5.6: Nasolabial Flaps for Oral Cavity Reconstruction
- Page ID
- 15459
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY
NASOLABIAL FLAP FOR ORAL CAVITY RECONSTRUCTION
Harry Wright, Scott Stephan, James Netterville
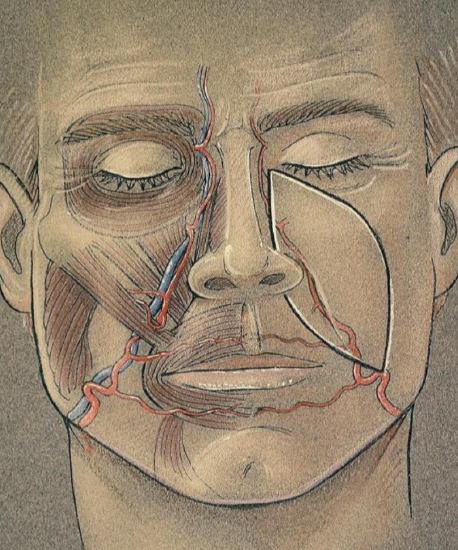
Figure 1: Relationship of the facial artery to the design of the nasolabial flap
Designed as a true myocutaneous flap pedicled on the facial artery, the nasolabial flap is a robust and versatile flap that is well suited to single-stage reconstruction of oral cavity defects or to staged reconstructions of facial defects (Figure 1). This chapter will focus on oral cavity reconstruction. The redundant skin extending from the medial canthus of the eye to the inferior margin of the mandible (nasolabial sulcus and nasofacial groove) defines the donor site for the nasolabial flap. This area is relatively hairless except for the lower cheek in males, an important consideration in oral cavity reconstruction. The flap itself is comprised of skin, subcutaneous tissue and the underlying musculature.
Surgical Anatomy
Blood Supply

Figure 2: The facial artery displayed in a cadaver dissection, showing the more common medial course
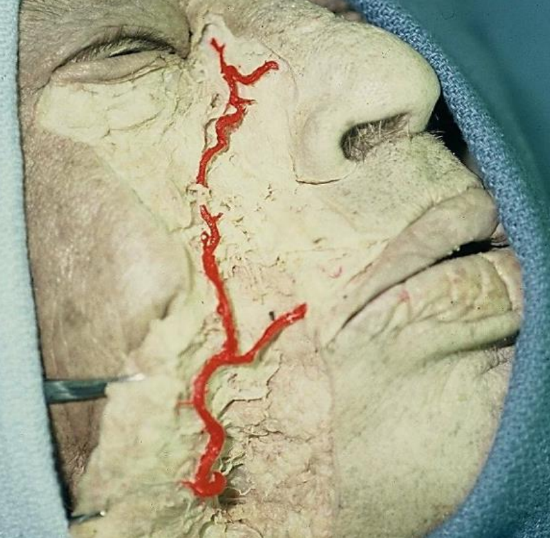
Figure 3: Cadaver dissection showing a less common lateral course of the artery
The subdermal plexus is supplied by feeder vessels from the branches of the facial artery and provides the blood supply to the nasolabial muscle and skin. This allows for high viability and permits bold thinning and shaping. The facial artery has four main branches in the face: the inferior labial artery, superior labial artery, alar artery and lateral nasal artery, and terminates as the angular artery. In a majority of dissections, the facial artery takes a medial course as shown in Figures 1 & 2, rather than a lateral course as shown in Figure 3 (unpublished data). The artery resides in the dense fibrous tissue at the oral commissure and continues along the superior border of the upper lip to the nasal ala. It then continues in a medial course along the nasofacial groove toward the medial canthus of the eye. Arterial perforators are especially concentrated in the inferior two-thirds of the nasolabial groove.
When raising a laterally-pedicled flap, as is often the case in single-stage oral cavity defect reconstructions, incorporation of the lower one-third of the nasolabial groove is essential to ensure a robust vascular musculocutaneous base.
Muscle
The relevant musculature is best understood as it relates to the facial artery. The facial artery is deep to the platysma, risorius, zygomaticus major and minor, levator labii superioris, and levator labii superioris alaeque nasi muscles. The artery is superficial to the mandible, buccinators muscle, and levator anguli oris muscle. The position of the artery deep to the majority of facial mimetic muscles suggests that the nasolabial flap may incurporate this muscle layer and be developed as a true musculocutaneous flap.
Surgical Technique
Flap design
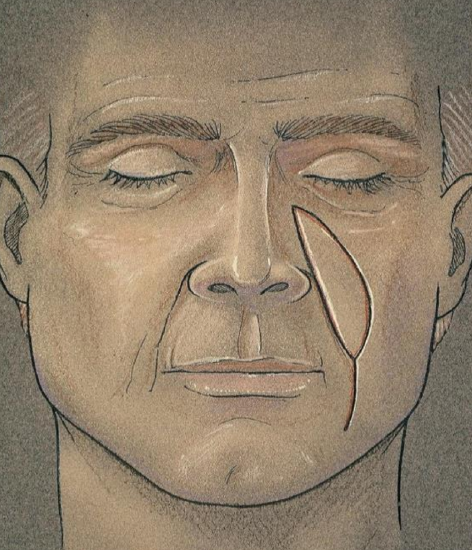
Figure 4: Approximate dimensions of the nasolabial flap
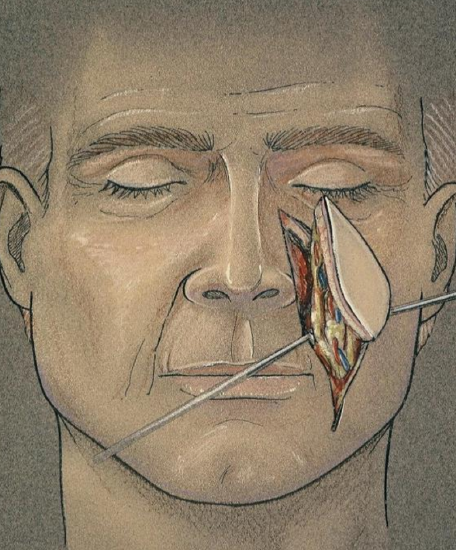
Figure 5: Illustration demonstrating the the laterally based pedicle
A fusiform flap is marked ensuring that the medial border of the flap is on the nasofacial groove (Figures 1, 4, 5). A pencil Doppler probe may be useful to locate and delineate the course of the artery. Average flap dimensions are 2.5 cm in width and 6 cm in length. The width may be closer to 5 cm when the facial skin is very redundant. The superior border of the flap is inferior to the medial canthus along the nasofacial junction. Placement of the inferior border depends on the nature of the defect. For floor of mouth reconstruction, the inferior border of the flap should be at the superior border of the mandible; reconstruction of palatal defects, however, requires the inferior border to be approximately at the level of the oral commissure.
Flap harvest
The skin incision is carried through the dermis and subcutaneous fat to the level of the underlying musculature. As shown in the anatomic dissections above and below, the artery lies in a plane deep to the facial mimetic musculature and in a medial position along the nasofacial groove. The flap is elevated in a superior-to-inferior fashion in a plane deep to the facial musculature, artery and vein, with the artery identified carefully by blunt dissection. The parotid duct is identified and preserved. The superior labial artery may require ligation.
Inset

Figure 6: The flap is narrowly pedicled on the facial artery, and then is tunneled via the buccal space into the oral cavity
Thus a musculocutaneous flap is developed and pedicled on the facial artery (Figures 5, 6, Case #6). The flap is then tunneled through the buccal space to repair the intraoral defect, as shown in Figure 6 and in several cases below. If single-stage reconstruction is the goal, the tunneled segment of the flap must be de-epithelialized. Staged reconstruction with delayed division of the pedicle may be performed, with the delay necessary to ensure adequate neovascularization.
Donor site closure
The donor site is irrigated prior to layered closure with 4‐0 Vicryl providing deep dermal closure and 5-0 fast absorbing catgut sutures to approximate the skin edges. The closure should advance the lateral skin flap in a superior and medial direction to avoid distortion of the lower eyelid.
Clinical Applications & Selected Cases
A nasolabial flap is suited to reconstructing small-to-medium oral cavity defects including, but not limited to alveolus (Case #1), floor of mouth (Cases #2, #3), buccal cavity (Case #4) and palate (Cases #5, #6).
Case #1: Superior alveolus reconstruction

Figure 7: Tumor of superior alveolus

Figure 8: Alveolectomy defect
This superior alveolus tumor was resected by superior alveolectomy. A lip-split approach was utilized for resection and to facilitate the reconstruction (Figures 7, 8).

Figure 9: Nasolabial flap being designed and raised

Figure 10: Flap turned in to reconstruct the defect

Figure 11: Nasolabial flap inset into the defect and donor site and lip-split closed
A nasolabial flap was designed, raised and turned in to reconstruct the defect (Figures 9-11).

Figure 12: Wound closure and final result
Figure 12 illustrates a Penrose drain left in a dependent portion of the donor site; and a postoperative image showing the donor site and accessory incisions to be well healed.
Case #2: Mouth floor reconstruction

Figure 13: Defect following resection

Figure 14: Outline of flap

Figure 15: Facial artery is bluntly dissected

Figure 16: Flap inset into floor of mouth
This floor of mouth cancer resection resulted in an alveolar ridge, gingiva, and floor of mouth defect; the inferior border of the defect is at the level of the superior border of the mandible (Figure 13). The defect was reconstructed with a nasolabial flap (Figures 14-16).
Though the flap is hairless in the image shown, the surgeon must anticipate the implications of transferring hair‐bearing skin intraorally.
Case #3: Mouth floor reconstruction

Figure 17: The robust nasolabial flap minimizes the risk of ankyloglossia
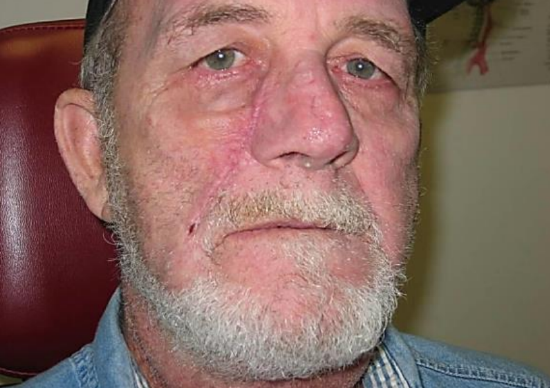
Figure 18: Early postoperative image shows aesthetically acceptable appearance of donor site

Figure 19: Later image shows a well-healed floor of mouth reconstruction

Figure 20: Though the right upper lip is paralyzed, the concomitant lip lift provided by the harvest of nasolabial donor skin aids with symmetry at rest
Figures 17-20 illustrate the postoperative results of reconstruction of an anterior floor of mouth defect crossing the midline.
Case #4: Buccal cavity reconstruction

Figure 21: Buccal defect

Figure 22: Flap inset into buccal defect

Figure 23: Healed flap in buccal defect
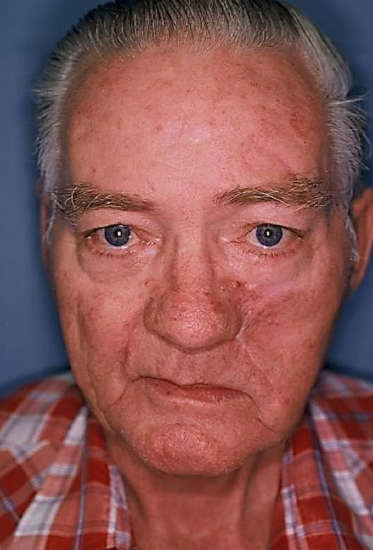
Figure 24: Final cosmetic result
The robust blood supply to the nasolabial flap permits shaping of the flap to precisely fill the defect (Figures 21-24).
Case #5: Palate reconstruction (postoperative)

Figure 25: Healed palatal defect
Figure 25 demonstrates a healed palatal reconstruction, with an implant visible for a dental prosthesis.

Figure 26: Excellent camouflage of scar and facial symmetry at rest

Figure 27: Asymmetry with smiling
Reconstruction of palatal defects requires that the inferior border of the incision be approximately at the level of the oral commissure. Note the excellent camouflaging of the scar and the facial symmetry at rest (Figure 26). When smiling the patient demonstrates the expected paralysis of the ipsilateral upper lip which is generally well-tolerated (Figure 27); this adverse outcome is further discussed below.
Case 6: Bilateral nasolabial flaps
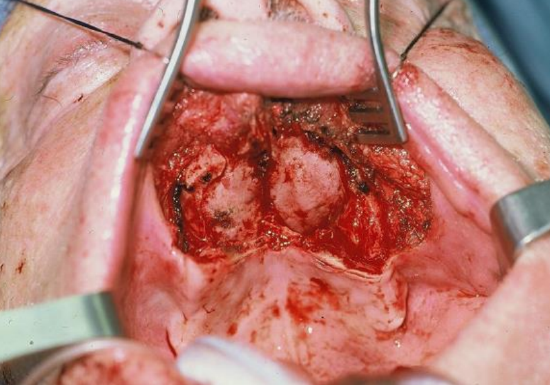
Figure 28: Defect of hard palate, alveolus and gingivobuccal sulcus

Figure 29: Bilateral nasolabial flaps
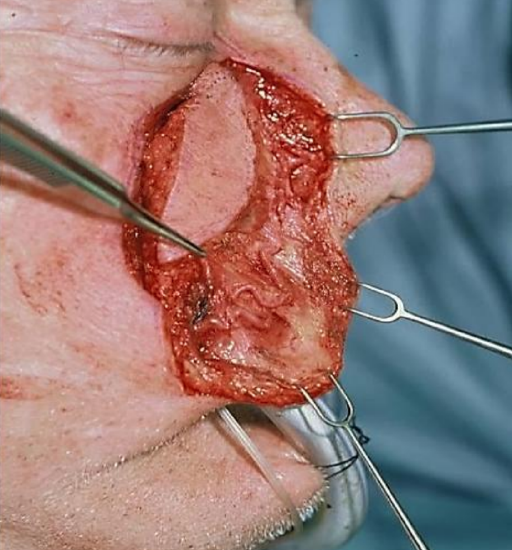
Figure 30: Angular artery visible
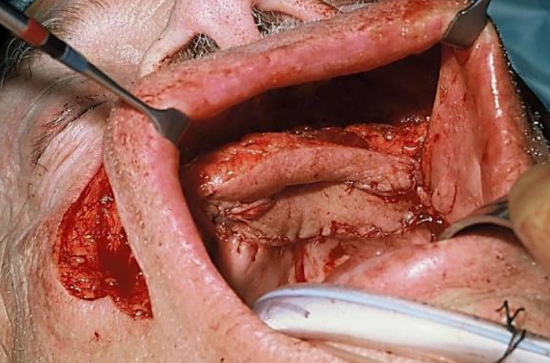
Figure 31: Flap being inset in a side-by-side configuration
This patient has a large defect of the hard palate, alveolus and gingivobuccal sulcus (Figure 28). Bilateral nasolabial flaps were raised (Figure 29). In Figure 30 the terminal branch of the facial artery i.e. the angular artery, is demonstrated.
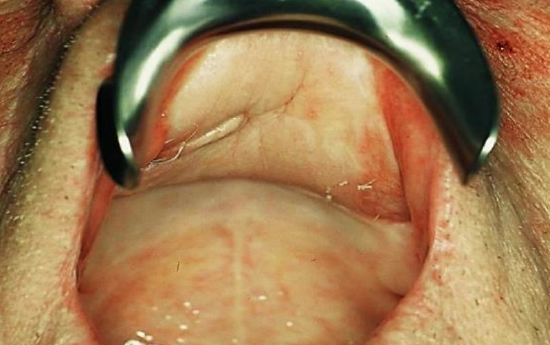
Figure 32: Healed palatal reconstruction

Figure 33: Healed facial scars
Postoperative images show well-healed donor sites and intact and symmetric elevation of the corners of the mouth i.e. intact cranial nerve VII (Figures 32, 33).
Adverse Outcomes
Upper lip weakness
Upper lip weakness may result if the terminal buccal branches of the facial nerve supplying lip elevators are lysed or if the principle lip elevators (zygomaticus major/minor, levator labii alique nasi, levator anguli oris) are completely divided. Muscle disruption may occur when extensive mobilization and rotation of the flap is required.
A unilateral nasolabial flap typically does not result in any appreciable ipsilateral lip weakness. As a correlation, deinnervated Abbe flap reconstruction of the upper lip has been shown on electromyography (1 and 5 years post-op) to regain 80 and 100% reinnervation of the transposed muscle segment.1 However, extensive disruption of innervation and mimetic muscle integrity during harvesting of bilateral nasolabial flaps may result in clinically appreciable weakness of the upper lip. Though permanent, it is usually well tolerated. As shown in the selected cases above, the resulting upper lip weakness is mitigated by the mild lip lift provided by closure of the donor site.
Oral competence
Bilateral upper lip weakness and numbness could significantly impair oral competence, especially lip-pursing, and must be considered if bilateral nasolabial flaps are planned. Special care should be taken to avoid disruption of the distal facial nerve branches in such cases.
Summary
Nasolabial flap reconstruction of intraoral defects is a well-recognized technique. Because the flap is pedicled on the facial artery, single-stage closure with a smaller pedicle may be achieved if the proximal portion of the flap is de-epithelialized. A robust blood supply helps to ensure flap viability and prevents flap breakdown and fistula formation even in adverse conditions of excess tension or mild compression of the transbuccal pedicle. The bulk provided by the facial musculature helps to fill larger defects. It does not impair speech and causes only minimal donor site morbidity. The flap is not overly time-consuming or technically difficult to master; however, knowledge of the relevant anatomy is essential.
References
Burget G, Menick F. Aesthetic restoration of one-half of the upper lip. Plast Reconstr Surg. 1986;78(5):583–93
Acknowledgements
- Illustrations by Paul Gross
- Cadaver dissections by David Haynes, MD FACS
Other flaps described in The Open Access Atlas of Otolaryngology Head & Neck Operative Surgery
- Pectoralis major flap
- Buccinator myomucosal flap
- Buccal fat pad flap
- Temporalis muscle flap
- Deltopectoral flap
- Paramedian forehead flap
- Upper and lower trapezius flaps
- Cervicofacial flaps
- Submental artery island flap
- Supraclavicular flap
- Latissimus dorsi flap
- Local flaps for facial reconstruction
- Radial free forearm flap
- Free fibula flap
- Rectus abdominis flap
- Anterolateral free thigh flap
- Thoracodorsal artery scapular tip (TDAST) flap
- Principles and technique of microvascular anastomosis for free tissue transfer flaps in head and neck reconstructive surgery
Authors
Harry V. Wright MD, MS
Fellow
Facial Plastic and Reconstructive Surgery
Otolaryngology and Head & Neck Surgery
University of South Florida, USA
dr.hvwright@gmail.com
Scott Stephan MD
Assistant Professor
Facial and Plastic Surgery
Vanderbilt Bill Wilkerson Center
Nashville, TE, USA
stephan@vanderbilt.edu
James L. Netterville MD
Director of Head and Neck Surgery
Vanderbilt Bill Wilkerson Center
Nashville, TE, USA
james.netterville@vanderbilt.edu
Editor
Johan Fagan MBChB, FCS(ORL), MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
johannes.fagan@uct.ac.za


