resistant mutants is increased by antitumor agents which are also mutagens. Heidelberger et al. demonstrated that treatment with chemical mutagens and single-step selection results in the emergence of tumor cells resistant to fluoropyrimidines. The one-step selection following exposure to a mutagen may be relevant to the clinical use of combinations such as CMF.
- Mechanisms of Acquired Drug Resistance
- Decreased Expression of a gene product
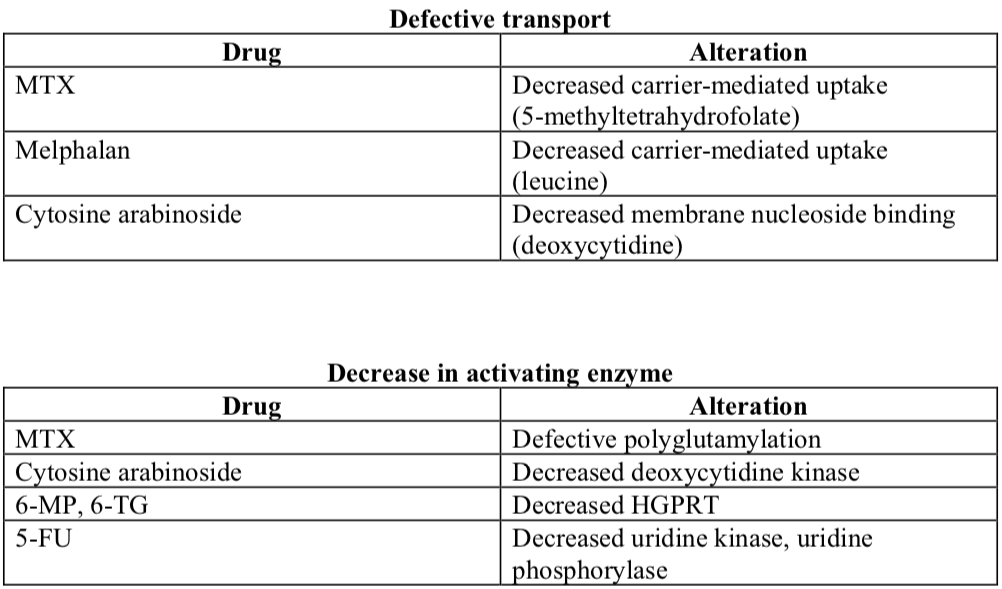
- Increased expression of a gene product
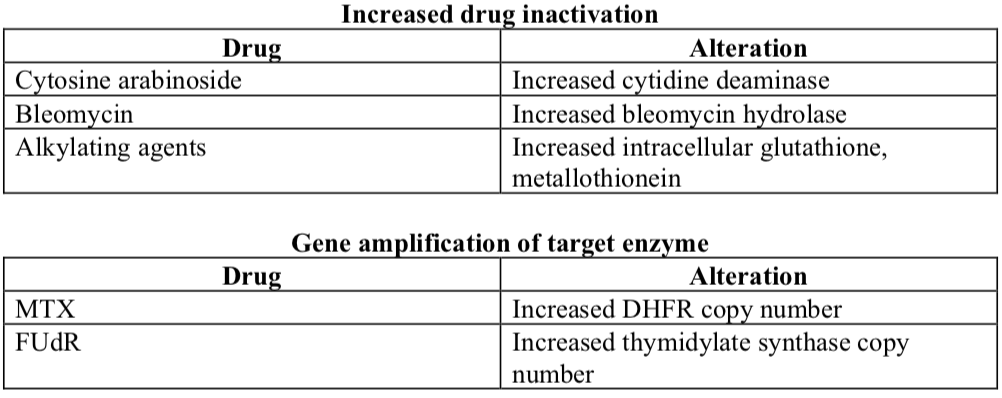
- Expression of an altered gene product

- Decreased Expression of a gene product
- Acquired Methotrexate Resistance
Acquired MTX resistance has been attributed to a variety of mechanisms. For example, the following have been identified in MTX-resistant sublines of a human squamous cell carcinoma (SCC15) established in culture by progressive dose escalation:
- Altered transport
- Defective polyglutamylation
- Polyglutamate derivatives (MTX-PGs) with 2 to 5 γ-linked glutamyl moieties (MTX-Glu2 to MTX-Glu5) are selectively retained by cells.
- MTX-PGs have a higher affinity for DHFR, cause prolonged inhibition of DNA synthesis and increase cytotoxicity.
- Increased production of DHFR (gene amplification)
- Abnormal homogeneous staining regions (HSRs): sites identified in MTX resistant cells which represent amplified DHFR genes on chromosome 2 (mouse) and 5 (human). HSRs are associated with stable resistance.
- Double minute chromosomes (DMs): small chromosomes of varying size without centromeres, usually occurring in pairs. These chromosomes do not segregate and therefore are lost during the process of cell division. Gene amplification on the double minute chromosome is thus unstable in the absence of selecting agents.
- Altered DHFR
- DHFRs in some resistant cells have a low affinity for MTX.
- An altered DHFR gene has a mutation in the codon for amino acid 22. This mutation (arginine for leucine) decreases both binding of MTX and function of the enzyme.
- Multidrug or Pleotropic Resistance
- Tumor cells exposed to a single drug develop cross-resistance to structurally unrelated compounds with different mechanisms of action. The affected drugs include a wide spectrum: anthracyclines, vinca alkaloids, actinomycin, podophyllotoxins.
- Resistant cells have an impaired ability to accumulate and retain drug. Drug efflux is probably more efficient.
- An over-expressed plasma membrane glycoprotein, designated the P- or permeability glycoprotein, with a MW of 170,000 daltons, is consistently found in multidrug- resistant human and animal cell lines, and in transplantable tumors.
- Drug resistance is related to the amount of P-glycoprotein
- Cells which regain drug sensitivity no longer express the membrane alteration.
- Transfer of DNA from drug-resistant cells confers multidrug resistance and plasma membrane glycoprotein expression.
- Transfer of multidrug resistance with a cDNA coding for the P-glycoprotein demonstrates that overexpression of this single gene is sufficient to confer the resistance phenotype.
- The P-glycoprotein or MDR1 gene is a member of a small family of genes. Not all members of this family confer the multidrug-resistant phenotype, thus suggesting that there may be functionally distinct classes of P-glycoprotein isoforms.
- Double minute chromosomes (DMs) and homogeneous staining regions (HSRs) are found in multidrug resistant lines. The degree of amplified DNA fragments correlates with the degree of drug resistance. The HSRs represent amplified P-glycoprotein genes and are reversible.
- The P-glycoprotein is comprised of 1280 amino acids with 12 hydrophobic segments that act as transmembrane domains. There are two similar domains with cytoplasmic sites that bind ATP. Both domains appear to be required for function. P-glycoprotein is primarily expressed on plasma membranes while smaller amounts have been detected in the ER and Golgi membranes.
- Vinblastine photoaffinity analogs bind to the P-glycoprotein, and binding is competitively antagonized by unlabeled vinblastine and anthracycline. The vinblastine protein complex is precipitated by a monclonal antibody to the P- glycoprotein. Moreover, vinblastine is transported by an ATP-dependent process through membranes that contain P-glycoprotein. These findings have established that the P-glycoprotein is a transporter molecule.
The P-glycoprotein is also homologous to bacterial transport proteins which are involved in ATP-dependent transport of specific molecules, particularly hemolysin, through the bacterial inner cell membrane.
- High levels of MDR1 gene expression have been found in liver, colon, small intestine, kidney, adrenal cortex and adrenal medulla. The P-glycoprotein is localized in a highly polar fashion on the bile canalicular surface of hepatocytes, the lumenal surface of the proximal tubule cells of the kidney, and on the lumenal mucosal surface of intestinal columnar cells. MDR1 RNA levels are usually high in those cancers derived from normal tissues which themselves have high MDR1 expression.
- Intrinsic multidrug resistance appears to be related to persistent expression of a gene involved in normal cellular function. Similar biochemical changes occur in multidrug resistant human breast cancer cells and in rat hyperplastic liver nodules that develop resistance to a wide variety of hepatotoxins (Solt Farber model). Mechanisms of de novo resistance to therapy in tumors associated with increased carcinogen exposure (colon, lung cancer) may therefore be similar to those associated with acquired resistance to anti-neoplastic agents.
- Drugs such as verapamil, diltiazem and quinidine have been found to overcome multidrug resistance in cell culture and in some animal experiments. For example, verapamil has been used to reverse adriamycin resistance in human ovarian cancer cells. Verapamil competes with vinblastine for binding, suggesting that drug binding to the P-glycoprotein is a necessary step in the process of drug resistance.
Other agents that reverse P-glycoprotein-mediated multidrug resistance include steroids and steroid antagonists (progesterone and tamoxifen) and reserpine. The most potent chemosensitizers are hydrophobic molecules with a basic nitrogen atom and two planar aromatic rings (termed the “pharmacophore”).
- Verapamil has been used clinically in an attempt to reverse multidrug resistance. A Phase I-II study failed to demonstrate a potentiation of doxorubicin therapy with verapamil in eight drug-resistant ovarian cancer patients. However, a more recent study has shown a therapeutic benefit for three of eight patients with multiple myeloma and non-Hodgkin’s lymphoma by adding a continuous infusion of verapamil to the VAD regimen. The three responding patients had P-glycoprotein positive tumors. Dose-limiting toxicity of verapamil was hypotension and cardiac arrhythmias. Myelosuppression was not increased in this trial. In this regard, in vitrostudies have demonstrated that doxorubicin cytotoxicity is not increased by verapamil in normal human marrow cells. Other clinical studies are underway using amiodarone and quinidine as inhibitors of P-glycoprotein mediated resistance.
- Acquired Resistance to Alkylating Agents
Prolonged exposure of human cells to alkylating agents has resulted in a maximum of 10- 15 fold resistance. This finding for alkylating agents is distinct from patterns of resistance seen with other chemotherapeutic agents. Alkylating agents therefore more closely resemble X-irradiation where significant resistance has not been demonstrated with repetitive treatment.
Reference
- Bast Fr. RC, Kufe DW, Pollack RE, Weichselbaum RR, Holland JF, Frei III E.: Cancer Medicine, 5th Edition. BC Decker, Inc., 2000


