2.3: Calories In Versus Calories Out
- Page ID
- 36817
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Discuss the principles that complicate correlating body weight to human health.
Describe the negative health impacts of weight loss dieting and weight cycling.
The ability to estimate energy expenditure and quantify calories consumed, has led to the simple conclusion that tracking or counting “calories in” compared to “calories out” will result in an easy way to manage body weight. This logic does not take into account the complexity and individuality of the human body. Human bodies are not static, meaning there are fluctuations from day to day in energy needs related to set point, sleep patterns, stress levels, activity levels, and eating patterns. Something as simple as the timing and macronutrient composition of meals, will impact the thermic effect of food, resulting in a change in energy expenditure.

Dieting Basics/ Dieting 101
The diet and weight loss industry is big business. In 2017, The U.S. Weight Loss and Diet Control Market reported a record $72 billion dollar value to the weight loss market.[1] This dollar amount is expected to continue to rise. At the same time, there is evidence that diets do not lead to long term weight loss for the majority of people. In observational studies, dieting was the best predictor of future weight gain and onset of obesity.[2][3][4] Meta-analysis and reviews of randomized clinical trials reported that on average, obesity treatments cause weight gain.[5][6] This additional weight gain leads to an increase in the set point, making it more difficult for an individual to lose weight in the future. Others reported a 3-5 % weight loss was possible 4 years later if participants continued all aspects of treatment.[7] For a 200 pound person, this represents a 6-10 pound weight loss. The health benefits of this modest weight loss are unclear and it is far less than what is expected or desired when following a diet. In conclusion, the diet industry makes money from a product that is proven not to work.
Dieting and Health
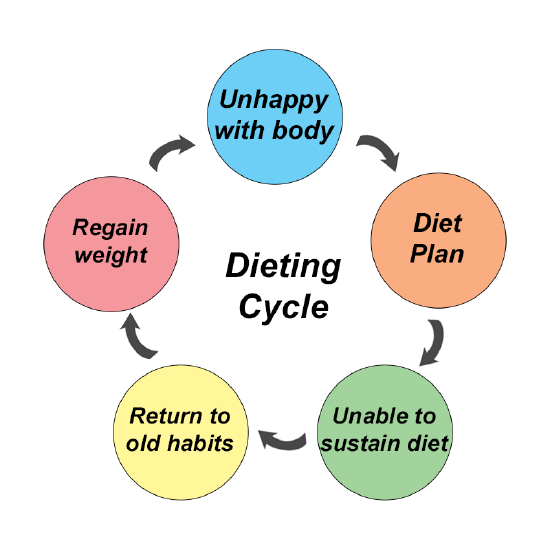
The scientific evidence shows that diets lead to modest weight loss for some and future weight gain for the majority of people. This often leads to a behavior called weight cycling or yo-yo dieting. The person continues to seek weight loss and a new diet, hoping to get a new result. This repetition of starting and stopping diets leads to losing and gaining a similar amount of weight over and over again. The weight goes up and down like a yo-yo. Yo-yo weight cycling is more harmful to health than being overweight at a stable weight. In addition, when someone cuts out food groups and restricts certain foods from their diet, the interest in the food increases. This in combination with intense hunger resulting from energy restriction, leads to a feeling of being out of control around foods and binge eating. To compensate for the feeling out of control, the person then restricts the food again and is then in a restriction/ binge or overeating cycle. [27]
The majority (up to 95%) of people regain the weight within three years and often gain back more.[8][9] Weight cycling puts stress on the body causing physical complications that are harmful, resulting in lowered or slowed metabolism, a reduction in lean body mass or muscle tissue, lowered body temperature, and increased risk for eating disorders.[10][11] Dieting and weight cycling also have a negative impact on mental health including lower self-esteem, and increases in depression, anxiety, irritability, and nervousness.[12] The evidence shows that dieting reduces both physical and emotional health.
Health and Body Weight
The assumption that health is determined by body weight, or a number on the scale, is outdated and not supported by science. As obesity rates continue to rise, it has been speculated that a higher Body Mass Index (BMI) stands alone as a health risk. However, there is substantial scientific evidence to support the notion that obesity in itself does not put an individual at increased risk of disease. The majority of epidemiological studies demonstrate that five pounds “underweight” is more harmful than 75 pounds “overweight”. [13][14][15][16][17] The results of multiple studies have indicated that using weight as a criterion for health is off-target and potentially harmful.[18][19][20] This suggests that it is not possible to tell how healthy an individual is simply by looking at them or calculating their BMI.

The following are measurable risk factors and markers of health that are not connected to body weight. These are good targets for nutrition education and counseling and ways to monitor improvements of health status over time.
- Biomarkers: blood pressure, blood glucose, total cholesterol, high-density lipoproteins, low-density lipoproteins, triglycerides
- Regular movement/ activity/ exercise
- Stress and inflammation
- Hormone balance
- Mental health status
- Sleep
- Quality of life
- Connection to the community
- Spiritual health
- Intellectual health
- Occupational health
References
- The U.S. weight loss & diet control market. (2019). Marketdata LLC. https://www.researchandmarkets.com/research/qm2gts/the_72_billion?w=4↵
- Neumark-Sztainer, D., Wall, M., Story, M., & Standish, A. R. (2012). Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. The Journal of Adolescent Health, 50(1), 80–86. ↵
- Neumark-Sztainer, D., Wall, M., Guo, J., Story, M., Haines, J., & Eisenberg, M. (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106(4), 559–568. ↵
- Stice, E., Cameron, R. P., Killen, J. D., Hayward, C., & Taylor, C. B. (1999). Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology, 67(6), 967–974. ↵
- Mann, T., Tomiyama, A. J., Westling, E., Lew, A.-M., Samuels, B., & Chatman, J. (2007). Medicare’s search for effective obesity treatments: Diets are not the answer. The American Psychologist, 62(3), 220–233. ↵
- Ayyad, C., & Andersen, T. (2000). Long-term efficacy of dietary treatment of obesity: A systematic review of studies published between 1931 and 1999. Obesity Reviews, 1(2), 113–119. ↵
- Franz, M. J., VanWormer, J. J., Crain, A. L., Boucher, J. L., Histon, T., Caplan, W., Bowman, J. D., & Pronk, N. P. (2007). Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. Journal of the American Dietetic Association, 107(10), 1755–1767. ↵
- Mann, T., Tomiyama, A. J., Westling, E., Lew, A.-M., Samuels, B., & Chatman, J. (2007). Medicare’s search for effective obesity treatments: Diets are not the answer. The American Psychologist, 62(3), 220–233. ↵
- Wooley, S. C., & Garner, D. M. (1994). Dietary treatments for obesity are ineffective. BMJ, 309(6955), 655–656. ↵
- Bacon, L. (2010). Health at every size: The surprising truth about your weight. BenBella Books, Incorporated. ↵
- Karelis, A. D., Messier, V., Brochu, M., & Rabasa-Lhoret, R. (2008). Metabolically healthy but obese women: Effect of an energy-restricted diet. Diabetologia, 51(9), 1752–1754. ↵
- French, S. A., & Jeffery, R. W. (1994). Consequences of dieting to lose weight: Effects on physical and mental health. Health Psychology, 13(3), 195–212. ↵
- Flegal, K. M., Graubard, B. I., Williamson, D. F., & Gail, M. H. (2005). Excess deaths associated with underweight, overweight, and obesity. JAMA, 293(15), 1861–1867. ↵
- Flegal K.M., Graubard B.I., Williamson D. F., & Gail M. H. (2018, March). Excess deaths associated with underweight, overweight, and obesity: An evaluation of potential bias. Vital & Health Statistics. 42, 1-21 ↵
- Orpan H. M., Berthaelot J. M., Kaplan M. S. , Feeny D. H., McFarland B., & Ross N. A. (2010). BMI and mortality: Results from a longitudinal study of Canadian adults. Obesity (Silver Springs). 18(1), 214-8. ↵
- Tamakoshi A., Hiroshi Y., Lin Y., Tamakoshi K., Kondo T., Suzuki S., Yagyu K., Kikuchi S., & the JACC Study Group (2010). BMI and all-cause mortality among Japanese older adults: Findings from the Japan collaborative cohort study. Obesity. 18(2), 362-9. ↵
- Campos P. (2004). The Obesity Myth. Gotham Books. ↵
- Kang X., Shaw L. J., Hayes S. W., Hachamovitch R., Abidov A., Cohen I., Friedman J. D., Thomson L. E., Polk D., Germano G., & Berman D. S. (2006). Impact of body mass index on cardiac mortality in patients with known or suspected coronary artery disease undergoing myocardial perfusion single-photon emission computed tomography. Journal of the American College of Cardiology. 47(7), 1418-26 ↵
- Oreopoulos A., Padwal R., Kalantar-Zadeh K., Fonarow G. C., Norris C. M., & McAlister F. A. (2008). Body mass index and mortality in heart failure: A meta-analysis. American Heart Journal. 156(1), 13-22. ↵
- Olsen T. S., Dehlendorft C., Petersen H. G., & Andersen K. K. (2008). Body mass index and prestroke mortality. Neuroepidemiology. 30, 93-100. ↵
- Association for Size Diversity and Health. (2020). HAES Principles. http://www.sizediversityandhealth.org↵
- Bacon L., Stern J. S., Van Loan M. D., & Keim N. L. (2005). Size acceptance and intuitive eating improve health for obese female chronic dieters. Journal of the American Dietetic Association. 105(6), 929-36. ↵
- Ulukau Hawaiian Electronic Library. wehewehe.org/↵
- The Original Intuitive Eating Pros. (2007 - 2019). 10 Principles of Intuitive Eating. https://www.intuitiveeating.org/10-principles-of-intuitive-eating/↵
- Schaefer J. T., Magnuson A. B. (2014). A review of interventions that promote eating my internal cues. Journal of the Academy of Nutrition and Dietetics. 114(5), 734-760. ↵
- Van Dyke N., Drinkwater E. J. (2014). Relationships between intuitive eating and health indicators: Literature review. Public Health Nutrition. 17(8), 1757-1766. ↵
- Parker, Libby (2019). Permission To Eat: a practical guide to working yourself out of an eating disorder during college, while celebrating the awesomeness that is you!

